Atrial fibrillation (AF) is the most common clinically significant cardiac arrhythmia. P-wave duration and interatrial blocks (IAB) have been reported to be associated with AF. Our aim was to determine the individual and combined association of P-wave duration and advanced IAB morphology with AF.
MethodsWe designed an age-, sex-, and survey-matched case-control study nested in a population-based cohort (REGICOR: REgistre GIroní del COR). Two different surveys recruited a total of 9380 participants from 1999 to 2005; all participants were invited to a second examination between 2009 and 2013. For the present study, we selected participants aged 25 to 79 years with follow-up through the end of the study. All electrocardiograms were analyzed by 2 observers to determine P-wave duration and morphology (normal, partial, or advanced IAB).
ResultsThe median follow-up was 7.12 years. Eighty participants presented with AF, had a legible baseline electrocardiogram, and were included in the study, along with 160 controls. P-wave duration and the presence of partial or advanced IAB were associated with AF. When P-wave duration and morphology were considered together, only P-wave duration (≥ 110 milliseconds) showed an independent and strong association with AF. The odds ratio for AF of P-wave duration between 110-119, 120-129 and ≥ 130 milliseconds vs < 110 milliseconds were 5.33; 95%CI, 1.74-16.33, 5.08; 95%CI, 1.73-14.90 and 5.44; 95%CI, 1.95-15.15, respectively.
ConclusionsA P-wave longer than 110 milliseconds increases the risk of AF. Advanced IAB morphology did not seem to provide an additional AF risk beyond that of P-wave duration.
Keywords
Atrial fibrillation (AF) is the most common clinically significant cardiac arrhythmia1–3 and is associated with high mortality4 and morbidity and reduced quality of life.5 The prevalence and incidence of AF are high and increase with age.6–8 The costs and hospitalizations attributable to AF have risen markedly and a continued increase is expected, due to population aging.9,10
Clinical cardiovascular risk factors such as obesity, hypercholesterolemia, diabetes mellitus, and hypertension are associated with higher risk of AF.11–13 Some electrocardiographic characteristics have also been related to AF. Among them, P-wave duration and interatrial blocks (IAB) have been associated with AF risk in some studies.14–20 Interatrial blocks are recognized as an electrocardiographic abnormality based on the presence of a P-wave duration ≥ 120 milliseconds, called partial IAB, or ≥ 120 milliseconds with a biphasic P-wave morphology in the inferior leads, called advanced IAB.21,22 Interatrial blocks have also been associated with a higher risk of supraventricular tachyarrhythmias,23–26 and the confluence of IAB and this type of arrhythmias has been recently named the Bayés syndrome.27
The evidence of a relationship between AF and P-wave characteristics, both duration and morphology, in the general population is scanty. We hypothesized that long P-waves and the presence of advanced IAB are independently associated with the risk of AF. The aim of this study was to determine the individual and combined associations between 2 P-wave characteristics, duration and morphology, and risk of developing AF in a population-based study.
METHODSDesignWe designed a retrospective age-, sex-, and survey-matched case-control study nested in the REGICOR (REgistre GIroni del COR) cohort study. One of the REGICOR components is a prospective population-based cohort study carried out in Girona province (∼700 000 inhabitants) in northeastern Catalonia, Spain.28 Individuals living in the city of Girona and surrounding rural villages were randomly selected from the nearest census and invited to participate. Recruited participants were aged 25 to 79 years, had lived in the referral area for at least 6 months, were free of end-stage disease, and were not institutionalized. In this study, the participants in 2 different surveys undertaken in 1999 to 2001 and 2003 to 2005 were included. All these participants were invited to a second physical examination between 2009 and 2013. For the present study, we selected participants who attended the follow-up physical examination.
All participants developing AF during the follow-up of the cohort were selected. Two controls, matched by age (± 2 years), sex and survey cohort, were randomly selected for each case. The study protocol was approved by the local ethics committee and all participants signed an informed consent form.
Baseline ElectrocardiogramsA standard 12-lead electrocardiogram (ECG) recording was obtained for each participant in the baseline visit and was digitalized. Minnesota code (8.3.1) was applied to standardize the diagnosis of AF.29 A standardized protocol and settings (25mm/sec and 10mm = 1mV) were used for all the ECGs.
