Hybrid positron emission tomography (PET) and magnetic resonance (MR) imaging is an emerging technology in the diagnosis of cardiovascular disease; however, there have been no reports of its use in the national clinical setting. Our objective was to evaluate the additional value of integrated PET/MR systems compared with MR and PET performed separately in this setting.
MethodsWe prospectively included 49 patients, 30 to assess myocardial viability (coronary group) and 19 to assess inflammatory, infectious, and tumoral diseases (noncoronary heart disease group). All patients underwent cardiac 18F-fluorodeoxyglucose PET/MR. PET/MR studies included attenuation correction sequences, followed by simultaneous cardiac PET and cardiac MR acquisition, with protocols adapted to the clinical indication (cine, tissue characterization and/or late enhancement imaging).
ResultsMost (87.8%) PET/MR studies were initially interpretable. Use of PET/MR improved diagnosis vs PET or MR performed separately in 42.1% of coronary cases and 88.9% of noncoronary cases. PET/MR enabled reclassification of 87.5% of coronary cases initially classified as showing inconclusive results on MR or PET and 70% of noncoronary cases.
ConclusionsIn our series, multimodality PET/MR technology provided additional diagnostic value in some patients with cardiovascular disease compared with MR and PET performed separately, especially in cases of noncoronary heart disease and in those with inconclusive results on MR or PET. In our experience, the main benefits of PET/MR include the possibility of simultaneous acquisition, the in vivo integration of anatomical/functional/metabolic aspects, and the interaction of different experts in imaging modalities.
Keywords
Hybrid positron emission tomography (PET) and magnetic resonance (MR) imaging is emerging as a promising technology for the study of cardiovascular disease. The main advantage of these systems is that the anatomic and functional images provided by MR can be simultaneously integrated with the metabolic data obtained by PET in a single acquisition and with an excellent spatial correlation.1 Initially, integrated systems combining PET and computed tomography (CT) were more widely developed than PET/MR because of their extensive use in oncology and the higher precision of attenuation maps generated by CT. However, technological advances in the last few decades have made it possible to overcome the earlier technical limitations of PET/MR and to introduce its use in cardiovascular patients.2,3 Several potential cardiovascular indications have been described, such as evaluation of myocardial viability, inflammatory and infiltrative cardiomyopathies, endocarditis, pericardial disease, and cardiac masses.1,4,5 This new technology enables improved tissue characterization and functional assessment with lower radiation exposure than PET/CT. Nonetheless, few studies have investigated the added value of PET/MR vs each of these techniques separately for evaluating heart disease. Nor are there previous studies in Spain describing the initial experience of its use in our hospital setting.
Our objective was to determine the added value of integrated PET/MR vs MR and PET separately in the diagnosis of cardiovascular disease. In addition, we describe our experience with a hybrid PET/MR system in the clinical setting, which could help launch similar programs and facilitate their incorporation in the diagnostic arsenal for cardiovascular conditions.
METHODSStudy populationIn accordance with the latest recommendations on clinical indications for cardiac PET/MR,6,7 we prospectively included patients older than 15 years referred to the nuclear medicine department for PET to evaluate myocardial viability, cardiac masses, or endocarditis, and to the cardiac imaging unit for MR to assess myocardial viability in known coronary disease or inconsistent findings in other ischemia screening tests, to evaluate cardiac masses and inflammatory or infiltrative heart disease, or to assess endocarditis with an inconclusive diagnosis on echocardiography. We excluded patients with electrical devices or claustrophobia, pregnant women, and those with a persistent glucose concentration >200mg/dL following the PET scan preparation requirements. Before programming the PET/MR study, patients were classified into 2 groups: a) a coronary group when the examination was destined to assess myocardial viability, and b) a noncoronary group when the study was performed to assess inflammatory/infiltrative heart disease, a cardiac mass, or endocarditis. This was done to provide suitable pretest preparation, as a patient's preparation requirements differ according to the imaging protocol assigned. The study was approved by the local hospital ethics committee.
