Keywords
INTRODUCTION
In the measurement of blood pressure (BP) the white coat phenomenon (WCP) is considered to be present when the difference in systolic BP/diastolic BP between the measurement taken in the doctor's office and that recorded on ambulatory monitoring is greater than 20/10 mm Hg, respectively. This phenomenon may interfere in daily practice and in the evaluation of the degree of blood pressure control required. These absolute differences correspond to what is referred to as the white coat effect (WCE). Numerous studies over the last twenty years,1-3 especially those with a transverse design performed in specialized hospital settings, have confirmed the importance of the WCE in persons with hypertension. This WCE may explain why some persons who are considered to have hypertension in fact have a normal BP outside the doctor's office, classified as white coat hypertension (WCH).4 This effect may also overestimate the true degree of hypertension in patients with high BP measurements, both in and away from the office (WCP).5 Many aspects related to the WCE remain unknown or unclear and are currently the subject of debate among experts.
The use of systems for ambulatory blood pressure monitoring (ABPM) in patient care and in research and has so far been done almost exclusively within the hospital setting and in selected patients. The magnitude of the WCE in the primary care setting, however, where most patients with hypertension are detected and controlled, is less well known. We therefore undertook a study, carried out in an urban health care center, to evaluate the WCE in a group of patients with hypertension who were diagnosed, treated and followed in primary care. A second objective was to assess the effect of withdrawal of antihypertensive therapy on the pressor response (prevalence of WCE, WCH and WCP) and the concordance between BP in the office and the ambulatory BP.
PATIENTS AND METHODS
Patients
The study included a simple random sample of 70 patients with hypertension between 1997 and 2001, all from the Centro de Salud Universitario San Pablo, in Seville, Spain. The confidence level was 95%, the precision 0.10 and the expected prevalence of the WCE was 25%.6,7 All the patients met the following criteria:
Essential light or moderate hypertension (grade 1 or 2 of the JNC VI classification),8 no signs or symptoms of visceral repercussion (phase I of the WHO classification).9 The JNC VII grades 2 and 3 have recently been combined.10
Age older than 18 years.
Received antihypertensive therapy with 1 or 2 drugs maximum continuously for at least one year prior to the study.
Good BP control for the 12 months prior to inclusion in the study (mean systolic and diastolic BP taken in the office of ≤140 and ≤90 mm Hg, respectively). At least 6 BP measurements were required to be registered in their charts during the previous year.
No arrhythmias, no chronic decompensating or debilitating processes and no physical or psychological limitations for ABPM.
Written informed consent to the study.
In order to rule out any involvement of target organs or secondary hypertension, a detailed clinical history was taken from all the patients, including the presence of associated cardiovascular risk factors (alcoholism, body mass index and smoking). A general laboratory study was also made which included a blood test, biochemical values, lipid and ion profiles, and elemental urine with sediment and microalbuminuria. A chest x-ray was done, as well as an electrocardiogram and a study of the fundus of the eye. No echocardiogram was performed due to the limitations of the study in a primary care setting. Patients were excluded if they had documented complications attributable to hypertension, such as stroke, angina or myocardial infarction. We verified the constancy of the BP measurements (at least 6 recordings during the previous year) to confirm good BP control with pharmacological therapy. Blood pressure measurements were taken under conditions recommended by the various consensus agreements and international organizations.8,9,11
Methods
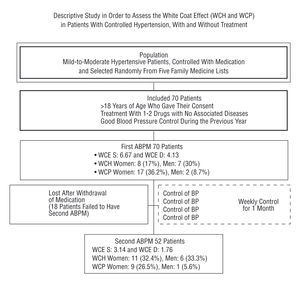
The study had a descriptive design, with a first period where the BP was well-controlled with pharmacological agents, and a second period during which these agents were withdrawn. All the patients underwent two 24-hour ABPM recordings during a normal working day. The initial recording was made at the start (first phase), when the patient was taking the usual antihypertensive medication, and the second recording (second phase) was made four weeks after stopping treatment with antihypertensive agents. Two periods were programmed, one daytime and one night-time (Figure 1).
Fig. 1. General scheme of the study. WCE S indicates systolic white coat effect; WCE D, diastolic white coat effect; WCH, white coat hypertension; WCP, white coat phenomenon; BP, blood pressure.
