Keywords
INTRODUCTION
Several studies in western countries have investigated the relationship between the number of cardiac procedures (NPC) at a hospital and surgical outcome.1,2 Many have found an inversal relationship between NPC and mortality.3-6 However, other studies have challenged this relationship7 and the experience factor itself has even been called into question.8,9 Most studies that found a relationship were performed in countries where the cardiologist and patient are free to choose the hospital.
The aim of this study was to analyze the influence of the NPC performed in Spanish hospitals on cardiac surgery outcome, taking into account the characteristics of the health care system which has a lower average number of interventions per hospital than the European average and which does not permit the patient to choose the hospital.
METHODS
This was a descriptive prospective observational study carried out in tertiary hospitals using grouped data. A proposal was sent to all the hospitals listed in the Spanish Society of Thoracic and Cardiovascular Surgery census, inviting their participation in an audited independent study to collect detailed information on risk factors and 1-year patient mortality. The study was designed to include a confidentiality protocol using computerized encryption procedures and a randomized mathematical model that guaranteed confidentiality regarding the data source. Data on surgeons were included in each hospital's database to facilitate internal quality analysis within each service, but this data was excluded from the joint database by prior agreement, as it was thought that anonymity would encourage participation. A total of 21 hospitals agreed to participate in the initial study-phase.
Each participating hospital prospectively collected information on 50 clinical risk factors predictive of mortality for every patient undergoing major heart surgery between January 1, 2004 and December 31, 2004. Hospital deaths occurring at any stage between the first cardiac intervention and hospital discharge were recorded as death due to surgery regardless of cause or in which hospital service it occurred. Early deaths occurring up to 30 days after the intervention among discharged patients were not recorded. Data on the parameters were recorded using the data format required to estimate surgical risk using the Parsonnet,10,11 EuroSCORE,12,13 Ontario,14 QMMI, and New England15 methods. Data was entered into a customized software database. Each hospital transmitted the encoded data to a virtual database stored on internet before being checked by an external referee.
In the second phase, the reliability of this data was checked against the data collected independently by referees who visited each hospital. Each service was audited by a different cardiovascular surgeon belonging to the study group, randomly selected from the project researchers under the following requirements:
1. Does not belong to the same region as the audited hospital.
2. Does not audit a hospital that, in turn, is going to audit theirs, and does not audit a hospital that audits another one which, in turn, will audit their hospital (to avoid 3-way interference).
3. Has not been excluded by the auditing hospital or excluded as a hospital auditor, according to a confidential rejection list established before randomization.
Official information on the number of patients undergoing cardiac surgery and surgical deaths was requested from the management of each hospital to avoid patient loss. Each referee fully reviewed a set of 20 case histories randomly assigned by the study organization after each hospital had sent in their data. The case history data directly obtained by the referees dealing with these case histories and the data obtained from the hospital management was combined with the information sent by each service. A total of 16 participating hospitals completed all stages and correctly validated their data. No differences were found between the number of deaths reported by the services and that found by the referees in the independent data review. There was a mean agreement of 94% between each hospital and the referee regarding risk factors. Two of the physical hospitals participating in the study shared the same surgical team and the same patient list and their patients underwent surgery in either hospital; thus, for the sake of consistency, their data were grouped and represented a single virtual hospital.
Using the verified data from each hospital, surgical risk was estimated for each patient using the Parsonnet and EuroSCORE methods according to the original algorithm described by the authors. Total surgical mortality was estimated for each hospital as well as the 95% confidence interval and the mortality index obtained by dividing absolute mortality in each hospital by mortality estimated with the most commonly used predictive methods.
The relationship between the NPC performed in each participating hospital and their crude and risk-adjusted mortality rate was estimated using Pearson's correlation coefficient, after verifying for normal distribution of the parameters using the Kolmogorov-Smirnov test to find the confidence interval of the coefficients, and the statistical significance of the relationship. An overall analysis was performed followed by another after discarding the outliers by eliminating the hospital with lowest crude mortality and the hospital with the highest from the equation. The SPSS software program, version 12.0 (SPSS, Illinois, USA), was used in the statistical analysis.
RESULTS
Every patient who underwent cardiac surgery in the hospitals listed in Table 1 during the year 2004 were enrolled in the study, gathering 6054 cases, cuhich, represents 35% of the national activity in adults cardiac surgery procedures in Spain according to the Spanish Society of Thoracic and Cardiovascular Surgery registry. A total of 468 patients died. Mean age was 65 (median, 68) years. Distribution by sex was men, 65% and women, 35%. Table 2 presents the overall results by procedure, compared with mortality recorded in the Spanish Society of Thoracic and Cardiovascular Surgery registry. Table 3 shows estimated average risk. The risk-adjusted mortality index was 0.81 using the Parsonnet method and 1.12 using the Euro-SCORE method.
