Our aims were to determine acute myocardial infarction (AMI) incidence and mortality rates, and population and in-hospital case-fatality in the population older than 74 years; variability in clinical characteristics and AMI management of hospitalized patients, and changes in the incidence and mortality rates, case-fatality, and management by age groups from 1996 to 1997 and 2007 to 2008.
MethodsA population-based AMI registry in Girona (Catalonia, Spain) including individuals with suspected AMI older than 34 years.
ResultsThe incidence rate increased with age from 169 and 28 cases/100 000 per year in the group aged 35 to 64 years to 2306 and 1384 cases/100 000 per year in the group aged 85 to 94 years, in men and women, respectively. Population case-fatality also increased with age, from 19% in the group aged 35 to 64 years to 84% in the group aged 85 to 94 years. A lower population case-fatality was observed in the second period, mainly explained by a lower in-hospital case-fatality. The use of invasive procedures and effective drugs decreased with age but increased in the second period in all ages up to 84 years.
ConclusionsAcute myocardial infarction incidence, mortality, and case-fatality increased exponentially with age. There is still a gap in the use of invasive procedures and effective drugs between younger and older patients.
Keywords
Ischemic heart disease continues to be the single most important cause of mortality, morbidity, and hospitalization rates in both high-income1,2 and low-income countries.3 Acute myocardial infarction (AMI) is a critical presentation of this disease, owing to its high case-fatality.4 Recent studies indicate that AMI event rates have declined since 1985 in most populations1,5; however, these studies limited their population upper age limit to 65 or 74 years. Data are scarce on the growing European population older than 74 years.6–8
The prevalence and incidence of chronic conditions and associated events, among them AMI, will increase in parallel with population aging.9 Older patients who present with an AMI tend to have more comorbidities, higher case-fatality, and fewer pharmacological and interventional treatments,6,10–12 making it essential to monitor AMI burden, case-fatality, and hospital management at the population level and across all ages.
The present study had 4 aims: a) to determine AMI incidence and mortality rates in the population older than 74 years compared with those in younger age groups; b) to determine the in-hospital AMI 28-day case-fatality in this population; c) to assess the variability in clinical characteristics and AMI management of hospitalized patients across age groups; and d) to analyze changes in the incidence and mortality rates, case-fatality, and management by age groups from 1996 to 1997 and 2007 to 2008.
METHODSDesignThe REGICOR (Registre Gironí del COR or Girona Heart Registry in English) population-based AMI registry for the province of Girona, Catalonia (Spain) included all AMI cases from 1990 to 2009 in the population aged 25 to 74 years. From January 1996 to December 1997 and from January 2007 to December 2008, the registry was extended to include all residents in the study area who were older than 74 years. The present analysis included AMI cases in REGICOR participants older than 34 years.
The methods used in this registry have been described in detail elsewhere.6,13 Briefly, the monitored area included 6 counties of Girona Province in northeast Catalonia (Spain). The population older than 34 years consisted of 339 352 inhabitants in the 1996 to 1997 census and 488 804 in the official 2007 to 2008 intercensus estimate.14 Population distribution by age and sex is presented in Table 1. The study region has 6 community hospitals that send all AMI patients, after emergency treatment, to the single referral hospital with a coronary care unit in the region. This network of public hospitals covers the entire population.
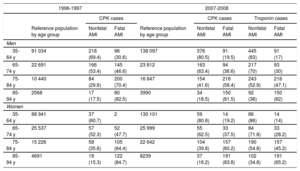
Reference Population and Number of AMI and Fatal AMI Cases Registered in the 2 Study Periods (1996-1997 and 2007-2008)
| 1996-1997 | 2007-2008 | |||||||
|---|---|---|---|---|---|---|---|---|
| CPK cases | CPK cases | Troponin cases | ||||||
| Reference population by age group | Nonfatal AMI | Fatal AMI | Reference population by age group | Nonfatal AMI | Fatal AMI | Nonfatal AMI | Fatal AMI | |
| Men | ||||||||
| 35-64 y | 91 034 | 218 (69.4) | 96 (30.6) | 138 097 | 376 (80.5) | 91 (19.5) | 445 (83) | 91 (17) |
| 65-74 y | 22 691 | 166 (53.4) | 145 (46.6) | 23 812 | 163 (63.4) | 94 (36.6) | 217 (70) | 93 (30) |
| 75-84 y | 10 440 | 84 (29.6) | 200 (70.4) | 16 647 | 154 (41.6) | 216 (58.4) | 243 (52.9) | 216 (47.1) |
| 85-94 y | 2568 | 17 (17.5) | 80 (82.5) | 3990 | 34 (18.5) | 150 (81.5) | 92 (38) | 150 (62) |
| Women | ||||||||
| 35-64 y | 88 941 | 37 (60.7) | 2 | 130 101 | 59 (80.8) | 14 (19.2) | 86 (86) | 14 (14) |
| 65-74 y | 25 537 | 57 (52.3) | 52 (47.7) | 25 999 | 55 (62.5) | 33 (37.5) | 84 (71.8) | 33 (28.2) |
| 75-84 y | 15 226 | 58 (35.6) | 105 (64.4) | 22 642 | 104 (39.8) | 157 (60.2) | 190 (54.8) | 157 (45.2) |
| 85-94 y | 4691 | 19 (15.3) | 122 (84.7) | 8239 | 37 (16.2) | 191 (83.8) | 102 (34.8) | 191 (65.2) |
AMI, acute myocardial infarction; CPK, creatinine phosphokinase.