Patient preparation and image acquisition protocolThe radiotracer used was 18F-fluorodeoxyglucose (18F-FDG) because of its widespread availability and long half-life, following a described method.7 Patients in the coronary group fasted for 12hours, and based on the pre-test blood glucose level, were administered an oral overload of glucose or insulin, according to the protocol (). Patients in the noncoronary group received a carbohydrate-free, fat-rich diet during the previous 24hours and were given an intravenous dose of unfractionated heparin at 50 IU/kg before the study. In each case, the calculated 18F-FDG dose was adjusted to the patient's weight and the extent of the PET scan, and patients waited at rest for 45minutes after the injection to avoid extracardiac uptake. The radiation administered was in accordance with the recommendations derived from current radioprotection laws and the ALARA (As Low As Reasonably Achievable) precept.8
Image acquisition was done on an integrated 3T MR and PET system (Biograph mMR, Siemens Healthcare, Germany),9 with HD technology, 16-channel surface coils, and cardiac synchronization. The PET/MR study began with attenuation correction sequences. Cardiac PET was then planned to include the area from the aortic arch to the upper border of the diaphragm (12cm, with an approximate duration of 30minutes). Last, multiparametric MR sequences7 were performed simultaneously with PET. These included cine sequences (SSFP) and short-axis delayed-enhancement sequences at 10minutes following Gadovist (0.2 mmol/kg) injection, with coverage from the base to apex of the heart. In addition, based on the clinical indication, T1- or T2-weighted turbo spin echo, perfusion, and valvular phase contrast sequences were added to the protocol. In some cases directed toward assessing endocarditis, full-body PET/MR was included.10
18F-FDG PET/MR image analysisThe MR, PET, and fused PET/MR images were analyzed by diagnostic imaging specialists using the Syngo.via program (Siemens Healthineers, Germany). Initially, each MR study was assessed by cardiologists and each PET study by nuclear medicine specialists separately, and then, the PET/MR analysis was performed together. In the MR cine images, the epicardial and endocardial contours of each short-axis view of the left ventricle were traced manually to calculate the volumes and heart function (Simpson method). Dilatation, hypertrophy, and segmental abnormalities were assessed using the 17-segment model of the American Heart Association,11 and the anatomic location/extent of lesions, valve function, T1/T2 hyperintensities, and perfusion patterns were determined according to the indication. Gadolinium uptake was defined as areas of hyperenhancement on delayed images relative to enhancement of the normal myocardium in each of the 17 myocardial segments by subjective evaluation, a highly reproducible method used in daily practice in most imaging units.12 Segments were considered to have a subendocardial pattern when the extent of enhancement was <50% (viable myocardium), an intermediate pattern when the extent of transmural enhancement was 50% to 75% (viability inconclusive),14 and a transmural pattern when enhancement was 75% to 100% (nonviable).13,14 In PET images, preserved metabolism was established on 18F-FDG uptake >50% (viable myocardium) and severe hypometabolism on uptake <50% (viability inconclusive); no uptake indicated nonviable myocardium.15,16 A segment-by-segment analysis was carried out to determine agreement between the viability findings of PET and MR for the 17 myocardial segments, and a patient-by-patient analysis to facilitate translation of the results to real-life practice, in which decisions are made for each individual patient. To establish viability and nonviability in each case, we used the extent of enhancement and regional and overall contractility on MR, and the degree of metabolism on PET.17,18 A study was considered inconclusive for myocardial viability when at least 2 segments showed intermediate enhancement on MR or severe hypometabolism on PET,17,18 and for noncoronary disease when PET or MR separately did not provide sufficient information to reach an imaging diagnosis. Lastly, PET/MR was considered useful when the simultaneous combination of imaging findings (contractility, segmental abnormalities, myocardial thinning, late enhancement, and metabolism) and the interaction between imaging specialists (cardiology and nuclear medicine) improved the diagnosis achieved with MR or PET separately, or helped with the patient's treatment. To further evaluate the diagnostic accuracy of the PET/MR study, the diagnosis was confirmed by clinical follow-up.
Statistical analysisCategorical values were compared using the Wilcoxon test and expressed as number and percentage, whereas continuous variables were compared with the Mann-Whitney U test and expressed as the mean±standard deviation. Statistical analyses were performed using SPSS version 21. The kappa concordance index was used to assess interobserver variability between 2 experienced diagnostic imaging specialists to qualitatively determine the usefulness of integrated PET/MR findings vs PET or MR results separately in each patient.