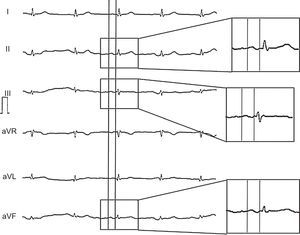
The P-wave duration and the presence of IAB were manually measured and assessed. To measure P-wave duration we analyzed the digitalized ECG images using the GeoGebra 4.2 software. We amplified the ECG image up to 20 times its original size to define the interval between the earliest and the latest detection of atrial depolarization in the frontal leads, defined as a positive or negative deflection, respectively, that deviates from the base line before the QRS complex (Figure 1). The software allows us to manually draw lines on the ECG and provides the distance between 2 points, which we later converted to milliseconds.
We defined partial IAB as a P-wave ≥ 120 milliseconds, and advanced IAB as a P-wave ≥ 120 milliseconds and a biphasic morphology in inferior leads (in lead II, the P-wave can only be positive with an isodiphasic final part).
The presence of premature atrial beats in the baseline ECG was also recorded. All the ECGs were analyzed by 1 observer (L.A. Escobar-Robledo), and reviewed by a second observer. If there was a discrepancy, a third observer verified the results. The intraindividual concordance of the P-wave duration measurement, assessed by reanalyzing 30 ECGs, was very high (intraclass correlation coefficient = 0.981; 95% confidence interval [95%CI], 0.960-0.991). The observers were blinded to the case or control status of the ECGs they analyzed.
Atrial Fibrillation During Follow-upAll participants were invited to attend a follow-up physical examination between 2009 and 2013. A standard 12-lead ECG recording was obtained for each participant and was digitalized. Minnesota code (8.3.1) was applied to standardize the diagnosis of AF.
Other VariablesIn both visits, examinations were performed by trained nurses using standardized measurement methods and the validated MONICA questionnaires.30,31 Body mass index was calculated as weight divided by squared height (kg/m2). Patients were considered hypertensive if previously diagnosed, under treatment, or presenting with systolic blood pressure ≥ 140mmHg or diastolic blood pressure ≥ 90mmHg. Fasting blood samples were taken and total cholesterol, high-density lipoprotein cholesterol, triglycerides and glycemia concentrations were determined. Diabetes was defined as history of diabetes, treatment, or fasting glycemia ≥ 126mg/dL. We also recorded the use of beta-blockers and drugs for diabetes and hypertension.
Statistical AnalysisStandard parametric and nonparametric methods were used to compare the characteristics of the participants with confirmed AF and the control group. The Pearson correlation coefficient was used to assess the association between continuous variables. The association between ECG characteristics and AF was assessed using conditional logistic regression. All the variables associated with both AF and P-wave duration (P-value < .10) in the bivariate analyses were included in the multivariate model. We also explored the linear and nonlinear association between P-wave duration and AF using smoothing spline methods. A P-value lower than .05 was considered statistically significant.
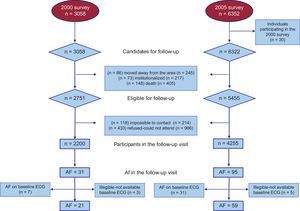
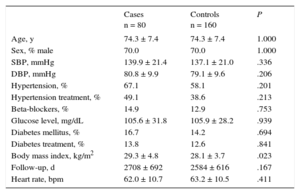
RESULTSThe median follow-up of the cohort was 7.12 years. The flowchart of participant inclusion is shown in Figure 2. Those attending the follow-up were younger, a high proportion were women, and had lower levels of systolic blood pressure, glycaemia, and triglycerides, as well as a lower proportion of treatment for hypertension, diabetes, and hypercholesterolemia at the baseline visit (). The analysis included 80 individuals with AF and 160 controls. Participant characteristics are shown in Table 1. The mean age was 74.3 years, and most of the participants were men. No differences in the prevalence of hypertension, hypertension treatment, diabetes, diabetes treatment, or in the mean values of systolic blood pressure, diastolic blood pressure, or heart rate were observed between cases and controls. However, the group of AF cases presented with higher body mass index than the group of controls.