Data are expressed as No. of individuals or No. (%).
From 2007 to 2008, 2 AMI definitions were applied, excluding and including troponin levels (CPK and troponin cases, respectively).
The study protocol was approved by the local ethics committee and was conducted according to the principles expressed in the Declaration of Helsinki.
Case-finding ProceduresThe MONICA methodology was used to identify and investigate possible AMI cases.15 Briefly, AMI patients admitted to the referral coronary care unit were prospectively registered; those admitted to the referral hospital but not treated in the coronary care unit and those admitted and treated in the community hospitals were retrospectively registered. For this retrospective registry, we reviewed all discharge records from the coronary care unit, standard hospitalization, and emergency room that included the International Classification of Diseases codes 410-411 [9th revision] or I21-I24 [10th revision]. This analysis was performed at least annually for all the hospitals in the area of interest. Any AMI cases referred to medical centers outside the study area were identified by a review of secondary medical transport records. To identify prehospital fatal AMI cases, we reviewed the official Mortality Register of Catalonia. All death certificates that included the International Classification of Diseases codes 410-414 (9th revision) or I20-I22, I24, I25 (10th revision) of residents in the area of interest were selected for review of medical records and autopsy results (if available) to identify any history of ischemic heart disease or evidence of an acute coronary event, respectively.15 Finally, when deemed necessary to complete the information on a particular case, the physician who signed the death certificate and relatives or witnesses were interviewed by telephone. An event in the same patient was considered a new episode when more than 28 days had elapsed after any preceding event(s).
Variables of InterestAge, sex, and place of residence were registered for all AMI patients, along with cardiovascular risk factors (smoking, hypertension, diabetes, hypercholesterolemia) and previous history of AMI or angina. In those patients admitted to hospital, the following variables were recorded: symptoms (typical vs nontypical), levels of myocardial necrosis biomarkers, electrocardiographic characteristics (Q-wave presence, Q-wave location, ST-elevation), initial and maximum Killip classification, severe arrhythmias (ventricular fibrillation or sustained ventricular tachycardia), invasive procedures (coronary angiography, percutaneous coronary intervention, coronary artery bypass grafting), reperfusion (thrombolysis or primary percutaneous coronary intervention), in-hospital drug therapy (antiplatelet drugs, angiotensin-converting enzyme inhibitors, beta-blockers, statins), and 28-day case-fatality.
Case ClassificationEach case was classified according to the MONICA algorithm, which takes into account the type of symptoms, electrocardiographic findings, necrosis biomarkers values, history of ischemic heart disease, and (in fatal cases) autopsy interpretation.15 Cases registered in the 2007 to 2008 period also included troponin level, and the new AMI classification for epidemiological studies proposed by several scientific societies was applied.16 All cases were categorized by trained personnel and referred to a case classification committee for review as needed.
According to the MONICA algorithm,15 5 categories were defined: a) definite AMI; b) possible AMI or coronary death; c) ischemic cardiac arrest with successful resuscitation not fulfilling criteria for definite or possible AMI; d) no AMI or coronary death, and e) fatal cases with insufficient data (unclassifiable deaths). All potential AMI cases were then classified according to 28-day case-fatality: fatal definite AMI, nonfatal definite AMI, fatal possible AMI, nonfatal possible AMI, and fatal cases with insufficient data. Estimation of incidence and mortality rates included nonfatal and fatal definite AMI, fatal possible AMI, and fatal cases with insufficient data.