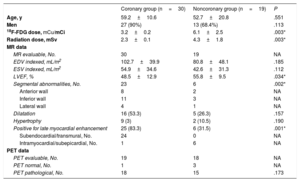
RESULTSIn total, 49 PET/MR studies were performed, 30 in the coronary group (figure 1) and 19 in the noncoronary group (figure 2). The clinical data for each patient are summarized in , and the separate MR and PET data for each group are shown in table 1. There was a predominance of men and mean age was 57 years. Dilatation, segmental abnormalities, and late enhancement were more common in the coronary group. The mean 18F-FDG dose administered was significantly higher in the noncoronary than the coronary group, as whole-body PET was included in some noncoronary cases (6.06 mCi vs 3.2 mCi, equivalent to an effective dose of 4.28 mSv and 2.26 mSv, respectively; P <.001). All hybrid PET/MR studies were successfully completed. Six studies, 5 in the coronary and 1 in the noncoronary group, were not evaluable; hence, 87.8% (43/49) of the PET/MR studies were initially interpretable. In the coronary group, 6 PET studies could not be recovered afterward to complete the detailed analysis by segments. Therefore, the final evaluation included 37 complete PET/MR studies, 19 to assess myocardial viability and 18 for noncoronary disease.
Magnetic resonance and positron emission tomography parameters of patients in the coronary and noncoronary groups
| Coronary group (n=30) | Noncoronary group (n=19) | P | |
|---|---|---|---|
| Age, y | 59.2±10.6 | 52.7±20.8 | .551 |
| Men | 27 (90%) | 13 (68.4%) | .113 |
| 18F-FDG dose, mCu/mCi | 3.2±0.2 | 6.1±2.5 | .003* |
| Radiation dose, mSv | 2.3±0.1 | 4.3±1.8 | .003* |
| MR data | |||
| MR evaluable, No. | 30 | 19 | NA |
| EDV indexed, mL/m2 | 102.7±39.9 | 80.8±48.1 | .185 |
| ESV indexed, mL/m2 | 54.9±34.6 | 42.6±31.3 | .112 |
| LVEF, % | 48.5±12.9 | 55.8±9.5 | .034* |
| Segmental abnormalities, No. | 23 | 6 | .002* |
| Anterior wall | 8 | 2 | NA |
| Inferior wall | 11 | 3 | NA |
| Lateral wall | 4 | 1 | NA |
| Dilatation | 16 (53.3) | 5 (26.3) | .157 |
| Hypertrophy | 9 (3) | 2 (10.5) | .190 |
| Positive for late myocardial enhancement | 25 (83.3) | 6 (31.5) | .001* |
| Subendocardial/transmural, No. | 24 | 0 | NA |
| Intramyocardial/subepicardial, No. | 1 | 6 | NA |
| PET data | |||
| PET evaluable, No. | 19 | 18 | NA |
| PET normal, No. | 1 | 3 | NA |
| PET pathological, No. | 18 | 15 | .173 |
18F-FDG, 18F-fluorodeoxyglucose; EDV, end-diastolic volume; ESV, end-systolic volume; LVEF, left ventricular ejection fraction; MR, magnetic resonance; NA, not applicable; PET, positron emission tomography.
Values express the No. (%) or mean±standard deviation, unless otherwise indicated.
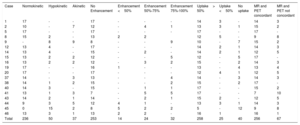
The analysis included 323 myocardial segments, in which contractility, enhancement, and 18F-FDG uptake (table 2) were evaluated. In total 26.9% (87/323) of segments showed abnormalities, mainly hypokinesia in 57.5% (50/87). Enhancement was detected in 21.7% (70/323), including intermediate enhancement in 7.4% (24/323) and transmural enhancement in 9.9% (32/323). In the PET images, 7.7% (25/323) of segments showed severe hypometabolism and 12.4% (40/323) no uptake. Comparison of the MR and PET findings, yielded agreement in 79.3% (256/323) of segments, with a similar prevalence of segments with inconclusive results for viability. An analysis of the inconclusive segments on MR (intermediate enhancement) was performed to assess the usefulness of fusion with PET, and 75% of them (18/24) showed preserved metabolism. In a subanalysis, 16/24 inconclusive segments showed transmurality closer to 50% and all were viable on PET, whereas 8/24 showed transmurality closer to 75% and all segments except 2 were nonviable on PET.
