Regular leisure-time physical activity (LTPA) has been consistently recognized as a protective factor for cardiovascular diseases (CVD) and all-cause mortality. However, the pattern of this relationship is still not clear. The aim of this study was to assess the relationship of LTPA with incident CVD and mortality in a Spanish population.
MethodsA prospective population-based cohort of 11 158 randomly selected inhabitants from the general population. LTPA was assessed by a validated questionnaire. Mortality and CVD outcomes were registered during the follow-up (median: 7.24 years). The association between LTPA and outcomes of interest (all-cause mortality and cardiovascular disease) was explored using a generalized additive model with penalized smoothing splines and multivariate Cox proportional hazard models.
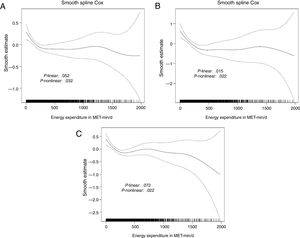
ResultsWe observed a significant nonlinear association between LTPA and all-cause and CVD mortality, and fatal and nonfatal CVD. Moderate-vigorous intensity LTPA, but not light-intensity LTPA, were associated with beneficial effects. The smoothing splines identified a cutoff at 400 MET-min/d. Below this threshold, each increase of 100 MET-min/d in moderate-vigorous LTPA contributed with a 16% risk reduction in all-cause mortality (HR, 0.84; 95%CI, 0.77-0.91), a 27% risk reduction in CVD mortality (HR, 0.73; 95%CI, 0.61-0.87), and a 12% risk reduction in incident CVD (HR, 0.88; 95%CI, 0.79-0.99). No further benefits were observed beyond 400 MET-min/d.
ConclusionsOur results support a nonlinear inverse relationship between moderate-vigorous LTPA and CVD and mortality. Benefits of PA are already observed with low levels of activity, with a maximum benefit around 3 to 5 times the current recommendations.
Keywords
Since the seminal studies by Morris et al.1 and Paffenbarger et al.,2 physical activity (PA) has been consistently reported as a protective factor for cardiovascular disease (CVD) and all-cause mortality.3–8 Moreover, PA has been associated with a lower risk of fatal and nonfatal CVD.3,9 It has been estimated that physical inactivity causes 6% of the burden of coronary heart disease, 7% of the burden of diabetes, and 9% of the burden of premature mortality.10 Therefore, the World Health Organization recommends that adults achieve at least 150minutes of moderate-intensity aerobic PA or 75minutes of vigorous-intensity aerobic PA throughout the week, or an equivalent combination of moderate- and vigorous-intensity PA, which approximately corresponds to 600 MET-min/wk or 85 MET-min/d.11 Unfortunately, these recommended levels are not achieved by 24.5% (11.6%-46.5%) of adults in Europe12 and 35% of adults in Spain.13
In the study of the relationship between PA and health, several domains (occupation, household, active commuting, and leisure) and dimensions (type, frequency, duration, and intensity) have been defined.14 The frequency, duration, and intensity of PA practice within each domain are used to estimate the amount of PA. Leisure-time PA (LTPA) is the domain showing the strongest beneficial effects on health.15 Moreover, the intensity and amount of PA could be relevant to defining its health effects. A recent meta-analysis suggested that the relationship between LTPA and mortality is linear,6 but others have reported that the effect of LTPA on mortality or other outcomes follows a nonlinear J-shaped inverse relationship.3,7–9 The pattern of the dose-response relationship and the role of PA intensity are relevant aspects to consider, especially to define adequate recommendations for the general population.
Three prospective cohort studies have analyzed the relationship between LTPA and cardiovascular or mortality outcomes in Spain16–19 but the dose-response relationship, taking into consideration the intensity of PA, has been specifically analyzed only in the PREDIMED cohort, which includes older adults with high vascular risk.19 The aim of this study was to determine the linear and nonlinear dose-response association of LTPA, considering PA intensity, with CVD and all-cause mortality risk in a population-based cohort.