In accordance with the new AMI classification16 (which includes troponin levels), 4 types of events were included to estimate incidence and mortality rates: nonfatal definite AMI, fatal definite AMI, fatal probable AMI, and fatal possible coronary event.
Statistical MethodsCase-fatality is the proportion of fatal AMI to all AMI cases. The cumulative incidence rate is the number of first and recurrent fatal and nonfatal AMI events divided by the midyear case population. The AMI mortality rate is the number of fatal AMI events divided by midyear case population.
For the 2 study periods (1996-1997 and 2007-2008), the cumulative incidence and mortality rates are presented per 100 000 inhabitants and year and case-fatality as a percentage, by age group (35-64, 65-74, 75-84, and 85-94 years) and by sex. Rates and proportions were calculated according to the normal approximation of the Poisson distribution and binomial distribution, respectively, and are presented with 95% confidence intervals.
The association between age group and categorical variables was assessed by the chi-square test for trends, and trends in continuous variables by linear regression. The level of significance accepted for 2-sided tests was 5%. All the analyses were performed using the R statistical package (version 3.1.0).
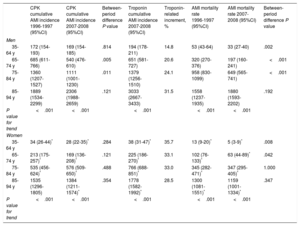
RESULTSThe total number of AMI cases, fatal AMI cases, and the reference population are shown in Table 1 by age group and sex for 1996 to 1997 and 2007 to 2008. We do not show data for the subgroup older than 94 years due to its small number of individuals and events. The cumulative incidence rate and mortality rates in the 2 study periods are presented in Table 2 by age group and sex. The incidence rate was significantly lower in men aged 65 to 74 years and 75 to 84 years in the 2007 to 2008 period; there were no other significant differences. Incidence rates increased with age, and were higher in men than in women in all age groups. However, the incidence ratio of men compared with women decreased with age, from 5.1 to 6.0 in the youngest group to 1.2 to 1.7 in the oldest group. The inclusion of troponin determination in the diagnosis of AMI increased the number of events evenly across all age groups in women (≈ 30%) and linearly with age in men (from 15% in the youngest group to 32% in the oldest group). Mortality rates increased with age and were higher in men than in women, but decreased between the 2 study periods in men aged 35 to 84 years and in women aged 35 to 74 years.
Acute Myocardial Infarction Cumulative Incidence (New and Recurrent Cases) and Mortality Rates per 100 000 Inhabitants per Year (95%CI) by Sex and Age Groups, and Biomarker CPK or Troponin, 1996 to 1997 and 2007 to 2008
| CPK cumulative AMI incidence 1996-1997 (95%CI) | CPK cumulative AMI incidence 2007-2008 (95%CI) | Between-period difference P value | Troponin cumulative AMI incidence 2007-2008 (95%CI) | Troponin-related increment, % | AMI mortality rate 1996-1997 (95%CI) | AMI mortality rate 2007-2008 (95%CI) | Between-period difference P value | |
|---|---|---|---|---|---|---|---|---|
| Men | ||||||||
| 35-64 y | 172 (154-193) | 169 (154-185) | .814 | 194 (178-211) | 14.8 | 53 (43-64) | 33 (27-40) | .002 |
| 65-74 y | 685 (611-766) | 540 (476-610) | .005 | 651 (581-727) | 20.6 | 320 (270-376) | 197 (160-241) | <.001 |
| 75-84 y | 1360 (1207-1527) | 1111 (1001-1230) | .011 | 1379 (1256-1510) | 24.1 | 958 (830-1099) | 649 (565-741) | <.001 |
| 85-94 y | 1889 (1534-2299) | 2306 (1988-2659) | .121 | 3033 (2667-3433) | 31.5 | 1558 (1237-1935) | 1880 (1593-2202) | .192 |
| P value for trend | <.001 | <.001 | <.001 | <.001 | <.001 | |||
| Women | ||||||||
| 35-64 y | 34 (26-44)* | 28 (22-35)* | .284 | 38 (31-47)* | 35.7 | 13 (9-20)* | 5 (3-9)* | .008 |
| 65-74 y | 213 (175-257)* | 169 (136-208)* | .121 | 225 (186-270)* | 33.1 | 102 (76-133)* | 63 (44-89)* | .042 |
| 75-84 y | 535 (456-624)* | 576 (509-650)* | .488 | 766 (688-851)* | 33.0 | 345 (282-471)* | 347 (295-405)* | 1.000 |
| 85-94 y | 1535 (1296-1805) | 1384 (1211-1574)* | .354 | 1778 (1582-1992)* | 28.5 | 1300 (1081-1551)* | 1159 (1001-1334)* | .347 |
| P value for trend | <.001 | <.001 | <.001 | <.001 | <.001 | |||
95%CI, 95% confidence interval; AMI, acute myocardial infarction; CPK, creatinine phosphokinase.