Both ABPM recordings were made with a SpaceLabs 90207, which measures by oscillometry and which had been validated previously.12,13 The validation was undertaken following the British Hypertension Society protocol for the evaluation of BP measuring devices.14
The monitor was programmed to obtain measurements of BP and heart rate each 20 min between 08:00 and 23:59 hours, and each 30 min between 00:00 and 07:59 hours. The program was based on the recommendations for a registry interval of 15-30 minutes during the day and 20-30 minutes at night.15 An analysis of the night-time dipper effect in BP has recently been published.16 Several other groups17-19 also recommend this programming rate. Shorter daytime intervals interfere with the daily activities of the person being monitored and would not be representative of daily life, and night-time differences are so small compared with shorter intervals that each 30 minutes during the night is adequate and does not interfere excessively with sleep.
For instrument calibration, three measurements were made with a mercury sphygmomanometer alternating with three measurements with the monitor, in the same arm and with the patient seated. Mean differences in the systolic and diastolic BP between the two methods of ±5 mm Hg were considered valid.20 If this difference was not fulfilled, calibration was repeated the following day when the monitor was taken away.
Each patient was given instructions concerning the following aspects:17
Perform the usual daily activities on the day of the control, avoiding any sporting activity.
Remain still each time the cuff inflates for a measurement.
Make a diary note of the time, position and activity being performed at the time of each measurement (siesta, going to bed, waking up, number of awakenings during the sleeping period, etc), although any of the methods for estimating ambulatory BP, such as intervals, standard or minidiaries, provide adequate evaluation of the period of activity.21
Incorrect readings were automatically eliminated by the system software (systolic BP >260 or <70 mm Hg and a diastolic BP >150 or <40 mm Hg; pulse pressure >150 or <20 mm Hg and heart rate >200 or <20 bpm). Visual inspection of the full list of readings enabled manual elimination of inconsistent increases or reductions in systolic or diastolic BP (30% or more difference compared with the previous or next reading). Registries were considered technically valid if they had at least 50 readings overall (about 80% of the theoretical 24 hour total) and at least one reading per hour during the waking period.
Statistical Analysis
The following BP variables were considered:
Casual BP: during phase 1 (patient taking usual pharmacological therapy), the mean of all the control BP measurements, during visits to the doctor and by the nurse, during the previous 12 months. The calibration mean was also considered to be a control measurement. During phase 2 (four weeks with no pharmacological antihypertensive therapy), the mean of all the control BP measurements in the office together with the calibration mean.
Ambulatory BP: although the means ± standard deviation of the whole day as well as of the daytime (waking) and night-time (sleeping) periods were calculated and evaluated at both controls, the ambulatory BP reading was considered to be the mean for the patient's active period, individualized according to the data in each person's diary. Normal BP values were considered to be ≤135 mm Hg systolic and 85 mm Hg diastolic at the same time.10,15,22
White coat hypertension: hypertension in the office (casual systolic BP≤140 mm Hg or casual diastolic BP≤90 mmHg) and normotension on ABPM (mean systolic BP during the active period ≤135 mm Hg and mean diastolic BP≤85 mm Hg, at the same time).15,22
White coat phenomenon: a difference between the casual BP and the ambulatory BP>20 mm Hg for systolic BP or >10 mm Hg for diastolic BP,23 independently of whether the patient was in pharmacological treatment phase 1 or phase 2 of the study.
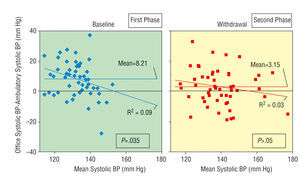
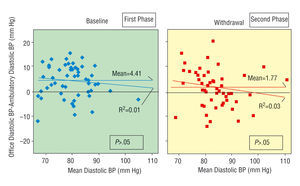
For each phase of the study the prevalence of the WCE was calculated, with its 95% confidence interval (CI). Comparison of means was done with Student's t test for paired data, and a non-parametric test when the quantitative variables did not follow a normal distribution. Comparison of the qualitative variables was done with the χ2 and McNemar tests. In both cases levels of significance were established at 5%. Analysis of the results was undertaken with the SPSS, version 10. Concordance between the casual BP and the ambulatory BP was evaluated by the method proposed by Bland and Altman24,25 (Figures 2 and 3).
Fig. 2. Concordance charts of systolic blood pressure. *Representation of the differences between the methods in relation with their mean.
Fig. 3. Concordance charts of diastolic blood pressure. *Representation of the differences between the methods in relation with their mean.
RESULTS
Of the 70 persons with hypertension who were initially enrolled, 52 (18 men and 34 women) completed the study and had the double control measurements after the 4-week washout period with no pharmacological antihypertensive treatment. The reasons for not completing the study were: unacceptable BP values after withdrawing the medication (n=9), a high percentage of errors in the second ABPM (n=5), refusal to have the second ABPM (n=3) and personal decision to restart antihypertensive therapy (n=1). The mean age of the subjects studied was 60.1±10.3 years (women: 59.4±9.6 and men: 61.4±11.6 years).