METHODSStudy design and populationThe REGICOR study is a prospective population-based cohort in Girona (≈700 000 inhabitants) that aims to study the burden of CVD and its determinants at the population level. The characteristics of the study have been detailed elsewhere.20 In summary, individuals were randomly selected from the population census and inclusion criteria required that participants had lived in the referral area for at least 6 months, were free of end-stage disease, and were not institutionalized. Selected participants were contacted by a letter informing them of the aims of the study and the tests to be performed. The recruitment took place in 3 consecutive periods: 1748 participants aged 25 to 74 years in 1995, 3056 aged 25 to 74 years in 2000, and 6352 aged 35 to 79 years in 2005. The participation rate was higher than 70% and all the participants were followed up until December 2011. In the case of participants randomly selected for more than 1 survey, the longest available follow-up data were considered. The study protocol was approved by the local ethics committee and each participant signed an informed consent form at enrolment.
Baseline dataExaminations were performed by trained nurses and interviewers using standardized and validated questionnaires and measurement methods, as previously described.21 Smoking, alcohol intake, and educational level were self-reported on standard questionnaires. Hypertension was considered when previously diagnosed by a physician, under treatment, or with values of systolic blood pressure ≥ 140mmHg or diastolic blood pressure ≥ 90mmHg. Participants were asked to fast for at least 10hours before their appointment at the health examination site. Fasting blood samples were taken and total cholesterol, high-density lipoprotein cholesterol, triglycerides, and glucose concentrations were determined. Low-density lipoprotein cholesterol levels were estimated using the Friedewald equation when triglycerides were <300mg/dL. Diabetes was defined if previously diagnosed, under treatment, or with fasting glucose values ≥ 126mg/dL. The presence of previous CVD was self-reported by the participants.
Assessment of leisure-time physical activityParticipants were asked about PA practice using the Minnesota Leisure-time Physical Activity Questionnaire,22 validated for the Spanish adult population.23,24 This questionnaire assesses leisure and active commuting domains and frequency, duration, and intensity dimensions. Briefly, from a list of 64 activities, participants mark those they have practiced during the year prior to the visit and a trained interviewer collects information related to the frequency of practice and the duration of each session. Each LTPA is assigned an intensity based on metabolic equivalents of task (MET).22,25
Total LTPA (T-LTPA) was estimated, and further classified as light-intensity LTPA if it required <4 METs (such as low-paced walking), moderate-intensity if it required 4 to 5.5 METs (such as brisk walking), and vigorous-intensity LTPA if it required ≥ 6 METs (such as jogging). We also estimated the combination of moderate-intensity LTPA and vigorous-intensity LTPA. We excluded any participant with T-LTPA=0 MET-min/wk.
Follow-upThe follow-up included physical re-examinations and telephone contact every 2 years. To ascertain any cardiovascular event or death, we also reviewed medical records, linked the data with a population-based myocardial infarction registry, and cross-checked these sources. To identify fatal events not otherwise recorded, we linked our data with the official mortality register.
All the events were classified by an event committee according to standardized criteria. Three main outcomes were defined: a) all-cause mortality; b) CVD mortality (ICD9 codes 390-459 and 798 or ICD10 codes I00-I99, in the mortality registry); and c) CVD mortality and nonfatal coronary or cerebrovascular events (ICD9 codes 410-414 and 431-437 or ICD10 codes I20-I25, I69.1-I69.9, in the medical records). If there were multiple CVD events in the same participant, the first-occurring event was considered.
Statistical analysisCategorical data are expressed as frequencies and percentages. Continuous variables are expressed as mean (standard deviation), or median [interquartile range] if they did not follow a normal distribution.
The adjusted risk of CVD or mortality over time based on the amount of LTPA was modelled using a generalized additive model with penalized spline smoothing (spline function, R Survival Package).26 This function allows a maximum of 10 knot points to assess the linear and nonlinear componenents of the dose-response relationship. Those participants with a LTPA> 2000 MET-min/d were excluded from these analyses due to their low number. When the nonlinear component was nonsignificant, LTPA was considered as a continuous variable in Cox proportional hazard regression models. Otherwise, we used bootstrapping methods to define the best cutpoint(s) at which a change in the linear dose-response association was observed. We performed 1000 iterations per outcome of interest and calculated the median of the observed cutpoint, which was then defined as the best cutpoint. The analyses were stratified according to best cutpoint, and Cox regression modelling considered LTPA as a continuous variable in each of the defined strata.