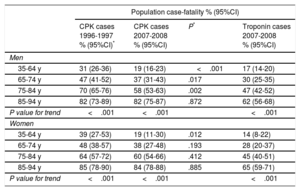
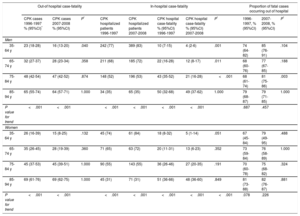
The 28-day population case-fatality increased with age, was similar in men and women in both periods, and significantly decreased in men aged 35 to 84 years and in women aged 35 to 64 years between the 2 study periods (Table 3). Overall, 66% and 88% of fatal AMI cases occurred in men and women, respectively, older than 74 years. Out-of-hospital and in-hospital 28-day case-fatality by sex and age group are shown in Table 4. The out-of-hospital case-fatality increased with age, was similar in men and women in both periods, and decreased between the 2 periods studied in men and women aged 35 to 64 years. The 28-day in-hospital case-fatality showed a similar pattern, although it decreased between the 2 study periods in men aged 35 to 84 years and in women aged 35 to 64 years. Considering only fatal cases, there was a high proportion of out-of-hospital fatalities, which was similar across age groups, regardless of sex and study period (Table 4).
Population Acute Myocardial Infarction 28-day Case-fatality by Sex and Age Groups and CPK or Troponin Biomarkers From 1996 to 1997 and 2007 to 2008
| Population case-fatality % (95%CI) | ||||
|---|---|---|---|---|
| CPK cases 1996-1997 % (95%CI)* | CPK cases 2007-2008 % (95%CI) | P* | Troponin cases 2007-2008 % (95%CI) | |
| Men | ||||
| 35-64 y | 31 (26-36) | 19 (16-23) | <.001 | 17 (14-20) |
| 65-74 y | 47 (41-52) | 37 (31-43) | .017 | 30 (25-35) |
| 75-84 y | 70 (65-76) | 58 (53-63) | .002 | 47 (42-52) |
| 85-94 y | 82 (73-89) | 82 (75-87) | .872 | 62 (56-68) |
| P value for trend | <.001 | <.001 | <.001 | |
| Women | ||||
| 35-64 y | 39 (27-53) | 19 (11-30) | .012 | 14 (8-22) |
| 65-74 y | 48 (38-57) | 38 (27-48) | .193 | 28 (20-37) |
| 75-84 y | 64 (57-72) | 60 (54-66) | .412 | 45 (40-51) |
| 85-94 y | 85 (78-90) | 84 (78-88) | .885 | 65 (59-71) |
| P value for trend | <.001 | <.001 | <.001 | |
95%CI, 95% confidence interval; CPK, creatinine phosphokinase.