The correlation coefficient for the NPC of each hospital and risk profile was r=0.268 (P=.334) using the Parsonnet method and r=0.193 (P=.492) using the Euro-SCORE method.
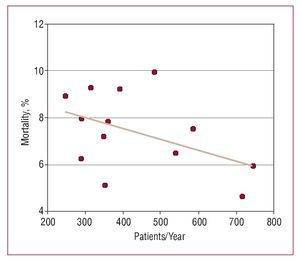
The correlation coefficient for NPC and crude mortality was r=0.065 (P=.819). Two hospitals deviated from central tendency: one with no mortality, but with less than 50 interventions, and the other with mortality higher than 10%. After eliminating data from the hospitals with the lowest and highest mortality rates, the coefficient was r=-0.464 (P=.110) (Figure 1).
Figure 1. Linear regression analysis between crude mortality and the number of major cardiac surgery procedures per year per hospital, discarding hospitals with the highest and lowest mortality rates. r=-0.464 (nonsignificant).
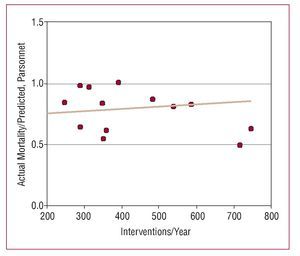
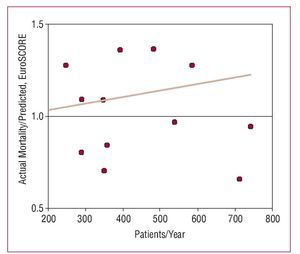
The correlation coefficient for the NPC of all hospitals and risk-adjusted mortality was r=0.092 (P=.745) using the Parsonnet method, and r=0.111 (P=.695) using the EuroSCORE method. After eliminating data from the hospitals with the highest and lowest mortality rates, r=-0.420 (P=.153) and r=-0.267 (P=.378), respectively (Figures 2 and 3).
Figure. 2. Linear regression analysis between the risk-adjusted mortality index (Parsonnet method) and the number of major cardiac surgery procedures per year per hospital, discarding hospitals with the highest and lowest mortality rates. r=-0.420 (nonsignificant).
Figure 3. Linear regression analysis between the risk-adjusted mortality index (EuroSCORE method) and the number of major cardiac surgery procedures per year per hospital, discarding hospitals with the highest and lowest mortality. r=-0.267 (nonsignificant).
DISCUSSION
Several studies have found an inverse relationship between the NPC of a hospital and risk-adjusted mortality16-21 in countries where there is a free choice of hospitals and where patients and referring physicians tend to select the hospital where surgery will take place. This volume-outcome relationship has been attributed to 2 possible factors22:
- Increased activity leads to excellence and thus there are better outcomes
- Excellent hospitals attract more patients
In the case of cardiac surgery, studies comparing the NPC-mortality relationship are not as conclusive as those investigating other areas of surgical activity. Although some studies have found a clear relationship, especially in coronary surgery, other studies have only observed worse results in hospitals with minimal activity,23 and others have found comparable results in hospitals based on an NPC above 200 procedures/year.24
The controversy on the effect of the NPC on outcome includes an additional component in Spain. Studies in western countries, especially in the USA, have been conducted within the context of a competitive system where it is possible to choose between several hospitals and where there is a culture of physicians and patients actively selecting hospitals based on results. On the other hand, the Spanish health care model is basically hierarchical and compartmentalized, and in practice free referral of particular patient is complex. The choice of the referral hospital does not depend on the referring physician's perceptions of quality, but on rigid organizational structures based on designated health areas normally having a single cardiac surgery reference hospital. In this system, referring patients to a hospital different from the one in their reference area is the exception, not the rule.
The fragmentation of public cardiac surgery hospitals in Spain is another factor that has to be taken into account. Major hospitals similar to those in central Europe or North America do not exist in Spain. Although in the regional health-care systems there are hospitals which commonly perform more than 1500 cardiac procedures/year, no hospital in Spain regularly performs more than 800 cardiac procedures/year. In addition to the lack of such high-activity hospitals, the mean number of cardiac procedures per hospital in Spain, with a median of 350 CPB/year, is by far lower than that found in Europe.
The debate on the advantages of having large cardiac surgery hospitals that concentrate experience, or spread the cases in many centers based on geographical, logistical and political criteria, rather than efficiency, reached its high-point during last decade, with the transfer of a centralized national health-care system to multiple regional independent health-care systems, at times forced by political convenience. Since then, doubts remain regarding whether the current fragmentation may have adverse effects on desired quality levels.