Distribution of segmental abnormalities, late enhancement, and 18F-FDG uptake detected by PET/MR in the coronary patient group, evaluated by segment (n=323 segments)
| Case | Normokinetic | Hypokinetic | Akinetic | No Enhancement | Enhancement <50% | Enhancement 50%-75% | Enhancement 75%-100% | Uptake> 50% | Uptake <50% | No uptake | MR and PET concordant | MR and PET not concordant |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 17 | - | - | 17 | - | - | - | 14 | 3 | - | 14 | 3 |
| 2 | 10 | - | 7 | 12 | - | 4 | 1 | 13 | 3 | 1 | 15 | 2 |
| 5 | 17 | - | - | 17 | - | - | - | 17 | - | - | 17 | - |
| 8 | 15 | 2 | - | 13 | 2 | 2 | 12 | 5 | - | 9 | 8 | |
| 9 | - | 8 | 9 | 8 | - | - | 9 | 10 | - | 7 | 15 | 2 |
| 12 | 13 | 4 | - | 17 | - | - | - | 14 | 2 | 1 | 14 | 3 |
| 14 | 13 | 4 | - | 15 | - | 2 | - | 14 | 2 | 1 | 12 | 5 |
| 15 | 13 | 2 | 2 | 12 | - | - | 5 | 12 | - | 5 | 17 | - |
| 16 | 13 | 2 | 2 | 12 | - | 3 | 2 | 15 | - | 2 | 14 | 3 |
| 19 | 17 | - | - | 16 | 1 | - | - | 13 | - | 4 | 13 | 4 |
| 20 | 17 | - | - | 17 | - | - | - | 12 | 4 | 1 | 12 | 5 |
| 37 | 14 | - | 3 | 13 | - | - | 4 | 14 | - | 3 | 14 | 3 |
| 38 | 14 | 1 | 2 | 15 | - | - | 2 | 15 | - | 2 | 17 | - |
| 40 | 14 | 3 | - | 15 | - | 1 | 1 | 17 | - | - | 15 | 2 |
| 41 | 13 | 1 | 3 | 7 | - | 5 | 5 | 17 | - | - | 7 | 10 |
| 43 | 14 | 2 | 1 | 14 | - | 2 | 1 | 15 | 2 | - | 12 | 5 |
| 44 | 9 | 3 | 5 | 12 | 4 | 1 | - | 13 | 3 | 1 | 14 | 3 |
| 45 | 0 | 15 | 2 | 8 | 5 | 2 | 2 | 5 | - | 12 | 9 | 8 |
| 46 | 13 | 3 | 1 | 13 | 2 | 2 | - | 16 | 1 | 16 | 1 | |
| Total | 236 | 50 | 37 | 253 | 14 | 24 | 32 | 258 | 25 | 40 | 256 | 67 |
18F-FDG, 18F-fluorodeoxyglucose; MR, magnetic resonance; PET, positron emission tomography
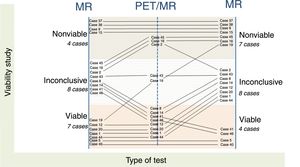
In the patient-by-patient analysis, MR studies yielded a diagnosis of myocardial viability in 7 patients and nonviability in 4, with 8 inconclusive studies, whereas PET findings indicated viability in 4 patients and nonviability in 7, with 8 inconclusive studies (table 3). In the comparison of MR and PET separately, there were 9 discordant cases: in 3 patients (cases 1, 20, and 44), MR indicated viability based on preserved contractility and absent or minimal enhancement, whereas PET was inconclusive; in 5 other patients (cases 12, 16, 41, 45, and 46), the hybrid technique was helpful by integrating segmental abnormalities, intermediate enhancement, and 18F-FDG uptake <50%; and in 1 patient (case 19) the data obtained were inconsistent. In 4 patients the diagnosis was inconclusive by both MR and PET (cases 2, 8, 14, and 43) and fusion was helpful in 3 of them. In 6 patients (cases 5, 9, 15, 37, 38, and 40) PET/MR did not provide additional information. Therefore, integrated PET/MR was useful in 42.1% (8/19) of patients in the coronary group. Among cases in which the diagnosis was inconclusive by MR (n=8) or by PET (n=8), PET/MR reclassified 87.5% (7/8) to a conclusive diagnosis with respect to MR and 87.5% (7/8) with respect to PET; that is, 87.5% (14/16) of inconclusive cases by both techniques. The contribution of PET/MR in the diagnosis of myocardial viability in our series is shown in figure 3.