Population and Hospitalized Acute Myocardial Infarction 28-day Case-fatality by Sex and Age Group From 1996 to 1997 and 2007 to 2008
| Out-of hospital case-fatality | In-hospital case-fatality | Proportion of fatal cases occurring out of hospital | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| CPK cases 1996-1997 % (95%CI)* | CPK cases 2007-2008 % (95%CI) | P* | CPK hospitalized patients 1996-1997 | CPK hospitalized patients 2007-2008 | CPK hospital case-fatality % (95%CI) 1996-1997 | CPK hospital case-fatality % (95%CI) 2007-2008 | P* | 1996-1997, % (95%CI) | 2007-2008, % (95%CI) | P* | |
| Men | |||||||||||
| 35-64 y | 23 (18-28) | 16 (13-20) | .040 | 242 (77) | 389 (83) | 10 (7-15) | 4 (2-6) | .001 | 74 (64-82) | 85 (76-91) | .104 |
| 65-74 y | 32 (27-37) | 28 (23-34) | .358 | 211 (68) | 185 (72) | 22 (16-28) | 12 (8-17) | .011 | 68 (60-76) | 77 (67-85) | .188 |
| 75-84 y | 48 (42-54) | 47 (42-52) | .874 | 148 (52) | 196 (53) | 43 (35-52) | 21 (16-28) | <.001 | 68 (61-74) | 81 (75-86) | .003 |
| 85-94 y | 65 (55-74) | 64 (57-71) | 1.000 | 34 (35) | 65 (35) | 50 (32-68) | 49 (37-62) | 1.000 | 79 (68-87) | 79 (71-85) | 1.000 |
| P value for trend | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | .687 | .457 | |||
| Women | |||||||||||
| 35-64 y | 26 (16-39) | 15 (8-25) | .132 | 45 (74) | 61 (84) | 18 (8-32) | 5 (1-14) | .051 | 67 (45-84) | 79 (49-95) | .488 |
| 65-74 y | 35 (26-45) | 28 (19-39) | .360 | 71 (65) | 63 (72) | 20 (11-31) | 13 (6-23) | .352 | 73 (59-84) | 76 (58-89) | 1.000 |
| 75-84 y | 45 (37-53) | 45 (39-51) | 1.000 | 90 (55) | 143 (55) | 36 (26-46) | 27 (20-35) | .191 | 70 (60-78) | 75 (68-82) | .324 |
| 85-94 y | 69 (61-76) | 69 (62-75) | 1.000 | 45 (31) | 71 (31) | 51 (36-66) | 48 (36-60) | .849 | 81 (73-88) | 82 (76-87) | .881 |
| P value for trend | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | .078 | .226 | ||
95%CI, 95% confidence interval; CPK, creatinine phosphokinase.
Unless otherwise indicated, data are expressed as No. (%).
The clinical characteristics of hospitalized AMI patients across age groups in the 2 study periods are shown in Table 5. The proportion of men and smokers decreased with age in both periods. The proportion of hypertension, diabetes, previous angina, and myocardial infarction increased with age and was significantly higher in the 2007 to 2008 period than in the 1996 to 1997 period. The proportion of patients classified as Killip III to IV also increased with age but was lower from 2007 to 2008 than in 1996 to 1997. The proportion of patients with severe arrhythmias was not related to age but decreased significantly in the second period, when a reduction in the proportion of patients with ST-elevation AMI was observed across age groups.
Sociodemographic and Clinical Characteristics of Hospitalized Acute Myocardial Infarction Patients (Defined Using Creatinine Phosphokinase as Necrosis Biomarker) Across Age Groups in the 2 Study Periods (1996-1997 and 2007-2008)
| 1996-1997 | |||||
|---|---|---|---|---|---|
| 35-64 y n=287 (%) | 65-74 y n=282 (%) | 75-84 y n=238 (%) | 85-94 y n=79 (%) | P for trend | |
| Men | 242 (84.3) | 211 (74.8) | 148 (62.2) | 34 (43.0) | <.001 |
| Age | 54.2 (7.7) | 69.9 (2.7) | 79.4 (3.0) | 87.7 (2.3) | <.001 |
| Hypertension | 129 (46.9) | 153 (55.8) | 142 (60.9) | 46 (59.7) | .002 |
| Diabetes mellitus | 60 (22.2) | 89 (33.6) | 79 (34.2) | 23 (30.3) | .028 |
| Dyslipidemia | 144 (55.2) | 115 (43.4) | 65 (28.5) | 8 (11.3) | <.001 |
| Current smoker | 160 (56.5) | 61 (22.1) | 16 (6.87) | 4 (5.48) | <.001 |
| Angina | 30 (11.5) | 38 (14.4) | 45 (20.2) | 9 (12.9) | .099 |
| Prior AMI | 50 (17.5) | 48 (17.2) | 45 (18.9) | 16 (21.1) | .564 |
