In December 2019 a novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was described among patients presenting with pneumonia symptoms in the city of Wuhan, China. With an overall case fatality rate of 2% to 3%, the coronavirus disease (COVID-19) has developed into a worldwide pandemic, becoming endemic in Europe in early March 2020.1 As of June 4, 2020, SARS-CoV-2 infection has already affected over 6.5 million people and has caused more than 380 000 casualties worldwide.2 Men of middle age and older are most commonly and severely affected, but individuals of any age can acquire COVID-19. Although most infections are not severe, the spectrum of symptomatic infection ranges from mild to critical. Among patients with a critical course of the disease, the main clinical findings are bilateral pneumonia, acute respiratory distress syndrome, heart failure, septic shock, and multiple organ dysfunction.3–5 Furthermore, COVID-19 often develops into a systemic inflammatory disease with an impact on the vascular and hematopoietic system and hypercoagulability is common among hospitalized COVID-19 patients.5
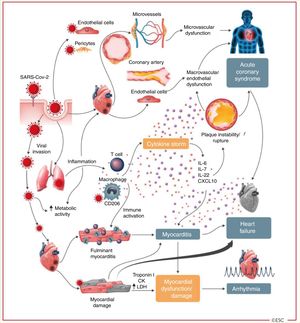
SARS-CoV-2 may interact with the cardiovascular system on multiple levels, increasing morbidity in patients with underlying cardiovascular conditions and provoking myocardial injury and dysfunction6 (figure 1).7 Since the early stages of the pandemic, higher mortality rates among COVID-19 patients with acquired cardiovascular disease, such as hypertension, coronary artery disease or diabetes, have been reported compared with patients without acquired cardiovascular disease, and heart failure may be precipitated by acute illness in patients with pre-existing cardiovascular disease.8
Cardiovascular involvement in COVID-19 – key manifestations and hypothetical mechanisms. SARS-CoV-2 anchors on trans-membrane angiotensin-converting enzyme-2 to enter the host cells including type-2 pneumocytes, macrophages, endothelial cells, pericytes and cardiac myocytes leading to inflammation and multi- organ failure. Infection of endothelial cells or pericytes is of particular importance because this could lead to severe microvascular and macrovascular dysfunction. In addition, immune over-reactivity can potentially destabilize atherosclerotic plaques and explain the development of acute coronary syndromes. Infection of the respiratory tract, particularly type-2 pneumocytes, by SARS-CoV-2 is manifested by the progression of systemic inflammation and immune cell over-reaction leading to “cytokine storm”, resulting in increased levels of cytokines such as IL-6, IL-7, IL-22 and CXCL10. Subsequently, it is possible that activated T cell and macrophages may infiltrate infected myocardium resulting in the development of fulminant myocarditis and sever cardiac damage. This process may be further intensified by a cytokine storm. Similarly, the viral invasion my case cardiac myocyte damage directly leading to myocardial dysfunction and contribute to the development of arrhythmias.6 Reproduced from the original work “ESC Guidance for the Diagnosis and Management of CV Disease during the COVID-19 Pandemic” https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance.7 Permission obtained from © The European Society of Cardiology 2020. All rights reserved.
Over the past few decades, a new cardiovascular population of adults with congenital heart disease (ACHD) has emerged in developed countries due to medical and surgical advances. Unfortunately, a complete cure of congenital cardiac defects in childhood is exceptional and many of them face a life-long increased risk in cardiovascular complications (such as heart failure, arrhythmias, pulmonary circulation disorders, and even death) due to hemodynamic residuae9,10 or sequelae of previous repair strategies. Therefore, it is reasonable to assume that some of these ACHD patients will be at increased risk of adverse outcomes if they contract COVID-19.