For each outcome, 2 models were created, one including age, sex, and survey, and the second one additionaly including smoking status, high-density lipoprotein, low-density lipoprotein, systolic blood pressure, glucose concentration, and treatments for hypertension, hypercholesterolemia, and diabetes. We also explored the interactions of LTPA with age and sex on the outcomes of interest. PA was included as total LTPA, and based on its intensity, moderate-vigorous and light LTPA. For 2 of the outcomes (CVD mortality and CVD mortality and nonfatal coronary or cerebrovascular disease) other causes of mortality different than CVD were considered as competing events in the analyses (competing risk).
All statistical tests were based on 2-tailed hypothesis testing and P values <.05 were considered statistically significant. Statistical analyses were performed with R version 3.4.2.27
Post-hoc statistical power estimationAn estimate of the statistical power of the study indicated that it was powered to detect as statistically significant a hazard ratio (HR) <0.80 and 0.74 for all-cause mortality and CVD events, respectively. The accepted alpha risk in a 2-sided test was 0.05, and the accepted beta risk was 0.20.
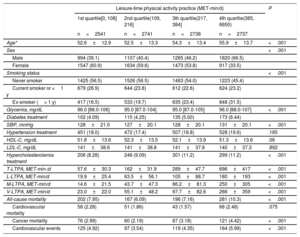
RESULTSAmong 11 158 participants who agreed to participate, 72 were excluded due to duplication of data among the 3 cohorts and 210 due to values of T-LTPA=0. The final study population totalled 10 876 participants. Baseline characteristics of the participants stratified by quartiles of T-LTPA are presented in table 1. The participants with higher amounts of T-LTPA were older, with a higher proportion of men, former smokers, and treatment for diabetes and hypercholesterolemia, compared with those with lower T-LTPA levels. The most common types of PA practiced in our population were: walking (light-intensity LTPA), brisk walking (moderate-intensity LTPA), gardening (moderate-intensity LTPA), walking trails (vigorous-intensity LTPA), climbing stairs (vigorous-intensity LTPA), and sports activities (vigorous-intensity LTPA).
Baseline characteristics of the participants and number of events of interest during the follow-up stratified by quartiles of LTPA in MET-min/d
| Leisure-time physical activity practice (MET-min/d) | P | ||||
|---|---|---|---|---|---|
| 1st quartile[0, 108] | 2nd quartile(109, 216] | 3th quartile(217, 384] | 4th quartile(385, 6650) | ||
| n=2541 | n=2741 | n=2738 | n=2737 | ||
| Age* | 52.6±12.9 | 52.5±13.3 | 54.3±13.4 | 55.9±13.7 | <.001 |
| Sex | <.001 | ||||
| Male | 994 (39.1) | 1107 (40.4) | 1265 (46.2) | 1820 (66.5) | |
| Female | 1547 (60.9) | 1634 (59.6) | 1473 (53.8) | 917 (33.5) | |
| Smoking status | <.001 | ||||
| Never smoker | 1425 (56.5) | 1526 (56.5) | 1463 (54.0) | 1223 (45.4) | |
| Current smoker or <1 y | 679 (26.9) | 644 (23.8) | 612 (22.6) | 624 (23.2) | |
| Ex-smoker (> 1 y) | 417 (16.5) | 533 (19.7) | 635 (23.4) | 848 (31.5) | |
| Glycemia, mg/dL | 96.0 [88.0-106] | 95.0 [87.0-104] | 95.0 [87.0-105] | 96.0 [88.0-107] | <.001 |
| Diabetes treatment | 102 (4.09) | 115 (4.25) | 135 (5.00) | 173 (6.44) | |
| SBP, mmHg | 128±21.0 | 127±20.1 | 128±20.1 | 131±20.1 | <.001 |
| Hypertension treatment | 451 (18.0) | 472 (17.4) | 507 (18.8) | 528 (19.6) | .185 |
| HDL-C, mg/dL | 51.8±13.6 | 52.3±13.5 | 52.1±13.9 | 51.3±13.6 | .06 |
| LDL-C, mg/dL | 141±38.6 | 141±38.8 | 141±37.8 | 140±37.3 | .892 |
| Hypercholesterolemia treatment | 206 (8.28) | 246 (9.09) | 301 (11.2) | 299 (11.2) | <.001 |
| T-LTPA, MET-min·/d | 57.6±30.3 | 162±31.9 | 289±47.7 | 696±417 | <.001 |
| L-LTPA, MET-min/d | 19.9±25.4 | 63.5±56.1 | 105±88.7 | 180±193 | <.001 |
| M-LTPA, MET-min/d | 14.6±21.5 | 43.7±47.3 | 86.2±81.3 | 250±305 | <.001 |
| V-LTPA, MET-min/d | 23.0±22.0 | 55.1±48.2 | 97.7±82.6 | 266±359 | <.001 |
| All-cause mortality | 202 (7.95) | 167 (6.09) | 196 (7.16) | 281 (10.3) | <.001 |
| Cardiovascular mortality | 58 (2.28) | 51 (1.86) | 43 (1.57) | 68 (2.48) | .075 |
| Cancer mortality | 76 (2.99) | 60 (2.19) | 87 (3.18) | 121 (4.42) | <.001 |
| Cardiovascular events | 125 (4.92) | 97 (3.54) | 119 (4.35) | 164 (5.99) | <.001 |
HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; LTPA, leisure-time physical activity; L-LTPA, energy expenditure in light-intensity LTPA; MET, metabolic equivalent; M-LTPA, energy expenditure in moderate-intensity LTPA; SBP, systolic blood pressure; T-LTPA, Total energy expenditure in LTPA; V-LTPA, energy expenditure in vigorous-intensity LTPA.