| Killip III-IV | 41 (14.7) | 60 (22.7) | 78 (34.7) | 26 (38.3) | <.001 |
| Severe arrhythmias | 49 (17.8) | 39 (14.6) | 44 (19.3) | 8 (11.8) | .854 |
| 2007-2008 | |||||
|---|---|---|---|---|---|
| 35-64 y n=450 (%) | 65-74 y n=248 (%) | 75-84 y n=339 (%) | 85-94 y n=136 (%) | P for trend | |
| Men | 389 (86.4) | 185 (74.6) | 196 (57.8) | 65 (47.8) | <.001 |
| Age | 53.8 (7.16) | 69.9 (2.89) | 79.3 (2.82) | 87.8 (2.57) | <.001 |
| Hypertension | 246 (55.8) | 164 (67.2) | 267 (80.2) | 104 (77.6) | <.001 |
| Diabetes mellitus | 127 (29.6) | 95 (38.9) | 135 (40.7) | 59 (44.4) | .001 |
| Dyslipidemia | 266 (61.6) | 127 (52.5) | 68 (43.6) | 6 (37.5) | <.001 |
| Current smoker | 275 (61.9) | 61 (25.0) | 29 (9.01) | 5 (3.85) | <.001 |
| Angina | 56 (12.8) | 43 (18.0) | 92 (28.7) | 44 (34.1) | <.001 |
| Prior AMI | 61 (13.8) | 55 (22.5) | 93 (28.5) | 31 (24.2) | <.001 |
| Killip III-IV | 35 (8.1) | 42 (18.2) | 85 (26.7) | 49 (37.6) | <.001 |
| Severe arrhythmias | 23 (5.34) | 13 (5.68) | 11 (7.10) | 1 (6.25) | .491 |
| ST-elevation AMI | 267 (60.0) | 126 (51.2) | 163 (49.2) | 47 (35.3) | <.001 |
| Non–ST-elevation AMI | 148 (33.3) | 97 (39.4) | 126 (38.1) | 60 (45.1) | <.001 |
| Nonclassifiable ST | 8 (1.80) | 12 (4.88) | 31 (9.37) | 18 (13.5) | <.001 |
| Q-wave | 22 (4.94) | 11 (4.47) | 11 (3.32) | 8 (6.02) | <.001 |
AMI, acute myocardial infarction.
The management and treatment of hospitalized AMI patients across age groups in the 2 periods is shown in Table 6. The use of antiplatelet drugs, beta-blockers, thrombolytics, coronary angiography, and revascularization procedures decreased across age groups from 1996 to 1997. In the later period, there was a significant increase in the prescription of antiplatelet, angiotensin-converting enzyme inhibitor, beta-blockers, statins, and thrombolytics and in the use of coronary angiography and revascularization. This increase was remarkably high in those aged 75 to 84 years.
Pharmacological and Invasive Management of Hospitalized Acute Myocardial Infarction Patients (Defined Using Creatinine Phosphokinase as Necrosis Biomarker) Across Age Groups in the 2 Study Periods (1996-1997 and 2007-2008)
| 1996-1997 | |||||
|---|---|---|---|---|---|
| 35-64 y n=287 (%) | 65-74 y n=282 (%) | 75-84 y n=238 (%) | 85-94 y n=79 (%) | P for trend | |
| Antiplatelet drugs | 260 (92.5) | 239 (88.5) | 188 (81.0) | 64 (83.1) | <.001 |
| ACE inhibitors | 86 (30.5) | 81 (29.7) | 65 (28.1) | 17 (22.1) | .693 |
| Beta-blockers | 139 (49.3) | 71 (26.1) | 22 (9.57) | 2 (2.60) | <.001 |
| Statins | --- | --- | --- | --- | --- |
| Thrombolysis | 124 (43.5) | 87 (31.6) | 22 (9.40) | 1 (1.28) | <.001 |
| Coronary angiographya | 84 (29.5) | 62 (22.6) | 18 (7.63) | 0 (0.00) | <.001 |
| Revascularizationa | 27 (10.0) | 17 (6.42) | 3 (1.30) | 0 (0.00) | <.001 |
| 2007-2008 | |||||
|---|---|---|---|---|---|
| 35-64 y n=450 (%) | 65-74 y n=248 (%) | 75-84 y n=339 (%) | 85-94 y n=136 (%) | P for trend | |
| Antiplatelet drugs | 418 (98.6) | 229 (97.4) | 156 (98.7)b | 14 (100)b | .988 |
| ACE inhibitor | 322 (74.9) | 176 (75.5) | 125 (80.1)b | 8 (53.3)b | .442 |
| Beta-blockers | 389 (89.4) | 188 (80.7) | 124 (80.0)b | 8 (53.3)b | <.001 |
| Statins | 400 (94.3) | 206 (89.2) | 141 (89.2)b | 11 (73.3)b | <.001 |
| Thrombolysis | 132 (49.6) | 49 (39.5) | 67 (41.9)b | 6 (12.8)b | |
| Primary PCI | 33 (12.4) | 17 (13.7) | 16 (10.0)b | 2 (4.26)b | |
| Reperfusionc | 165 (62.0) | 66 (53.2) | 83 (51.9)b | 8 (17.0)b | |
| Coronary angiographya | 376 (86.4) | 171 (70.7) | 156 (48.6) | 7 (5.26) | |
| Revascularizationa | 326 (75.3) | 141 (59.5) | 118 (36.9) | 6 (4.48) | |
ACE, angiotensin-converting enzyme; PCI, percutaneous coronary intervention.
