Keywords
INTRODUCTION
Despite prevention initiatives, atherosclerosis continues to be responsible for increased adult morbidity and mortality in the Western world, reaching epidemic proportions in technologically developed societies. This well-documented process begins very early in life with progressive vascular modification and cholesterol deposits in the intima of large arteries, although this is not manifested clinically until adulthood.1-5
The main cardiovascular risk factors (CVRF) favoring pediatric atherogenic development are known. The most relevant are overweight and, particularly, obesity, which are reaching dramatically rising prevalence levels in Western societies and especially in Spain.6-11 This problem, of an evidently nutritional nature, entails complications such as arterial hypertension, dyslipidemia, diabetes, metabolic syndrome, hepatic steatosis, biliary disease, and orthopedic disorders, as well as respiratory and psychological problems. These comorbidities, which were once characteristic of adults, are now being detected at alarmingly rising frequencies in children at an increasingly early age.11,12
Other cardiovascular risk groups of children are carriers of familial dyslipidemia, especially those with a serum lipid profile with high levels of low density lipoprotein cholesterol (LDL-C) and low hight density lipoprotein cholesterol (HDL-C). Also considered at risk are healthy children who have extensive family history of cardiovascular disease and premature death (men <55 years and women <65 years).13
Information available on the topic supports the hypothesis that preventive intervention should begin as soon as possible, ie, in the early years of life; therefore, it of great clinical interest to have a noninvasive method with which to detect vascular injury in the subclinical phase, particularly at the onset of endothelial dysfunction and/ or during the first histological changes. In this respect, several ultrasound techniques have been developed in recent years, which aim to assess the degree of arterial involvement in subjects suffering from CVRF.14-17 Some studies have assessed morphologic changes to the arterial wall by measuring the intima-media thickness (IMT) of the carotid artery, linking its gradual increase with the severity and extent of coronary artery disease and stroke.18-22 Later works have concluded that this assessment can only provide a local or at the most regional estimation of the vascular wall under examination and propose the use of high-resolution and ultrasound techniques to assess the functional changes in arterial elasticity caused by atherosclerosis. Most of these studies have been conducted in adults and concluded that increased arterial hardening by arteriosclerosis, is a good predictor of cardiovascular events, independent of classic factors.16,23-25 Furthermore, endothelial dysfunction is thought to occur with atherosclerosis, probably related to local inflammation, suggesting that CVRF exert a deleterious effect on arterial elasticity through endothelial dysfunction.26
Under these circumstances we propose that having a functional marker of vascular damage that precedes structural changes would enable preventive measures to be taken at the sub-clinical stage. Therefore our goal was to analyze several indices of arterial-wall stiffness of the common carotid artery using high-resolution Doppler ultrasonography, in children and adolescents with CVRF, to assess its usefulness as an earlier marker of vascular damage as compared to the first structural changes reflected in IMT.
METHODS
Patients
A case-control study was conducted (June 2008-December 2009) in schoolchildren and adolescents aged 8-16 years with CVRF (obesity and dyslipidemia) referred by a primary care pediatrician to the Pediatric Gastroenterology and Nutrition Unit of Hospital Clínico Universitario de Valencia. Patients were recruited from 10 health care centers (Number Area 5 of the Department of Health in Valencia) whose referral hospital is the Hospital Clinico Universitario de Valencia, Spain. Selection was at random and patients presenting dysmorphic syndromes and/or with endocrine disorders were excluded. A control group of children with no CVRF, matched by age and sex was also included in the study (referred from the same health centers for studies of functional murmurs or preoperative study prior to minor surgery). Children were included in the study after the informed consent of a guardian was given. The study protocol was approved by the hospital's Committee on Ethical Practice.