The present study is the first to analyze risk-adjusted mortality outcomes in Spain. This was made possible with the cooperation of several hospitals which wanted to obtain an accurate and independent picture of the national health-care situation, motivated by their own concerns regarding improving their service. To date, all the available information on cardiac surgery mortality has been based on crude mortality records which were not confirmed by external sources. These registries, of which the Spanish Society of Thoracic and Cardiovascular Surgery25 registry is the best example, offer undeniable value by providing general information and identifying trends. However, there are 2 pending issues with that national registry: first the reliability and accuracy of the reported data; and second, the evaluation of risk factors among patients, since the differences in mortality among hospitals could be attributed to admitting patients with different risk profiles.
After a 1-year collection period, and almost another year of between-hospital checking, data analysis provided true information on crude mortality and risk-adjusted mortality of sufficient accuracy to make credible comparisons among hospitals, adjusted by patient risk.
The Parsonnet and EuroSCORE methods were used to analyze risk-adjusted mortality as these are the most frequently used in out practice in Europe, and have been validated for the Spanish context in different studies.26,27 They constitute a de facto standard, although they have the characteristic limitations of scales that are applied to populations different from the ones that were used to create them.28
The result of our hospital-to-hospital comparison demonstrates that there is no association between NPC and outcome in Spain. This result is maintained for both crude mortality and risk-adjusted mortality. Examination of the different subgroups only reveals a trend towards significance within the high-activity hospital subgroup, such that from 500 interventions/year upwards, where there seems to be a weak inverse association between NPC and outcome. However, the results obtained from this subgroup are not different from those obtained from hospitals with less activity, and thus it cannot be stated, based on our data, that small hospitals yield worse results than large hospitals.
The results also demonstrate that, in general, small hospitals do not select patients with a different risk profile than those with higher activity levels (Figure 4), which is consistent with the rigidity of the referral system. These findings contrast with those found in North America, where low-risk patients select hospitals on the basis of proximity, whereas high-risk patients and those undergoing reintervention tend to choose high-activity hospitals. It is probable that this preference for hospitals of excellence among high-risk patients and their cardiologists is due to their perception that choosing such a hospital is justified "by a worse" or "by the adverse" prognosis.
Figure 4. Risk distribution of each hospital in relation to its annual volume of activity (EuroSCORE method), 95% CI. r=0.193 (nonsignificant).
The consequence of these observations is that, in Spain, in large hospitals and those with less surgical activity per year, good outcomes exclusively depend on their quality as a hospital and not on the NPC performed.
Study Limitations
Almost all national high-activity hospitals (more than 500 interventions/year) participated in the present study, whereas there was less participation by hospitals with less than 300 interventions/year.
The methodological design of the study incorporated a computerized safety protocol that guaranteed the privacy of each hospital's data, such that it was not possible to identify the data source once it had been validated and combined into the common database. The aim of this measure was to prevent fears regarding data security breaches from stopping those hospitals that might perceive their results as being below average from participating. Despite these attempts to obtain as representative a sample as possible, as in all voluntary studies, it is probable that there was a selection bias in favor of the units that were more proactive and interested in quality issues. In this case, there could be a possible bias toward hospitals with better outcomes than average, and thus we cannot infer that the similar results found in our study among participating centers can be reproduced in other centers.
With the same aim of fostering broad and representative participation, no information was included that could identify the surgeon who performed the intervention, and thus an important modification factor could not be analyzed.
This was a non-analytical ecological study and thus could give rise to an ecological fallacy by associating two sets of independent observational data (mortality and volume). Similarly, as only 16 hospitals were included there may have been a lack of statistical power to detect any possible differences.
CONCLUSIONS
No statistically significant relationship was found between cardiac surgery risk in patients undergoing such interventions in national hospitals and NPC per year. Neither was a significant relationship found between the NPC per hospital and their crude mortality and risk-adjusted mortality rates.
ACKNOWLEDGEMENTS
This study would not have been possible without the generous help of all the cardiac surgeons from the participating hospitals who, without institutional support, made a personal and financial effort to participate in data collection and data checking.
ABBREVIATIONS
NPC: Volume of activity at a hospital defined as number of cadiac procedures a year.
This project received no financial assistance.
Correspondence: I. Díaz de Tuesta.
Avda. Atlántico, 89. 38109 El Rosario. Santa Cruz de Tenerife. España.
E-mail: cardiac@tuesta.net
Received June 22, 2007.
Accepted for publication October 30, 2007.