The present study assessed the burden of AMI in the population older than 34 years in 2 periods a decade apart: 1996 to 1997 and 2007 to 2008. The incidence and case-fatality of AMI exponentially increased with age in both men and women. We also report a decrease in AMI incidence from 1996 to 1997 and 2007 to 2008 in men aged 65 to 84 years. Population case-fatality also decreased in men in the population aged 35 to 84 years and in women in the population aged 35 to 64 years. Although a decrease in out-of-hospital case-fatality was observed in young men and women, the population case-fatality change was more closely associated with decreased in-hospital case-fatality. The use of troponin as a myocardial necrosis biomarker increased AMI incidence in women by approximately 30% across age groups and from 15% in young men to 32% in the oldest group of men. The proportion of AMI patients with Killip III to IV and non–ST-elevation AMI increased with age. The use of invasive reperfusion procedures and drugs with proven efficacy (antiplatelets, beta-blockers, angiotensin-converting enzyme inhibitors, statins) increased in the second period in all age groups up to 84 years.
Acute Myocardial Infarction Incidence Across Age GroupsSimilar to the results observed in previous studies,6,17 the incidence of AMI increased exponentially with age, especially in women. However, AMI incidence was higher in men than in women in all age groups. The effect of the inclusion of troponins in the estimation of AMI incidence was higher in women, increased with age in men, but remained stable across age groups in women. These results are concordant with those reported by other authors18–20 and could be related to a sex- and age-related pathological mechanism of acute coronary syndrome, with a more important role for microvascular disease and plaque erosion in women and older individuals and for plaque rupture in men and the younger population.21–23
Differences in Acute Myocardial Infarction Incidence From 1996 to 1997 and 2007 to 2008The cumulative rate of AMI incidence decline between the 2 study periods is consistent with previous reports from other European countries that have analyzed the population aged 35 to 74 years.5 In the second study period, we also observed a decline in AMI incidence in men aged 65 to 84 years, while the incidence remained stable in women. Similar incidence rate findings have been recently reported in England for the period 2002 to 2010, with a significant decrease in younger age groups but no significant changes at older ages.24 These trends could reflect the impact of primary prevention strategies that are compressing the occurrence of AMI to older age groups. Differences in trends between men and women could be related to differences in the intensity of the application of preventive strategies by sex.25 Moreover, the most common clinical manifestation of cardiovascular disease in women is cerebrovascular disease2,26; the competing risk between these 2 clinical entities could explain the absence of changes in AMI incidence rates in women.
Acute Myocardial Infarction Mortality Rate and 28-day Case-fatality Across Age GroupsThe mortality rate depends on the incidence rate and case-fatality. In our study, mortality and incidence rates showed a similar pattern. Population and in-hospital 28-day case-fatality increased with age and was similar in men and women, showing that the previously described sex gap has disappeared. As reported in other series, most fatal cases occurred in the population older than 74 years6 and predominantly in out-of-hospital settings. However, the proportion of out-of-hospital fatal cases was very high and was similar across age groups in both sexes. Similar results have been reported in other series, highlighting the problem of out-of-hospital death.27,28
Acute Myocardial Infarction Mortality and 28-day Case-fatality Differences From 1996 to 1997 and 2007 to 2008In-hospital case-fatality declined in the population younger than 85 years in men and in women up to 65 years between the 2 study periods. This decline could be explained by improved management of AMI patients: adherence to current clinical guidelines increased the use of effective drugs and invasive procedures.29 Similar results have been reported in other series,30 suggesting that the oldest age group seems to have missed this benefit. The low rate of revascularization in this age group, also observed in other studies,31 could explain the findings.