Clinical Evaluation
For each patient the following data were recorded: a) family history of cardiovascular risk (overweight, obesity, metabolic syndrome, type 2 diabetes mellitus, primary arterial hypertension, inherited, and acquired dyslipidemia, cardiovascular incidents in men <55 years and women <65 years old); b) personal history and growth curve; c) nutritional assessment: anthropometric measurements (weight and height) were collected using a standardized technique; to compare children of different ages and sex, the z-score was calculated for each measurement with reference to WHO standards 200727; to define obesity, the body mass index (BMI) Z-score was calculated and subjects were considered obese when it was ≥2SD, equivalent to a BMI of 30 kg/m2 at the age of 1927-29; d) arterial pressure, always measured by the same researcher using the same measuring apparatus (Dinamap® oscillometric method); high values were checked with the auscultatory method and mercury sphygmomanometer; measurements were taken from the right arm with the child sitting comfortably; the sleeve was placed at the level of the heart, adjusting the size to fit the diameter of the arm; 3 measurements were taken for each child and the average of the 3 were calculated; the values for each child were compared with reference tables according to sex, age, and height (The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents).30
Biochemical Analyses of Plasma
Total cholesterol was determined along with fractions and triglycerides. Dyslipidemia was diagnosed when total cholesterol and LDL-C values were above the 95th percentile for age and sex, with/ without HDL-C <35 mg/dL, and triglycerides were above the 95th percentile.31
High-Resolution Ultrasound Measurement of Arterial Stiffness and Intima-Media Thickness
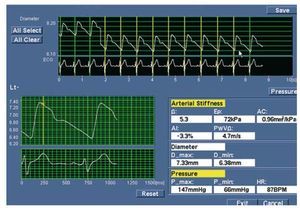
An Aloka alfa-10 ultrasound apparatus was employed using EchoTracking®. Measurements were taken of the right common carotid artery, 1 cm below the carotid bulb, with the patient in supine position, head turned 45 degrees to the left and an ambient temperature of 22-25ºC, as described previously.32 The common carotid artery was chosen because it is a central artery, branching directly from the aorta. The patient remained in the supine position for at least 5 minutes before starting the examination. The transducer was positioned so that the carotid artery could be observed longitudinally and was tilted to maximize the echoes from the interface between the medium and adventitia. When this line of division was captured clearly, the 2 system tracers were placed on the diametrically opposed interface points. Once in place, these tracers were oscillated with the arterial wall, thus recording the temporal distance between the two. Patient monitoring by ECG continued throughout the examination so that the system could detect the onset of the pulse wave. Using this technique we recorded (Figure 1): a) graphic chart of the pulse wave; b) maximum or systolic arterial diameter (Ds) corresponding to the peak of each pulse and representing the point at which the blood vessel is subjected to highest pressure (systolic blood pressure [SBP]); c) minimum or diastolic arterial diameter (Dd) corresponding to the lowest point, when the pressure to which the blood vessel is subjected is minimum (diastolic blood pressure [DBP]). All measurements were performed by the same researcher.
Figure 1. Results windows. Top: pulse wave and electrocardiogram. Bottom right: calculated parameters of arterial stiffness in one of the patients. b indicates stiffness parameter; Ep, pressure-strain elasticity modulus; AC, arterial compliance; AI, augmentation index; PWV, one-point pulse wave velocity; D_max, maximum arterial diameter; D_min, minimum arterial diameter; P_max, systolic blood pressure; P_min, diastolic blood pressure; HR, heart rate
After the 3 measurements of blood pressure had been taken, the average of both SBP and DBP were calculated and recorded in the EchoTacking program, assuming the arterial pressure at the level of the brachial artery was the same as that of the carotid. Once all data were recorded, the program implemented a series of equations to calculate the 5 parameters related to arterial wall elasticity:
- Arterial compliance (AC): π (Ds2-Dd2)/ 4(SBPDBP). Units: mm2/kPa
- Pressure-strain elasticity modulus (Ep): (SBPDBP) Dd/ (Ds-Dd). Units: kPa
- Stiffness index (β): ln (SBP-DBP)/ [(Ds-Dd)/ Dd].
- One-point PWV (PWV): Distance/ Δt. Units: m/s
Augmentation index (AI): (D2 - D1) 100/(Ds-Dd). Units: as a percentage
The IMT was measured at the same point specified for functional examination, determining the thickness in the carotid far wall, according to the criteria established by Mannheim.33 The images were recorded digitally and measured again manually. The mean of 3 measurements was obtained, as well as the maximum value; both were analyzed.
Statistical Methods
Sample size was calculated using the Ene 3.0 program (Statistical Department, University of Barcelona, Spain and Department of Biometry, GlaxoSmithKline®). The results of an initial pilot study on PWV and also on Ep were taken as a reference. For both, sample size should be between 23-25 subjects per group.