Characteristics of the Study Population
| Cases n = 80 | Controls n = 160 | P | |
|---|---|---|---|
| Age, y | 74.3 ± 7.4 | 74.3 ± 7.4 | 1.000 |
| Sex, % male | 70.0 | 70.0 | 1.000 |
| SBP, mmHg | 139.9 ± 21.4 | 137.1 ± 21.0 | .336 |
| DBP, mmHg | 80.8 ± 9.9 | 79.1 ± 9.6 | .206 |
| Hypertension, % | 67.1 | 58.1 | .201 |
| Hypertension treatment, % | 49.1 | 38.6 | .213 |
| Beta-blockers, % | 14.9 | 12.9 | .753 |
| Glucose level, mg/dL | 105.6 ± 31.8 | 105.9 ± 28.2 | .939 |
| Diabetes mellitus, % | 16.7 | 14.2 | .694 |
| Diabetes treatment, % | 13.8 | 12.6 | .841 |
| Body mass index, kg/m2 | 29.3 ± 4.8 | 28.1 ± 3.7 | .023 |
| Follow-up, d | 2708 ± 692 | 2584 ± 616 | .167 |
| Heart rate, bpm | 62.0 ± 10.7 | 63.2 ± 10.5 | .411 |
DBP, diastolic blood pressure; SBP, systolic blood pressure.
Unless otherwise indicated, data are expressed as mean ± standard deviation.
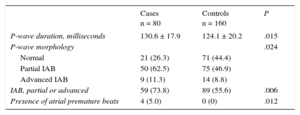
P-wave characteristics and differences between cases and controls are shown in Table 2. P-wave duration was longer in the group of AF cases than in the control group. The presence of IAB, partial or advanced, was also more frequent in AF cases than in controls. Atrial premature beats were only observed in cases, not in controls. P-wave duration was associated with heart rate (Pearson correlation coefficient = −0.167; P value = .010), body mass index (Pearson correlation coefficient = 0.121; P value = .062) (), and hypertension and hypertension treatment ().
P-wave Electrocardiographic Characteristics in Cases and Controls
| Cases n = 80 | Controls n = 160 | P | |
|---|---|---|---|
| P-wave duration, milliseconds | 130.6 ± 17.9 | 124.1 ± 20.2 | .015 |
| P-wave morphology | .024 | ||
| Normal | 21 (26.3) | 71 (44.4) | |
| Partial IAB | 50 (62.5) | 75 (46.9) | |
| Advanced IAB | 9 (11.3) | 14 (8.8) | |
| IAB, partial or advanced | 59 (73.8) | 89 (55.6) | .006 |
| Presence of atrial premature beats | 4 (5.0) | 0 (0) | .012 |
IAB, interatrial blocks.
Data are expressed as no. (%) or mean ± standard deviation.
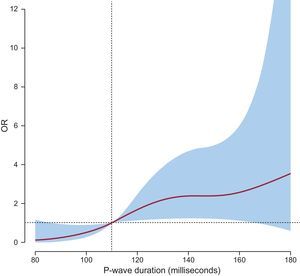
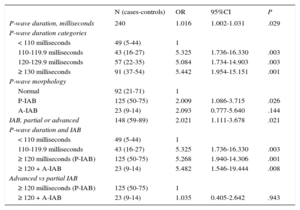
In the multivariate conditional logistic regression models including body mass index as a covariate (Table 3), we observed that P-wave duration (as a continuous or categorical variable) and the presence of partial or advanced IAB were directly associated with AF. Body mass index was also related to AF with odds ratios (OR) ranging between 1.065 and 1.071 in the logistic regression models. Additional adjustment for baseline heart rate and hypertension did not affect the magnitude of the observed associations (). When considering P-wave duration, we assessed the linearity of the association with AF and observed that the nonlinear component was statistically significant (P = .019) (Figure 3). We observed increased OR for AF when the duration exceeded 110 milliseconds; longer P-wave durations did not additionally increase the OR for AF.