ACHD patients now outnumber children with congenital heart disease (CHD). The available evidence suggests an overall ACHD prevalence of about 3000 per million. Included in this group are patients with “mild” defects (eg, repaired atrial septal defect or ligated ductus arteriosus), but most have moderate or severe CHD whose natural history has been forever changed by therapeutic interventions. Analyses of registry data of adults with various forms of CHD from Spain and Switzerland have allowed for detailed phenotyping of patients followed by ACHD referral centers. With a median [interquartile range] age of 35 [25-45] years, 24% and 44% of patients in the Spanish Registry are classified as having moderate or severe CHD, respectively, and 32% as having mild defects.11 In the Swiss Adult Congenital Heart Disease Registry (SACHER), up to 16% of 2836 patients had cyanotic or other complex congenital heart disease, 15% had lesions affecting the right heart (ie, tetralogy of Fallot or Ebstein anomaly), 13% had complex diseases of the left ventricular outflow tract, 25% had valvular lesions, and 22% had a shunt pathology.12 As expected, most Spanish and Swiss ACHD patients had undergone previous repair procedures (77% and 71%, respectively) and 47% of those had had 1 or more reinterventions.11,12
When considering the potential outcome of COVID-19 in ACHD patients, competing risks have to been taken into account. First, age per se is an independent risk factor for COVID—19-related mortality.13,14 Immune responses in older adults are slower, less coordinated, and less efficient than in younger adults, making them more susceptible to coronavirus infections.15 In addition, circulating plasma concentrations of angiotensin-converting enzyme II are higher in adults than children and are also higher in men than in women.16 COVID-19 invades cells by binding to angiotensin-converting enzyme II, which is expressed on the surface of alveolar cells in the lungs, making older men potentially vulnerable to SARS-CoV-2. On the other hand, typical ACHD patients with their median age of 35 years may be less susceptible or have a milder COVID-19 course, due to the protective effects of their age, independently of the underlying defect complexity. In addition, although the number of ACHD patients older than 60 years is steadily increasing, acquired cardiovascular risk factors for fatal COVID-19 outcomes are infrequently found in the ACHD population. In the Spanish cohort, 75% of patients were younger than 45 years, and the prevalence of hypertension, diabetes and ischemic heart disease was only 14%, 2.7%, and 1.5%, respectively (unpublished data). Thus, many ACHD patients without major comorbidities may not be at higher risk for a poor outcome if they contract COVID-19 than the corresponding general population.
Second, several common cardiac defects predominantly affect the contractility of the right ventricle, eg, tetralogy of Fallot, pretricuspid shunts leading to right ventricular volume overload, Ebstein anomaly, pulmonary stenosis, and right ventricular pressure overload due to shunt-induced pulmonary hypertension. These patients may have an impaired contractile reserve of their subpulmonary ventricle, rendering them potentially more hemodynamically unstable in the presence of bilateral pneumonia or acute respiratory distress syndrome caused by SARS-CoV-2. Another group of patients deemed at increased risk are those with univentricular physiology after Fontan palliation. These patients do not have a subpulmonary ventricle and pulmonary blood flow depends on an unobstructed pulmonary vascular bed. Bilateral pneumonia could have detrimental effects on pulmonary blood flow and ventricular preload. This is why vaccination for seasonal influenza and pneumococcal disease is highly recommended in these patients.17
Third, among ACHD patients, those with chronic cyanosis are at high risk for both thromboembolic events and hemorrhagic complications. Since individuals with COVID-19 may have a number of coagulation abnormalities and hypercoagulability appears to adversely impact prognosis, close monitoring for clinical signs of thrombosis or bleeding should be advised in all cyanotic individuals with COVID-19 with severe or unusual presentations.
Fourth, other ACHD-associated comorbidities such as lung disease, liver impairment, renal failure and immunodeficiency associated with genetic disorders may have a negative impact on outcomes in COVID-19 infection.