Usefulness of the PET/MR diagnosis compared with the diagnostic performance of MR or PET separately, evaluated by patient
| Indication (n=19) | Diagnosis by MR | Diagnosis by PET | Usefulness of PET/MR | |
|---|---|---|---|---|
| 1 | Viability | Viable | Inconclusive | Not useful: MR supports viability |
| 2 | Viability | Inconclusive | Inconclusive | Useful: PET/MR does not support viability |
| 5 | Viability | Viable | Viable | Not useful: redundant information |
| 8 | Viability | Inconclusive | Inconclusive | Useful: PET/MR supports viability |
| 9 | Viability | Nonviable | Nonviable | Not useful: redundant information |
| 12 | Viability | Viable by enhancement (but with segmental abnormalities) | Inconclusive (but normal uptake predominates) | Useful: PET/MR supports viability |
| 14 | Viability | Inconclusive | Inconclusive | Useful: PET/MR supports viability |
| 15 | Viability | Nonviable | Nonviable | Not useful: redundant information |
| 16 | Viability | Inconclusive (but inferior akinesia) | Nonviable (but only 2 segments with no uptake) | Useful: PET/MR does not support viability |
| 19 | Viability | Viable | Nonviable | Not useful: inconsistent information |
| 20 | Viability | Viable | Inconclusive | Not useful: MR supports viability |
| 37 | Viability | Nonviable | Nonviable | Not useful: redundant information |
| 38 | Viability | Nonviable | Nonviable | Not useful: redundant information |
| 40 | Viability | Viable | Viable | Not useful: redundant information |
| 41 | Viability | Inconclusive | Viable | Useful: PET/MR supports viability |
| 43 | Viability | Inconclusive | Inconclusive | Not useful: information inconsistent |
| 44 | Viability | Viable | Inconclusive | Not useful: MR supports viability |
| 45 | Viability | Inconclusive | Nonviable | Useful: PET/MR supports nonviability |
| 46 | Viability | Inconclusive | Viable | Useful: PET/MR supports viability |
| Indication (n=18) | Diagnosis by MR | Diagnosis by PET | Usefulness of PET/MR | |
|---|---|---|---|---|
| 3 | Infiltrative | Inconclusive | Inconclusive | Useful: PET/MR does not support sarcoidosis |
| 4 | Infiltrative | Inconclusive | Inconclusive | Useful: PET/MR helps guide biopsy, but no diagnosis |
| 6 | Pericardium | Inconclusive | Inconclusive | Useful: PET/MR helps guide biopsy, but no diagnosis |
| 13 | Tumor | Inconclusive | Conclusive, indicates malignancy (but does not assess anatomic extent) | Useful: PET/MR indicates malignancy |
| 18 | Endocarditis (mechanical valve) | Inconclusive (but suspected perivalvular complication) | Conclusive (but does not locate or assess valve function) | Useful: PET/MR in possible endocarditis |
| 24 | Tumor | Conclusive, indicates malignancy (but does not assess metabolism) | Conclusive, indicates malignancy (but does not assess anatomic extent) | Useful: PET/MR indicates malignancy |
| 25 | Myocarditis | Inconclusive | Conclusive (but without spatial resolution) | Useful: PET/MR indicates recurrent myocarditis and guides biopsy |
| 26 | Tumor | Inconclusive | Conclusive, indicates no malignancy (but does not assess valve function) | Useful: PET/MR indicates no malignancy |
| 27 | Tumor | Inconclusive | Conclusive, indicates no malignancy (but does not assess cardiac infiltration) | Useful: PET/MR indicates no malignancy |
| 28 | Endocarditis (biological valve) | Inconclusive | Conclusive (but does not locate or assess valve function) | Useful: PET/MR possible endocarditis |
| 30 | Endocarditis (native valve) | Inconclusive | Conclusive (but does not locate or assess valve function) | Useful: PET/MR does not indicate endocarditis (there is no valvular uptake) and whole-body PET detects an abdominal tumor |