Odds Ratio for Atrial Fibrillation of the Different Electrocardiographic Variables Analyzed in this Study (Adjusted for Body Mass Index; Survey-, Age-, and Sex-matched)
| N (cases-controls) | OR | 95%CI | P | |
|---|---|---|---|---|
| P-wave duration, milliseconds | 240 | 1.016 | 1.002-1.031 | .029 |
| P-wave duration categories | ||||
| < 110 milliseconds | 49 (5-44) | 1 | ||
| 110-119.9 milliseconds | 43 (16-27) | 5.325 | 1.736-16.330 | .003 |
| 120-129.9 milliseconds | 57 (22-35) | 5.084 | 1.734-14.903 | .003 |
| ≥ 130 milliseconds | 91 (37-54) | 5.442 | 1.954-15.151 | .001 |
| P-wave morphology | ||||
| Normal | 92 (21-71) | 1 | ||
| P-IAB | 125 (50-75) | 2.009 | 1.086-3.715 | .026 |
| A-IAB | 23 (9-14) | 2.093 | 0.777-5.640 | .144 |
| IAB, partial or advanced | 148 (59-89) | 2.021 | 1.111-3.678 | .021 |
| P-wave duration and IAB | ||||
| < 110 milliseconds | 49 (5-44) | 1 | ||
| 110-119.9 milliseconds | 43 (16-27) | 5.325 | 1.736-16.330 | .003 |
| ≥ 120 milliseconds (P-IAB) | 125 (50-75) | 5.268 | 1.940-14.306 | .001 |
| ≥ 120 + A-IAB | 23 (9-14) | 5.482 | 1.546-19.444 | .008 |
| Advanced vs partial IAB | ||||
| ≥ 120 milliseconds (P-IAB) | 125 (50-75) | 1 | ||
| ≥ 120 + A-IAB | 23 (9-14) | 1.035 | 0.405-2.642 | .943 |
95%CI, 95% confidence interval; A-IAB, advanced IAB; IAB, interatrial blocks; OR, odds ratio; P-IAB, partial IAB.
The association of abnormal P-wave morphology, defined by the presence of advanced IAB, with AF tended to be similar to that of partial IAB (Table 3). When considering P-wave duration and morphology simultaneously, we observed that the association with AF was present when P-wave duration was longer than 110 milliseconds, independently of the coexistence of advanced IAB. The OR for AF in the group with advanced IAB was very similar to that of the group with partial IAB (Table 3).
As a post hoc statistical power estimation and according to the sample size of our study and assuming an alpha risk of 0.05 and a beta risk of 0.20 in a 2-sided test, the ORs that could be detected as statistically significant was ≥ 4.5 on comparison of the group with advanced IAB vs the group with normal P-wave, and was ≥ 3.3 on comparison of the group with advanced IAB vs the group with partial IAB.
DISCUSSIONThe results of this study confirm the association between P-wave duration and AF. We observed that AF was associated with P-wave duration > 110 milliseconds, and that longer P-wave durations did not further increase the magnitude of the association. Partial and advanced IAB morphology were also associated with AF; however, the presence of advanced IAB did not increase the magnitude of the association with AF beyond that of partial IAB or P-wave duration between 110 and 119 milliseconds.
Several studies have identified variables associated with a higher risk of AF. Most of these studies have focused on clinical variables, such as age, hypertension, diabetes, cardiac morbidity, obesity, or obstructive sleep apnea.12,13,32 Few studies have also considered electrocardiographic characteristics, such as signs of left ventricular hypertrophy or P-R interval duration.33 In the last decade, P-wave characteristics have attracted the attention of several groups.34–36
The Framingham Heart Study (FHS),17,18 the Copenhagen ECG study19 and the Atherosclerosis Risk in Communities study (ARIC)18,20 have analyzed the association between several P-wave indices and the risk of AF. In all 3 studies, a statistically significant relationship between P-wave duration and the risk of AF was observed. The ARIC and the FHS studies compared the risk of AF in those individuals with a P-wave duration ≥ 120 milliseconds with those below this cutoff and reported a significant association (meta-analyzed hazard ratio [HR], 1.55; 95%CI, 1.29-1.85).18 In the Copenhagen ECG Study, P-wave duration was stratified in 5 groups, considering P-wave between 90 and 111 milliseconds as the reference group. The authors reported a HR for AF of 1.22 in the group with a P-wave of 112 to 119 milliseconds, a HR for AF of 1.50 in the group with a P-wave of 120 to 129 milliseconds and a HR for AF of 2.06 in the group with a P-wave ≥ 130 milliseconds (all of them statistically significant).19
Our data suggest that the magnitude of the association is higher and, in concordance with Nielsen et al.,19 appears at shorter P-wave duration, when the P-wave duration is greater than 110 milliseconds. The inclusion of individuals with P-wave duration between 110 and 119 milliseconds in the reference group could decrease the magnitude of the association reported in the FHS and the ARIC studies. There is an open discussion about the P-wave duration threshold to define interatrial block (100, 110 or 120 milliseconds). We believe that this definition should be based on the clinical implications of the P-wave duration rather than on its population distribution as has been proposed.37
The assessment of the pathological mechanisms explaining this association was beyond the scope of our study. However, previous reports have shown that P-wave duration is highly correlated with atrial fibrosis and fatty infiltration.38 Platonov et al.,39 reported that this fibrosis and fatty infiltration was more manifest in patients with permanent AF than in those with paroxysmal AF, in which the presence of abnormal electric activity within the pulmonary veins plays a major role. However, the presence of fibrosis in paroxysmal AF, at least in elderly patients, has also been documented.40,41 Interestingly, in our study we mainly identified permanent/persistent AF and missed most of the paroxysmal AF episodes. Therefore, the association between P-wave duration and AF in our study is based primarily on permanent/persistent AF and could be related to this fibro-fatty atrial infiltration.