Data are expressed as No. (%) or mean±standard deviation or median [interquartile range].
After a median of 7.24 [interquartile range 5.89-9.37] years of follow-up, 863 deaths were reported. The generalized additive model showed a significant nonlinear association between T-LTPA and all-cause mortality (figure 1). In the bootstrapping analysis, the best cutpoint to define a change in the linear dose-response association was around 350 to 400 MET-min/d, and we selected the latter as the best cutpoint. Below this threshold and adjusted by confounders, increasing levels of T-LTPA from 0 to 400 MET-min/d had a protective effect on all-cause mortality, with a HR of 0.89 for any increase of 100 MET-min/d and 95% confidence interval (95%CI) of 0.83 to 0.96 (table 2). Higher amounts of T-LTPA (> 400 MET-min/d) did not provide additional benefit (figure 1).
Predicted relative risk (with 95% confidence limits) of all-cause mortality (A), cardiovascular mortality (B), and total cardiovascular events (C) related to increasing levels of total leisure-time physical activity (MET-min/d). The graph was produced using a generalized additive model with spline smoothing functions and 4 degrees of freedom. MET, metabolic equivalent.
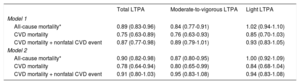
Hazard ratio (95% confidence interval) of the association between LTPA practice from 0 to 400 MET-min/d and all-cause mortality, CVD mortality, and cardiovascular disease morbidity or mortality. The effect size of the association is expressed for each increase of 100 MET-min/d in LTPA
| Total LTPA | Moderate-to-vigorous LTPA | Light LTPA | |
|---|---|---|---|
| Model 1 | |||
| All-cause mortality* | 0.89 (0.83-0.96) | 0.84 (0.77-0.91) | 1.02 (0.94-1.10) |
| CVD mortality | 0.75 (0.63-0.89) | 0.76 (0.63-0.93) | 0.85 (0.70-1.03) |
| CVD mortality + nonfatal CVD event | 0.87 (0.77-0.98) | 0.89 (0.79-1.01) | 0.93 (0.83-1.05) |
| Model 2 | |||
| All-cause mortality* | 0.90 (0.82-0.98) | 0.87 (0.80-0.95) | 1.00 (0.92-1.09) |
| CVD mortality | 0.78 (0.64-0.94) | 0.80 (0.65-0.99) | 0.84 (0.68-1.04) |
| CVD mortality + nonfatal CVD event | 0.91 (0.80-1.03) | 0.95 (0.83-1.08) | 0.94 (0.83-1.08) |
CVD, cardiovascular disease; LTPA, leisure-time physical activity; MET, metabolic equivalent.
Model 1: Adjusted for age, sex and survey
Model 2: Adjusted for age, sex, survey, smoking, high-density cholesterol cholesterol, low-density cholesterol, cholesterol treatment, systolic blood pressure, antihypertensive treatment, glucose, diabetes treatment, body mass index and family history of CVD.
When our analysis incorporated PA intensity, moderate and vigorous-intensity LTPA showed a protective association with mortality (table 2). Below the 400 MET-min/d threshold, each 100 MET-min/d increase in moderate and vigorous-intensity LTPA was associated with a 16% decrease in all-cause mortality risk (HR, 0.84; 95%CI, 0.77-0.91). The fully-adjusted model showed similar results.