| 31 | Endocarditis (native valve) | Inconclusive | Conclusive (but does not assess the extent or valve function) | Useful: PET/MR does not indicate endocarditis (there is no valvular uptake) and whole-body PET detects an abdominal tumor |
| 32 | Endocarditis (mechanical valve) | Inconclusive | Conclusive (but does not locate or assess valve function) | Useful: PET/MR possible endocarditis (whole-body PET is useful for detecting septic embolism) |
| 33 | Tumor | Conclusive, indicates malignancy (but does not assess metabolism) | Conclusive, indicates malignancy (but does not assess cardiac infiltration) | Useful: PET/MR indicates malignancy |
| 34 | Myocarditis | Conclusive | Conclusive | Not useful: redundant information |
| 35 | Myocarditis | Inconclusive | Inconclusive | Useful: PET/MR negative for active inflammation, which indicates an old process |
| 36 | Tumor | Inconclusive | Conclusive, indicates no malignancy (but does not assess valve function) | Useful: PET/MR indicates no malignancy |
| 39 | Endocarditis (native valve) | Inconclusive | Inconclusive | Not diagnostic: negative for valvular uptake, but positive for peripheral uptake |
MR, magnetic resonance; PET, positron emission tomography
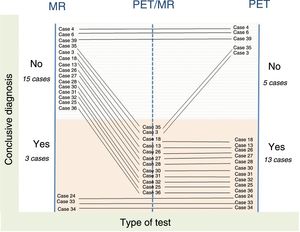
PET/MR was useful in 88.9% (16/18) of studies: in 13 it provided additional data for the diagnosis and in 3 it aided a biopsy procedure. There was no added value in only 2 patients, 1 with myocarditis (case 34, because of redundant information) and 1 with native valve endocarditis (case 39). The case-by-case usefulness of PET/MR is shown in table 3. MR suggested malignant disease in 2 cases of tumors, but without conclusive metabolic information, whereas PET provided information in 6 patients, although spatial resolution was limited to assess anatomic extent and cardiac infiltration; hence, fusion with MR images was required. None of the 6 patients with suspected endocarditis had an inconclusive diagnosis on MR imaging. PET provided information in 5 of these patients, but fusion with MR was needed because of poor resolution; in addition MR provided information on valvular and ventricular function, and possible perivalvular complications. In patients with myocarditis, MR was useful in 1 of the 3 cases included and PET was helpful in 2 by showing active foci; anatomic fusion with MR was also beneficial. The performance of each technique separately was poor in infiltrative disease and pericardial disease, whereas integration of anatomic and metabolic images was helpful for guiding biopsy and ruling out active disease. In summary, MR yielded 83.3% (15/18) of inconclusive cases and PET 27.8% (5/18), with high diagnostic value. Among the inconclusive cases by MR or PET, PET/MR reclassified 80% (12/15) to a conclusive diagnosis with respect to MR and 40% (2/5) with respect to PET. That is 70% (14/20) of inconclusive cases by both techniques (figure 4).
Agreement was found to be excellent in the analysis comparing PET/MR findings vs the results of PET or MR alone in individual patients in both the groups studied (κ=0.913). Furthermore, in 10 patients in the coronary group and 16 in the noncoronary group with diagnostic confirmation over follow-up, PET/MR provided an accurate diagnosis in 8 (80%) and 14 (87.5%) patients, respectively (). Hence, agreement was high between the viability diagnosis provided by PET/MR and the findings on clinical follow up in the coronary group and the same was true for the findings in noncoronary patients.