Until recently, the diagnosis of IAB was not generally accepted, and both atrial enlargement and atrial blocks were considered nonspecific atrial abnormalities. Recent results from the ARIC study confirm that the presence of advanced IAB is associated with an increased AF risk (HR, 3.09; 95%CI, 2.51-3.79).20 In our study, the presence of A-IAB was also associated with AF, although this association was not statistically significant (OR, 2.09; 95%CI, 0.78-5.64). We also analyzed whether the combination of a long P-wave duration and the presence of advanced IAB increased the risk of AF compared with a P-wave duration ≥ 110 milliseconds. We did not observe an increased risk when both factors were present; therefore, the risk would be directly related to P-wave duration. However our study is hampered by low statistical power and these results should be interpreted with caution. De Bacquer et al.,15 have reported that the combination of long P-wave and morphological P-wave alterations (notching or deflection) significantly increased the risk of AF. Additional studies should analyze the combined effect of long P-wave and A-IAB on AF risk.
Recent studies have shown that the inclusion of some electrocardiographic markers (P-wave duration, or PR interval or left ventricular hypertrophy) did not improve predictive capacity, as measured by discrimination or reclassification, of the CHARGE-AF risk function.18,42 Further studies are warranted to assess whether the inclusion of P-wave duration or the presence of advanced IAB could improve the predictive capacity of this type of risk functions.
Limitations and StrengthsSeveral limitations should be considered: a) the sample size of the study is limited by the number of events. Moreover, the number of participants with advanced IAB is reduced and limits the assessment of this P-wave morphology pattern; b) follow-up was based on a single visit and use of a standard 12-lead ECG, which limits the ability to detect paroxysmal AF; c) the retrospective design of the study could limit the assessment of the exposure of interest, and also that of potential confounders, and d) those participants who did not attend the follow-up were older, had higher comorbidity, and likely had a higher risk of AF than those who completed the follow-up. Moreover, as the same variables that were associated with AF have been reported to be associated with IAB,20 we likely missed some individuals with AF in the follow-up and some with IAB in the baseline visit. These results likely reduced the statistical power of our study and highlight a potential bias that would underestimate the magnitude of the reported association.
Among the strengths of the study is the representative population, which supports the external validity of the results. Moreover, all the ECG measurements were performed manually by 2 independent observers and showed a high accuracy.
CONCLUSIONSP-wave duration is associated with a higher risk of developing AF, beginning at 110 milliseconds. Advanced IAB morphology did not seem to provide an additional AF risk beyond that of P-wave duration, although the reduced number of participants with advanced IAB limits the conclusion about this P-wave morphology pattern. Further studies are required to validate this P-wave duration threshold and to analyze the added predictive value of this electrocardiographic marker.
FUNDINGThis work was supported by the Spanish Ministry of Economy and Innovation through the Carlos III Health Institute [Red de Investigación Cardiovascular RD12/0042, FIS99/0655, FIS99/0013-01, FIS 99/9342, PI081327, MS12/03287], European Funds for Development, and by the Catalan Research and Technology Innovation Interdepartmental Commission [SGR 2014-1195]. I.R. Dégano was funded by the RECERCAIXA Program, Obra Social “La Caixa” [RE087465].
CONFLICTS OF INTERESTNone declared.
- –
Atrial fibrillation is the most common clinically significant cardiac arrhythmia.
- –
Some clinical and electrocardiographic characteristics are associated with a higher risk of AF.
- –
Long P-wave duration and interatrial block have been associated with AF risk.
- –
However, the combined significance of P-wave duration and morphology and risk of AF has not been evaluated.
- –
We confirm that P-wave duration is directly associated with a higher risk of AF.
- –
We have identified that a P-wave longer than 110 milliseconds already increases the risk of AF.
- –
Advanced interatrial block does not seem to produce an additional AF risk beyond that of P-wave duration.
.
To the REGICOR investigators and participants (can be consulted in the