In the absence of observational studies, these different CHD-related confounders of COVID-19 disease course make risk stratification for adverse outcomes highly challenging. Even if drastic preventive measures such as a lockdown of public life have proven effective in fighting the pandemic in many European countries, the socioeconomic burden of these actions in terms of loss of workforce and economic activity, as well as social isolation, is huge. Therefore, we need reliable tools to identify ACHD patients at risk for poor COVID-19 outcomes that are useful for guiding preventive actions and follow-up protocols. In this context, close collaborations on a national and international level are the key to success. In this regard, the community of ACHD experts has set in motion 2 collaborations. The International Society for Adult Congenital Heart Disease has endorsed a research initiative by Dr Aboulhosn (University of California, Los Angeles, USA) aiming to develop a database of ACHD patients who have tested positive for SARS-CoV-2. These database will collect detailed clinical CHD-related data and hopefully allow a refined risk stratification based on anatomical and functional data.In addition, a research initiative within the European Collaboration for Prospective Outcome Research in Congenital Heart disease (EPOCH)18 has been started to collect COVID-19 cases among ACHD patients across Europe and to share the outcome data of these cases on a weekly basis among all participating centers. To date (27 May), 23 centers in Austria, Belgium, Denmark, France, Germany, Italy, the Netherlands, Spain, and Switzerland are participating in the study. These centers care for more than 40’000 ACHD patients. An analysis of the data collected between 30 March and 25 Maywill be published in the near future and will hopefully provide the first clue on the overall burden of COVID-19 in ACHD patients.
Until we can base our risk stratification on outcome data, expert panels may play an important role in advising us how to harmonize risk stratification in ACHD patients during the current pandemic. In this respect, the Working Group on ACHD of the European Society of Cardiology is currently drafting a position paper. Another manuscript describing an aid for risk stratification based on a survey among 24 experts of the 23 participating centers of the project (EPOCH) has been submitted. Meanwhile, we all are required to stay alert and to start thinking about potential improvements and steps to take in order to adapt our clinical practice to the new situation. Overall, the COVID-19 pandemic is not only a medical challenge but also a chance for improvement.
Regular ACHD outpatient visits in tertiary care centers all over Europe have been canceled to concentrate the medical resources on the fight against the pandemic and stop its spread. For patients with complex chronic conditions, as it is the case for many ACHD, interrupting regular follow-up visits may result in a delayed diagnosis of CHD complications and thus delay appropriate management, with a potentially direct effect on morbidity and mortality. We know from young ACHD patients with loss of follow-up during the transition period from pediatric to adult care that a lapse of care is associated with more late complications and a higher need for urgent cardiac interventions.19 The desire to minimize the risk of coronavirus exposure for a given ACHD patient must obviously be weighed against the need for in-person visits, particularly in those with decompensated congestive heart failure or arrhythmias. If possible, scheduled clinic visits should be converted to telehealth visits. Accustomed since their childhood to being surrounded by technological devices, the young ACHD population may be particularly inclined to the use of mobile health technologies. A wide range of clinical data, including visual examination, auscultatory sounds, physiological parameters and echocardiographic images, can be transmitted in real-time across telemedicine links, facilitating accurate diagnosis, effective decision making and promoting access to specialist opinion. Such telemedicine programs can continue to provide state of the art, high quality, personalized care for individuals in the community beyond the coronavirus pandemic.
In conclusion, the current COVID-19 pandemic poses unprecedented challenges and changes to both patients and specialists. Assumptions derived from theoretical reasoning and extrapolation of data from patients with acquired heart disease might not be sufficiently accurate for risk stratification in ACHD. Predicting the risk of poor outcomes remains challenging due to the variety of cardiac defects and repair strategies. The COVID-19 pandemic may represent a special burden for patients with severe CHD, such as cyanotic patients, patients with overt heart failure or associated pulmonary vascular disorders, and the involvement of other organs may adversely impact the prognosis. However, fairly young ACHD patients without comorbidities may not be particularly vulnerable to COVID-19. Since they are also exposed to the potentially far-reaching socioeconomic impact of this pandemic, our recommendations for these patients needs to be based on sound clinical evidence. Therefore, national and international collaborations aiming to address this issue must be fostered and are on their way.
CONFLICTS OF INTERESTF.J. Ruperti-Repilado and M. Schwerzmann have no potential conflicts of interest to declare. P. Gallego is associate editor of Revista Española de Cardiología. The journal's editorial procedure to ensure impartial handling of the manuscript has been followed.