Statistical processing was performed with SPSS version 15. The results were expressed as mean and standard deviation. Continuous variables were compared using the Student t test. The relation ship of BMI, arterial pressure, LDL-C, HDL-C, and triglycerides with arterial stiffness parameters and IMT was studied using the Pearson correlation coefficient. For all studies, P<.05 was considered statistically significant.
RESULTS
The sample included a total of 99 children aged between 8 and 16 years (62 boys and 37 girls, 63% and 37%, respectively), distributed into 2 groups: a) study group of 65 children with CVRF of which 45 were obese and 20 had familial dyslipidemia; and b) controls: 34 children without disease who did not have any CVRFs, matched to the study group by age and sex.
Table 1 summarizes anthropometric results, blood pressure and lipid values of the 3 groups, and the differences between them. In obese children, 5 patients had LDL-C levels over 130 mg/dL, and 3 had HDL-C levels below 35 mg/dL, with HDL-C levels significantly lower than in the controls and the dyslipidemic patients (P<.001) and triglyceride levels significantly higher than in the controls (P<.01). Four patients showed arterial hypertension; the rest had normal values but on average these values were significantly higher than in the controls.
In the dyslipidemic group, all patients were normotensive, with values similar to those of the control group. Obviously, since it was the selection criterion, all had high total cholesterol and LDL-C, with significant differences compared to the other groups. However, HDL-C levels were similar to those observed in controls. None of them had HDL-C levels below 35 mg/dL.
With respect to measurements of arterial stiffness and IMT (Table 2), on comparing the CVRF groups with the controls we found that all parameters increased in CVRF patients compared to the controls; however, these differences were only statistically significant for the β, Ep, PWV and arterial diameters in obese children. Statistically significant differences in AC also were observed, but only in dyslipidemic patients compared to controls. On comparing the 2 CVRF groups, significant differences were found only in AI and arterial diameters.
The IMT measurements were taken in 42 cases (18 obese children, 9 dyslipemic children, and 15 controls). Analysis of results showed no significant differences between groups.
The results of the correlation analysis between anthropometric and biochemical parameters compared with vascular parameters are summarized in Table 3: in controls DBP was correlated with PWV and HDL-C with vascular parameters (β, AC, and PWV); in obese children there was correlation of BMI, SBP and triglyceride levels with vascular parameters (β, Ep, AC, and PWV); in the dyslipidemic subjects, a correlation was only found between triglyceride levels and β, Ep and PWV. IMT was not correlated with any biochemical parameters apart from triglyceride levels in the dyslipidemic group.
DISCUSSION
The preclinical phase of atherosclerosis begins in childhood, when very early alterations that progress slowly have been described1-5 and which do not usually lead to ischemic complications in adulthood. Early detection of the extent of arterial degeneration caused by atherosclerosis using noninvasive techniques, based on ultrasound, has provided an important stimulus to develop early detection programs and to assess the effects of intervention in the pediatric population.
So far most research conducted in children and adolescents has studied the IMT to determine the vascular damage in CVRF patients, mainly in obese children.21,22,34 However, results show there is already structural damage to the arterial wall and thus indicate that measurements of arterial stiffness parameters reflect dysfunction earlier on, which is, therefore, potentially reversible.16,35 Numerous studies have shown that PWV in children and adolescents is significantly correlated with CVRF and increases gradually with age in both sexes. In young adults, this parameter has been established as a good measure of arterial stiffness, proving to be an important predictor of cardiovascular events.32,36
Other parameters to assess arterial stiffness, such as arterial compliance and distensibility, evaluate the role of the artery studied as a hollow structure. The Ep parameter can be regarded as a measure of the intrinsic rigidity of the arterial wall itself and is inversely related to arterial elasticity.32 Two other parameters used in adults have been the beta stiffness index, which assesses the elastic properties of the arterial wall independent of distending pressure and AI as an indirect index to evaluate aortic elasticity.37
In this study, the age range (8 to 16 years) was chosen expecting major changes would take place in carotid elastic properties as compared to the control group. The average age was similar in all groups, even slightly lower in the dyslipidemic group of children; therefore, the differences detected in functional vascular parameters cannot be attributed to age.