Analysis of the Pressor Response According to the Phase
Figure 1 shows that the WCE was greater during the first phase (systolic WCE: 6.67, diastolic WCE: 4.13) than the second phase (3.14 and 1.76).
White coat hypertension during the first phase was detected in eight women (17% of the women) and seven men (30% of the men). This represented 21.4% of all the patients compared with 33% in the second phase.
During the first phase the WCP was seen in 19 of the 70 patients (27% total; 36.2% of the women and 8.7% of the men), whereas during the second phase the WCP was only detected in 10 patients (5.6% of the men and 26.5% of the women).
Comparative Analysis of the Pressor Response in the 52 Patients Who Completed the Study
In phase 1 (with treatment) the systolic WCE (8.1 vs 3.1) and the diastolic WCE (4.3 vs 1.7) were significantly higher than in phase 2 (Table 1).
Interestingly, 14 patients who did not have WCH during the first treatment phase were diagnosed with WCH after 4 weeks without treatment (Table 2), whereas 10 patients with the WCP during the first phase did not have WCP in the second phase (Table 3).
TABLE 2. Comparative Analysis, According to Study Phase, of White Coat Hypertension (WCH)
The analysis according to sex only showed significant results for the systolic WCE in women (Table 4).
The percentage of persons with WCH remained the same after stratifying by sex. Perhaps interestingly, 9 women and 5 men who did not have WCH during the first phase did have WCH during the second phase (Table 5).
Regarding the WCP, most of the men remained the same whereas 9 women with the WCP in the first phase did not have it in the second phase (P=NS) (Table 6).
Concordance Between Office and Ambulatory Blood Pressure Measurements
The WCE was significantly (P=.035) related with lower systolic BP levels during the first phase but not during the second phase (Figure 2). No significant differences were seen for the diastolic BP; thus the WCE does not appear to be related with the diastolic BP level (Figure 3).
DISCUSSION
Although mean BP measurements were calculated at both controls for the full day as well as the daytime (waking) and night-time (sleeping) periods, the ambulatory BP was considered to be the mean of the active period, individualized according to the data in each person's diary. Normal BP values were considered to be ≤135 mmHg systolic and ≤85 mm Hg diastolic at the same time.10,15,22
The mean daytime measurement suffices to evaluate whether a person has hypertension because the quality of night-time readings varies greatly. Nevertheless, depending on whether there is or is not a night-time decrease in BP, this period can help us understand better the total load to which the patient is submitted.26
Interpretation of the Results of the First Phase of the Study
Inclusion of the calibration ABPM reading as one more control resulted in an increase in the mean BP, probably resulting from a sympathetic response to the placement of a strange instrument not previously seen by the patient. Moreover, the calibration was done by the lead investigator who, as a physician, provoked a greater WCE than that seen at the control readings, which were usually done by a nurse. Several studies indicate that nursing staff have less influence than physicians on BP readings.27,28 This may explain why the BP measurements in some of the patients initially selected to participate in the study were above the means established for a good control. Stratification by sex showed no significant differences, and sex had no apparent influence on the BP of the 70 patients included in the study.
Initial ABPM
Stratification by sex for the initial ABPM reading showed significant differences. The mean BP recordings during the active period were higher in the men, 9.3 mm Hg in the systolic BP and 7.5 mm Hg in the diastolic BP. The afternoon siesta (daytime sleep) could account in part for this difference, since the men were more likely to have a siesta than the women, who during this period after lunch (when the BP is usually lower) had a fall in the mean for the active period, whereas the reading for the men during the siesta was included in the sleep period, not the active period.29
Quantification of the Pressor Response28,30
As mentioned earlier, some patients with good BP control, and therefore initially included in the study, could surpass the study limits when the calibration readings were included, although the later ABPM showed ambulatory readings (active period) <135/85 mm Hg, therefore showing WCH.
Myers and Reeves23 studied the WCE in 71 patients receiving antihypertensive therapy, a very similar sample to those in our study. They found a WCP in 52 patients (73%), which contrasts with our findings, though this may be due to different selection criteria as their patients already had suspected WCP. Whatever the case, it seems clear that BP measurements made in the office may not represent the usual ambulatory BP in patients who are receiving chronic antihypertensive therapy.23,28,31
Interpretation of the Results of the Second Phase of the Study
As in the first phase, inclusion of the calibration reading in the second phase increased the means of the control measurements, again with no significant difference when stratified according to sex.
Second ABPM
Stratification by sex showed significant differences, with men having a higher mean BP in the active period for both systolic BP (10.2 mm Hg) and diastolic BP (7 mm Hg). As with the first reading, this difference may be explained by the siesta.