DISCUSSIONThis study describes the first clinical experience in Spain implementing hybrid PET/MR technology to assess cardiovascular disease, with an analysis of its usefulness. We found that cardiac PET/MR is feasible for this purpose and can help with the diagnosis and treatment in some patients—especially those with inconclusive findings on MR or PET—by integrating anatomic, functional, and metabolic information, and favoring an interaction between imaging specialists from different disciplines. PET/MR proved to be particularly useful for the study of cardiac masses and inflammatory or infectious conditions, being of help in 90% of cases, while MR alone had limited value. In patients with coronary disease, this technique improved the diagnosis in 42% of cases, particularly those showing intermediate enhancement, where functional recovery may be variable,13 and in cases showing severe hypometabolism.
The literature contains few reports on the clinical value of integrated PET/MR systems, although there are a large number of reviews on their application in cardiovascular disease, indicating that it is a promising technology. There is considerable evidence that PET and MR separately are both valid techniques for establishing the diagnosis and prognosis of ischemic heart disease,19,20 showing a good correlation in predicting postinfarction functional recovery.21 Nonetheless, data from the 2 techniques can be inconsistent: scar tissue may be detected on delayed-enhancement MR images in up to 11% of patients while 18F-FDG PET shows normal uptake.22 In other studies, not specifically focused on this objective, concordance was 80% between the findings of hybrid PET/MR technology and those of PET or MR separately.17,18,22,23 These results are consistent with our finding of 79% concordance between MR and PET for defining segmental viability. In the patient-by-patient analysis of viability, a large number of cases (11/19) did not benefit from fusion of the 2 techniques because MR alone or PET alone provided conclusive information. Although the study sample was limited, these results question the usefulness of PET/MR technology in chronic coronary disease. We found that the greatest value of the hybrid technique was in patients with inconclusive findings in MR or PET images, where integration of parameters obtained by MR such as myocardial thinning and regional contractility with PET findings of the degree of uptake-metabolism helped define the presence or absence of myocardial viability, in line with previous evidence.22 For example, most segments with intermediate transmural enhancement on MR imaging (inconclusive viability) showed normal uptake on PET, findings consistent with those of other studies.17,18 This observation is likely related to the transmural enhancement index being closer to 50%, which indicates viability.
In the noncoronary group, PET/MR showed greatest value in the study of cardiac masses, endocarditis, and myocarditis. PET was of help to determine whether masses were benign or malignant, but fusion with anatomic MR images was needed to precisely locate the lesions, determine their extent and degree of infiltration into adjacent structures (myocardium, valvular apparatus), and establish their morphological and tissue characteristics.24 In endocarditis, the greatest contribution of PET/MR was from PET, which enabled detection of systemic neoplasms and identification of active foci of valvular, perivalvular, and systemic inflammation in patients with mechanical or biological valves. However, fusion with MR images was crucial to locate the metabolic lesions detected by PET and evaluate their repercussion on valvular and ventricular function, parameters that determine the prognosis of surgery. Given the known value of PET/CT in the diagnosis of endocarditis,25 above all in patients with mechanical prostheses where MR has artifact limitations, it would be of interest to conduct larger studies specifically designed to assess the diagnostic value of PET/MR vs PET/CT. In myocarditis, the PET/MR combination was useful to identify active foci and guide biopsies, although it has shown lower value in chronic states.26
Our study has the added value of simultaneous acquisition of PET/MR images on a totally integrated system, a product of technological advances in recent years27 that improves spatial correlations and accelerates acquisition time. Formerly, PET and MR image acquisition was performed sequentially, as it was impossible to integrate the 2 techniques in a single system. Images were then fused in the postprocessing step. This procedure can lead to errors caused by imprecise alignment of images that have been acquired with differing cardiac and respiratory synchronization in the 2 studies, and it limits correction of the raw PET data.28
Our experience highlights the importance of proper patient preparation before the examination and the PET/MR protocol for evaluating myocardial viability. In our series, 6 studies (5 coronary and 1 noncoronary) of the 49 performed could not be assessed because of inadequate myocardial uptake or suppression of radiotracer. To assess viability, the patient should be in a state of hyperinsulinemia to achieve a suitable concentration of radiotracer in the healthy myocardium (presence of signal) and a deficit of radiotracer in the affected myocardium (absence of signal). These conditions were difficult to achieve in diabetic patients and those receiving corticosteroids, and the images obtained were not evaluable. Hence, patient selection for the test should be done with special caution. To assess inflammation, carbohydrate-free, fat-rich food intake is needed to suppress the physiologic 18F-FDG uptake of healthy myocardial cells (absence of signal) and visualize only uptake by active cells (presence of signal). Inadequate myocardial preparation makes interpretation of the images difficult; hence the interaction between the professionals involved is essential.