We observed no significant interaction between LTPA and age or sex on mortality.
Physical activity and cardiovascular eventsTo evaluate the relationship between LTPA and cardiovascular events, a further 453 individuals with CVD at baseline were excluded from the population, resulting in a final sample of 10 423 individuals. During follow-up, 437 cases of CVD were identified including 226 fatal CVD events.
The general additive model showed a significant nonlinear association between T-LTPA and incident CVD (figure 1). Again, the bootstrapping analysis found that the best cutpoint to define a change in the linear dose-response association was around 350-400 MET-min/d, and we selected 400 MET-minute/d as the cutpoint. Below this threshold and adjusted by confounders, increasing levels of T-LTPA from 0 to 400 MET-min/d had a protective effect on CVD mortality, with a HR of 0.75 for any increase in 100 MET-min/d and 95%CI of 0.63 to 0.89 (table 2). The association with fatal and nonfatal CVD events was weaker (HR, 0.87; 95%CI, 0.77-0.98). The fully-adjusted model showed similar results.
When the intensity of LTPA was considered (table 2), we found a statistically significant association between moderate-intensity and vigorous-intensity LTPA and CVD mortality (HR, 0.76; 95%CI, 0.63-0.93) and marginally nonsignificant with incident CVD events (HR, 0.89; 95%CI, 0.79-1.01). The fully-adjusted model showed similar results.
We observed no significant interaction between LTPA and age or sex on CVD risk.
DISCUSSIONIn this study, we observed a nonlinear relationship between LTPA and cardiovascular events and mortality risk. An inverse linear association was observed between LTPA and these 2 clinical outcomes up to a threshold of 400 MET-min/d, with no further benefit above this amount. Moreover, only moderate and vigorous intensity, but not light-intensity, LTPA was associated with a beneficial effect.
These results concur with current guidelines for adults that recommend at least 150minutes of moderate-intensity or 75minutes of vigorous-intensity aerobic PA throughout the week, or an equivalent combination of the 2 intensities.11 This amount of PA represents an approximate energy expenditure of 600 MET-min/wk or 85 MET-min/d. Guidelines also state that additional health benefits can be obtained if this practice is increased to 300min/wk of moderate-intensity or 150min/wk of vigorous-intensity PA.
The relationship of PA to CVD, events, and mortality has been widely studied in the past. However, the dose-response pattern of this association remains controversial. Cheng et al.6 recently published a systematic review and meta-analysis suggesting that this relationship is linear, yet this affirmation relies on results showing moderate to high heterogeneity between studies. However, other pooled- and meta-analyses have reported a nonlinear association. Arem et al.8 performed a pooled analysis of 6 cohorts including more than 650 000 individuals and reported that meeting the PA recommendations is associated with a significant longevity benefit. They reported an upper threshold for mortality benefit at 3 to 5 times the current PA recommendations, which would be roughly equivalent to 250 to 400 MET-min/d. In a meta-analysis of 33 studies (9 allowing quantitative estimates of PA), Sattelmair et al.9 concluded that individuals engaging in PA equivalent to the recommendations had a 14% lower risk of coronary heart disease, while those engaging in 2 times the recommendations had a 20% lower risk, with modest decreases in risk at higher levels of PA practice. A recent meta-analyses including studies with objective measurement of PA also reports a nonlinear dose-response relationship between PA and all-cause mortality with a maximum benefit around 15 to 20min/d of MVPA.3 When considering the 3 Spanish cohorts in the EPIC-Spain study, Huerta et al.16 included over 38 000 individuals with more than 13 years of follow-up. They found no association between recreational PA and cardiovascular or overall mortality, although a significant inverse association was observed in women when recreational and household activities were considered. In the SUN cohort, Alvarez-Alvarez et al.17 included more than 1000 university alumni with a median follow-up of 10 years. They reported a lower CVD risk among those with LTPA> 750 MET-min/wk (∼100 MET-min/d) and those with a LTPA> 1500 MET-min/wk (HR, 0.77 and 0.75, respectively), although these associations were not statistically significant, probably due to the low number of events.17 The PREDIMED cohort included 7356 older adults with high vascular risk and more than 6 years of follow-up. The authors reported that higher LTPA levels, regardless of intensity (total, light, and moderate-to-vigorous) were associated with lower all-cause mortality, and that this association was nonlinear with a maximum effect around 300 MET-min/d.19
In our study, we observed a nonlinear association with a maximum benefit at around 350 to 400 MET-min/d, with no additional benefit above this point. The inconsistencies between studies in terms of the linear vs nonlinear pattern of the association, and of the different upper threshold definitions, could be explained by several reasons: differences in the length of follow-up (the longer the follow-up the greater the benefit), mean age of participants (greater benefits in younger participants), and mainly the accuracy of the method used to assess PA. The nonlinear association is consistent with the results reported by Elelund et al.,3 Arem et al.,8 and Sattelmair et al.9 We obtained a threshold similar to that reported by Arem et al.8 but higher than that of Sattelmair et al.9 (approximately 200 MET-min/d); however, their analysis only considered coronary heart disease. Moreover, most of these studies used questionnaires to measure PA, and differences in the instruments used could introduce significant heterogeneity between their results.14 Ekelund et al.3 showed that when using objective methods to assess PA the effect size of the association between PA and mortality are about twice as large compared with those reported in studies using self-reported PA.