Quantification of the Pressor Response
Eleven women (32% of the women) and 6 men (33% of the men) had WCH in the second phase (Table 5), probably influenced by the greater effort of these patients to control their risk factors after withdrawal of their medication.
Different studies have estimated the prevalence of WCH in primary care to be between 35%32 and 43%,33 although the methodology used32 and a probable selection bias33 limit the worth of these estimates. The results of 2 population-based studies34,35 undertaken exclusively in men apparently disagree with the previous studies. In the first,34 the prevalence of WCH (14%) was different from that of the men in our study, probably due to the low sample number. In the second study,35 the ambulatory BP was above the casual BP in almost all the participants and the correlation between the two BP was excellent, probably because of the low number of hypertensive patients, most of whom were being treated and whose hypertension was well controlled.36
The WCE was much less marked in the ABPM of the second phase (systolic WCE: 3.14, diastolic WCE: 1.76). This may be because the ABPM readings were higher after four weeks with no antihypertensive treatment, with less difference with the control readings at withdrawal.
Interestingly, the WCP was detected less than in the first phase. This phenomenon was seen in 10 of the 52 patients studied in the second phase, which represents 19% (26.5% of the women and 5.6% of the men; Table 6). The explanation for this difference could be the same as that mentioned above for the WCE. Thus, the lack of statistically significant differences suggests that withdrawal of antihypertensive treatment does not modify the prevalence of WCH or the WCP.
Our group recently showed the qualitative and quantitative impact of the WCE in primary care, with the preliminary results published in 1997.7 In an unselected group of 152 patients with recently diagnosed and not yet treated hypertension, whose pressor response could therefore be compared with the response of our patients in the second phase, the casual BP overestimated the ambulatory BP by means of 13 mm Hg in the systolic BP and 5 mm Hg in the diastolic BP, with large individual differences, and according to sex and depending on the person taking the measurements. The prevalences of WCH and the WCP, however, were high (25% and 45%, respectively), especially in women. All these persons, independently of the results of ABPM, were recommended to undertake the usual follow-up for hypertension at their health centers (doctors' and nurses' offices). They were given instructions about non-pharmacological treatment and advised about measures to correct other associated cardiovascular risk factors. The decision as to whether to treat the hypertension was taken on an individual basis by each patient's family care physician, based mainly on the ambulatory BP readings and evaluation of the overall cardiovascular risk.
The final prevalence of WCH in our study was 33% (Figure 1). In consequence, 17 patients (11 women and 6 men) were no longer considered to have hypertension and their antihypertensive medication was withdrawn definitively, although their BP was still periodically monitored in the office.
Analysis of the influence of the different antihypertensive drugs on the WCE has also been the subject of a recently published report by our group.37
Comparison Between the First and Second Phases of the Pressor Response
Statistical tests to compare just the 52 patients who finished the study showed that the overall WCE was significantly greater in the first phase than the second (8.1 vs 3.1 and 4.3 vs 1.7 mm Hg for systolic and diastolic BP, respectively), both in women (10.9 vs 5.6 and 6.9 vs 3.7 mm Hg for systolic and diastolic BP, respectively) and in men (2.9 vs 1.6 and 1.2 vs 1.8 mm Hg for systolic and diastolic BP, respectively), although after stratification by sex the sample was reduced and only the systolic BP in women was significantly different.
These data confirm the greater likelihood of women to have the WCE suggested by Pickering et al4 and endorsed by others,7,28,38 though not all39,40 and not so marked as in our study.
Gender clearly appears to be an important factor in the white coat response. Attempts at explaining the white coat response by measurable psychological variables, such as stress or depression, show differences according to sex, whereas clinical variables were not as effective at predicting the white coat response.41
CONCLUSIONS
Withdrawal of antihypertensive medication in patients with well-controlled grade 1 or 2 hypertension failed to modify significantly the prevalence of the WCP and WCH, and the WCE was greater when the patients were receiving pharmacological agents. Of the patients who completed the study, 33% were classified as having WCH and their antihypertensive medication could be definitively stopped.
Full English text available at: www.revespcardiol.org
ABBREVIATIONS
BP: blood pressure.
WCE: white coat effect.
WCH: white coat hypertension.
WCP: white coat phenomenon.
ABPM: ambulatory blood pressure monitoring.
This project was made possible thanks to funds from the Consejería de Salud de la Junta de Andalucía (Grant to Proyectos de Investigación Expediente 83/92)
Correspondence: Dr. F. Villalba Alcalá.
San Benito, 7, Casa A 2.o B. 41018 Sevilla. España.
E-mail: francisco.villalba.sspa@juntadeandalucia.es