We believe that 2 factors improve the technique in diagnostic PET/MR: first, the technological advances that enable simultaneous acquisition of anatomic, functional, and metabolic images; and second, the teamwork combining knowledge from different expert imaging specialties, which goes beyond the technological capabilities provided by the systems.
LimitationsAmong the limitations of the study, we mention the difficulty of defining a patient's condition as being viable or nonviable because the cardiac segments analyzed could have different degrees of transmurality or metabolism. However, we sought a simple classification system to facilitate interpretation of the findings and comparison between the techniques when offering a diagnosis to guide a patient's treatment, as is done in clinical practice. Discrepancies in which segments showed hypometabolism and no enhancement may be related to the poor spatial resolution of PET, which tends to magnify hypocaptant areas when evaluated only by this technique.7 In these cases, MR provides better definition of the extent of damage; thus, spatial resolution is improved by combined PET/MR.
The design of our analysis (comparison of MR and PET studies evaluated separately with the PET/MR study by consensus) could be considered a limitation, as joint image reading might make it difficult to separate the value of the technique itself from the added value of the interaction between imaging specialists. However, this type of analysis reflects standard practice in the interpretation of hybrid studies that implicate different imaging modalities.
Another limitation is the small number of studies included and the technical problems of the raw PET data a posteriori in relation to the learning curve, inherent to a new technology. Nonetheless, we believe it is of interest to describe our experience considering the limited available evidence on the clinical and scientific development of PET/MR in cardiology, this being the first published experience in Spain.
Although the inclusion of diverse diseases (coronary and noncoronary) in the same study may seem to be a weakness, with the added difficulty of there being no single reference pattern common to all of them, our objective was to evaluate the usefulness of PET/MR in clinical practice and contribute to consolidating its indications in cardiology, which are still to be defined. The diagnostic confirmation over follow-up enabled evaluation of the diagnostic performance of PET/MR. In the future it will be necessary to carry out cost-effectiveness studies with a larger number of patients and a longer follow-up to monitor clinical and experimental situations where this new diagnostic tool can provide the greatest benefits and cost value.
CONCLUSIONSIn our series, multimodal PET/MR technology provided added value and complemented each separate technique in the diagnosis of some patients with cardiovascular disease, particularly infectious and inflammatory diseases and tumors in patients with inconclusive findings on MR or PET. In our experience, the main advantages of PET/MR are the possibility of simultaneous image acquisition, integration of anatomic/functional images (MR) with metabolic images (PET), and the interaction between different expert imaging professionals. Adequate patient selection and preparation is essential and cost-effectiveness studies are needed in this line.
FUNDINGL. Fernández-Friera, A. Moreno-Arciniegas, and L. Anmad Shihadeh received financial support from the Community of Madrid (AORTASANA-CM; B2017/BMD-3676), European Social Fund (ESF). L. Fernández-Friera received funding from Instituto de Salud Carlos III (PI15/02019), Madrid, Spain.
CONFLICTS OF INTERESTNone to declare.
- -
PET/MR is an emerging hybrid technology in diagnostic imaging that combines the anatomic, functional and metabolic information obtained by PET and MR in fused images. Real-life clinical experience in its use is limited.
- -
This study is the first to assess the usefulness of PET/MR in the diagnosis of coronary and noncoronary cardiovascular disease, using a practical clinical focus and analyzing the added value of the technique compared with PET and MR imaging separately. In addition, it provides detailed information on the PET/MR method (design, preparation protocol, acquisition, and analysis) based on our experience in a setting where there are no previous studies describing its implementation.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2020.06.034