On comparing arterial stiffness parameters of healthy children with those of CVRF children, they were higher in the latter, but statistically significant differences were only found in beta stiffness index b, Ep, PWV and arterial diameters in obese children and for AC in dyslipemic patients. Differences in AI and arterial diameters were found between the 2 vascular risk groups. Similar results have been recorded by other authors in both obese and dyslipidemic patients.16,35 However, on assessing whether structural changes were reflected in the IMT, no differences were found in either study group when functional anomalies had already shown up. Bearing in mind the limitations due to sample size, these results seem relevant and support the potential use of these functional indices as early markers of vascular injury in individuals at risk. Studies with larger sample sizes and longer follow-up periods can validate these findings.
The results obtained show the onset of changes in arterial elasticity take place sooner in obese children than in those with dyslipidemia. We also found that blood pressure values were significantly higher than other groups, although they did not reach hypertense levels. This same group also revealed a pattern associating dyslipidemia with significantly lower HDL-C values and higher triglyceride levels, which would suggest they are at an early stage of metabolic syndrome. Moreover, BMI, SBP and triglycerides were significantly correlated with arterial stiffness indices, which would directly indicate adiposity as a trigger of vascular injury. These findings support the need to implement intervention programs for obese school children and adolescents in order to delay the process before adulthood. Similarly, postoperative follow-up of vascular anomalies would be of great interest to evaluate the possible reversibility of functional alterations and/or IMT.
With regard to the relationship between dyslipidemia and cardiovascular disease, there is no doubt that low levels of LDL-C play a role in the prevention and treatment of coronary disease. The effect of dyslipidemia on arterial elastic properties has been extensively studied in adults, where healthy individuals have shown an inverse relationship between LDL levels and aortic compliance.38 Elasticity of the common carotid artery was also assessed in normotensive hypercholesterolemic patients (with or without varying degrees of coronary disease), in hypertensive normocholesterolemic patients (without coronary disease) and healthy controls. Results indicated reduced carotid compliance mainly occurred in normotensive hypercholesterolemic patients, suggesting that reduction in compliance is an indicator of severe atherosclerosis.39
In children with heterozygous familial hypercholesterolemia, an increase in stiffness of the carotid artery has been observed. This group of patients was found to have LDL-C levels that were positively correlated with PWV.13,35 However, no correlation was found between either Ep or IMT and total cholesterol or LDL-C levels.35 Our patients with dyslipidemia showed significantly higher values of LDL-C than the obese patients and controls, with HDL-C values in all 3 groups over 35 mg/dL. In this group there were statistically significant differences in AC compared with controls; however, we did not observe any correlation between LDL-C levels and vascular damage as reported by other authors,35 possibly because the sample size of this group was smaller than the others.
Significant changes in functional vascular parameters in the 2 CVRF groups would seem to indicate that the arterial wall components are affected very early on, which probably leads to the onset of IMT found in these patients. Nevertheless, on analyzing this structural parameter in our study groups, we found no significant differences in IMT compared to controls, suggesting that this structural parameter is affected later on. These results lead us to the conclusion that functional vascular parameters are the ultrasonographic indicators which change the earliest in children with CVRF.
CONCLUSIONS
The ultrasonographic measurement of arterial stiffness is a sensitive procedure which can serve asan earlier marker than IMT for detecting vascular changes in children with CVRF. Systematic application of these techniques may have important preventive implications because it would provide a marker of atherosclerosis at the preclinical phase of the disease. Detection of functional alterations in children at risk would enable them to benefit from early therapeutic measures, thereby preventing or delaying the development of atherosclerosis when they reach adulthood.
ABBREVIATIONS
BMI: body mass index
CVRF: cardiovascular risk factor
DBP: diastolic blood pressure
Dd: diastolic (or minimum) arterial diameter
Ds: systolic (or maximum) arterial diameter
SBP: systolic blood pressure
This work was supported by the 2009 Sira Carrasco Research Grant, awarded by the Sociedad Española de Gastroenterología, Hepatología y Nutrición Pediátrica (SEGHNP).
Correspondence: Dra. C. Martínez-Costa.
Departamento de Pediatría, Obstetricia y Ginecología. Universidad de Valencia. Sección de Gastroenterología y Nutrición Pediátrica. Hospital Clínico Universitario de Valencia.
Avda. Blasco Ibáñez, 17. 46010 Valencia. Spain
Correo electrónico: ceciliam@comv.es
Received October 24, 2009.
Accepted for publication April 21, 2010.