Regarding PA intensity, our results provide evidence that longevity and cardiovascular benefits are related to moderate- and vigorous-intensity LTPA. This is concordant with current guidelines11 and previous studies.7,8,28 Some studies report that light-intensity PA might also be beneficial.3,4,19,29,30 Saint-Maurice et al.30 suggested that, despite an association between light-intensity PA and reduced mortality, an approximately equal volume of moderate-to-vigorous PA had greater benefits. On the other hand, most of these studies were performed in older individuals. In our previous study in a Spanish population, we reported that light-intensity PA was associated with lower risk of myocardial infarction in persons aged 65 to 74 years but not in the younger population.31 However, we did not observe this association in the present analysis, likely because the outcomes of interest were different. A meta-analysis published in 2019 concludes that, although light-intensity PA could play an important role in improving adult cardiometabolic health and reducing mortality risk, definitive conclusions cannot yet be established.3
Strenghts and limitationsThe main strengths of our study are the prospective population-based cohort design. Moreover, we used general additive models to properly assess the linear and nonlinear dose-response relationships between LTPA and the health outcomes of interest.
Our study also has several limitations. First, LTPA was measured by a self-reported questionnaire. Although questionnaires are a common tool for epidemiological surveys and the instrument used in this study had been previously validated for this population, we cannot exclude a certain measurement bias. Also, a recall bias might have influenced the quality of information about LTPA practice. Second, we only considered LTPA and did not include other domains, such as occupational and household PA. Third, we did not include an analysis of sedentary behavior, which has also arisen as an independent cardiovascular risk factor.32 Finally, we did not consider changes in PA practice, or in other covariates, during the follow-up of the study.
CONCLUSIONSThis study lends support to the public health relevance of PA contributing to the prevention of CVD and all-cause mortality, even in a European country with a low incidence of diseases of the circulatory system. Furthermore, our results support a nonlinear relationship between moderate-vigorous PA and CVD and all-cause mortality: a large part of the benefits of PA can be obtained with low-moderate levels of practice, with a maximum benefit around 3 to 5 times the current recommendations. This is an important message to encourage the general population to engage in PA practice, supporting the “some is better than none, more is slightly better” approach.
FUNDINGThis project was funded by the Carlos III Health Institute–European Regional Development Fund (FIS PI12/00232; FIS PI15/00051, CIBERCV, CIBERESP), and the Government of Catalonia through the Agency for Management of University and Research Grants (PERIS SLT002/16/00088, 2017SGR222). A. Fernández-Sanlés was funded by the Spanish Ministry of Economy and Competitiveness (BES-2014–069718).
CONFLICTS OF INTERESTNo conflict of interest to declare.
- -
CVD is the main cause of mortality in developed countries.
- -
Regular LTPA has been widely recognized as a protective factor for incident CVD and all-cause mortality.
- -
There are contradictory results regarding the dose-response pattern of the effect of LTPA on incident CVD and all-cause mortality.
- -
This study supports the hypothesis of a nonlinear relationship of LTPA to incident CVD and all-cause mortality.
- -
There is an upper threshold for the beneficial effect of LTPA at 400 MET-min/d, above which no further benefit is observed.
- -
The beneficial effect of LTPA appears to be mainly related to moderate- and vigorous-intensity PA.