The decrease in out-of-hospital case-fatality in the young population5 and the faster decline of in-hospital than out-of-hospital case-fatality28,32 has also been observed in other populations and explains the increased contribution of out-of-hospital deaths to overall case-fatality. We cannot rule out the possibility that these trends could be explained by some methodological issues, mainly related to the validity of coding the cause of death. However, the methods and information sources were the same in the 2 analyzed periods, suggesting that the impact of any potential bias would be similar in both. Furthermore, similar population trends have been reported in other populations.5 In summary, this growing body of evidence supports the need for population-based policies to decrease the burden of the disease, such as smoking bans, nutritional and exercise promotion programs, efforts to improve the prompt arrival of AMI patients at emergency departments and research on the impact of community access to appropriate early defibrillation.
Acute Myocardial Infarction Clinical Characteristics Across Ages and Study PeriodsThe present study showed an age-related decrease in the proportion of men and of smokers and an increase in the proportion of patients with hypertension and diabetes. The proportion of patients with non–ST-elevation AMI and with previous angina and myocardial infarction also increased with age. The non–ST-elevation AMI increase with age has been reported in other series33 and may reflect the aggressive primary and secondary prevention strategies implemented in the first decade of the 21st century,34 or perhaps a different pathogenic mechanism across age groups with a higher relevance of plaque erosion instead of rupture in older individuals.21,22
We also observed an increase in the proportion of patients (mainly older patients) with prior AMI in the second period, which could be explained by the decrease in case-fatality of the first episodes. Moreover, we observed a decrease in the proportion of patients with admission Killip class III to IV and with severe ventricular arrhythmias, both of which could be related to the widespread use of more effective therapies.
The use of invasive strategies and evidence-based drugs in managing patients with AMI decreased with age. However, it is noteworthy that this age-related difference disappeared from 1996 to 1997 and from 2007 to 2008 for antiplatelet drugs, and that the use of beta-blockers, angiotensin-converting enzyme inhibitors, and invasive strategies increased in the oldest age groups.
Strengths and LimitationsThe main strength of this study lies first in its population basis, which included both in-hospital and out-of-hospital AMI cases; second, in the inclusion of AMI cases without age limits; and third, in the use of standardized methods in 2-year periods separated by a decade. Moreover, we used 2 AMI definitions, with and without troponins, to guarantee the comparability of AMI incidence and mortality rates and case-fatality across periods.
A limitation to be considered is that our most recent data are from 2007 and 2008. An AMI code for ST-elevation acute coronary syndrome patients was implemented in our region in June 2009. This code has improved care in the acute phase of these events, increasing revascularization rates and decreasing delays,35,36 but our study period precluded assessment of its impact at the population level.
CONCLUSIONSAlthough AMI incidence rates tended to decrease in the first decade of this century, AMI incidence increased exponentially with age. Both AMI mortality and case-fatality also increased with age, but substantially decreased in the first decade of this century. Specifically, in-hospital case-fatality decreased more steeply than out-of-hospital case-fatality. In-hospital management of AMI patients still shows a lower use of invasive treatments and evidence-based drugs in older age groups, but this gap decreased during the first decade of this century. Additional efforts are necessary to decrease out-of-hospital case-fatality.
FUNDINGThis project was funded by the Carlos III Health Institute-European Regional Development Fund (ERDF) (FIS 94/0540, FIS 99/0013-01, FIS 99/9342, FIS PI020471, INTRASALUD PI11/01801, FIS PI08/1327, CP12/03287, Red de Investigación Cardiovascular RD12/0042, CIBERCV, CIBERESP); and the Government of Catalonia through the Agency for Management of University and Research Grants (2009SGR1195, 2014SGR240). I. R. Degano was funded by the RECERCAIXA Program, Obra Social “LaCaixa” (RE087465), M. Grau is funded by an ERDF contract from Carlos III Health institute (FIS CP12/03287).
CONFLICTS OF INTERESTNone declared.
- –
Data on AMI incidence, mortality and case-fatality are scarce for the growing European population older than 74 years.
- –
The population incidence rate and case-fatality of AMI exponentially increased with age in both men and women.
- –
The AMI incidence rate was 169 and 28 cases/100 000 per year in the group aged 35 to 64 years, and 2306 and 1384 cases/100 000 per year in the group aged 85 to 94 years, in men and women, respectively.
- –
Population case-fatality also increased with age, from 19% in the group aged 35 to 64 years to 84% in that aged 85 to 94 years.
- –
The burden of AMI in the population older than 74 years is very high, indicating that the absolute number of AMI events will increase in relation to the aging of the European population.
.
To the REGICOR investigators and participants.