Myocardial infarction (MI) incidence and case fatality trends are highly informative but relatively untested at the population level. The objective of this work was to estimate MI incidence and case fatality in the Girona population aged 35-74 years, and to determine their 30-year trends (1990-2019).
MethodsThe REGICOR (Girona Heart Registry) monitored MI incidence and case fatality rates from 1990 to 2008. For the period 2008 to 2019, we linked discharges from Girona hospitals (n=4 974 977) and mortality registry (n=70 405) during this period. Our linkage algorithm selected key MI diagnostic codes and removed duplicates. Estimates from the linkage algorithm and the REGICOR registry were compared using chi-square tests for overlapping years (2008-2009). We estimated the annual percent change (APC) of standardized MI incidence and 28-day case fatality, and analyzed their trends using joinpoint regression.
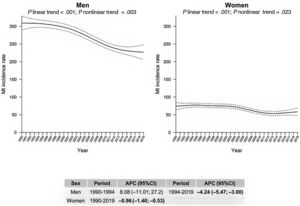
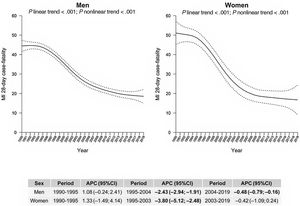
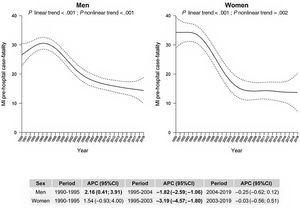
ResultsMI incidence and case fatality estimates were similar in the linkage algorithm and the REGICOR registry. We observed significant decreasing trends in the incidence of MI. The trend was APC, -0.96% (95% confidence interval (95%CI), –1.4 to –0.53) in women from 1990 to 2019 and –4.2% (95%CI, –5.5 to –3.0) in men from 1994 to 2019. The largest decrease in case fatality was –3.8% (95%CI, -5.1 to –2.5) from 1995 to 2003 in women and –2.4% (95%CI, –2.9 to –1.9) from 1995 to 2004 in men, mainly due to prehospital case fatality declines: -1.8% (95%CI, –2.6 to –1.1) in men and –3.2% (95%CI, –4.6 to –1.8) in women.
ConclusionsIn Girona, MI incidence and case fatality decreased between 1990 and 2019. The incidence showed a slow but continuous decrease while case fatality only stabilized in the last decade, particularly in women.
Keywords
Despite improvements in prevention, treatment, and patient management, myocardial infarction (MI) remains the leading single cause of mortality in Europe, accounting for more than 1.8 million deaths each year.1 The standardized mortality rate per 100 000 inhabitants is the most widely available indicator used for MI burden trend analysis, as these data can be easily obtained from local mortality registries and indicate the number of persons dying of MI annually per 100 000 inhabitants in a region.
MI mortality rates are influenced, in part, by MI incidence and changes in risk factors. However the main determinants are disease severity and acute-phase patient management.2 In contrast, trends in incidence rates are mainly influenced by population risk factors and the prevalence of lifestyles,3 and indicate the total number of persons developing MI per 100 000 inhabitants regardless of their survival. The combination of mortality and incidence data yields case fatality data, computed as the proportion of fatal cases among the total number of cases occurring within a particular timeframe (eg, 28 days).
In Europe, attempts to update MI incidence and case fatality data are precluded by the lack of a consistent method to define and count fatal and nonfatal cases at the population level,4 and by limited access to data sources whose content is restricted by European Personal Data Protection regulations.4–8. Most data come from population-based registries (eg, the WHO-MONICA Project)6, in which fatal and nonfatal events are carefully reviewed.4,9 Unfortunately, the maintenance of population registries is time-consuming, expensive, requires trained personnel,10 and is usually restricted to small geographical areas and relatively short time spans.11 For instance, REGICOR (Registre GIroní del COR or Girona Heart Registry) collected this information in the region of Girona between 1990 and 2008, but data collection was discontinued afterward.
An alternative to gather MI incidence and case fatality indicators in large populations is linking routinely collected health care data (eg, primary care records, hospital discharges, mortality registers, pharmacy information)12,13 to allow for more cost-effective long-term analyses of MI incidence and case fatality indicators in large populations. Linked-data methods (LDM) are cost-effective and have been used to estimate selected MI burden indicators in Denmark,14 Finland,15 the Netherlands,16 Norway,17 Sweden,18 and the UK.19 To ensure optimal quality, the method used to estimate MI incidence and case fatality must be validated with population-based registries whenever possible, which has been done in studies in Finland and the UK.13,20,21
A minimum data set (MDS) of all public hospital discharges reached full implementation in Catalonia in 2008. The Data Analysis Program for Health Research and Innovation (PADRIS, for Programa d’Analítica de Dades per a la Recerca i la Innovació en Salut) made the MDS available for research in 2018, together with mortality registry records from 2008 onwards. Data for 2008 to 2009 overlap the REGICOR population registry of all incident MI patients in Girona from 1990 to 2009,4,6,7 which allowed us to validate the procedure.
Our objective was to determine the 30-year trends of MI incidence rate and 28-day case fatality in Girona between 1990 and 2019 in north-eastern Spain.
METHODSStudy designWe used a population-based retrospective cohort study. The reference population varied around 700 000 inhabitants from 1990 to 2019. We used the official population figures provided by the Institut d’Estadística de Catalunya as the denominator for MI incidence.
Population participants 1990 to 2008We included the REGICOR prospective MI registry participants. REGICOR collected all cases (fatal and nonfatal) of MI in the study region between 1990 and 2008, and validated the diagnoses by standardized methods.4,6 The number of hospitalized MI patients was 6775 (5531 men and 1244 women), and 2401 (1706 men and 695 women) patients with an MI diagnosis in their death certificates died before reaching a hospital.
Population-based data sources and linkage methods 2008 to 2019We electronically linked (LDM) 2 routinely updated digital databases: the Catalan mortality registry and the hospitalization discharge MDS for all hospitals in the province of Girona.
First and recurrent MI cases were classified by both the WHO-MONICA22 and American Heart Association/European Society of Cardiology criteria.23 MI total events included 3 WHO-MONICA categories: nonfatal and fatal definite MI (NF1+F1), fatal possible MI or coronary death (F2), and unclassifiable deaths (insufficient data) (F9).22 We selected patients from the hospital discharge MDS with a main diagnosis of MI (code 410, ICD-9, or I21X, ICD-10). In nonfatal cases, code 410 in second place was included when the main diagnosis was MI-related (411 to 414 or 427.4, 427.5, 427.8, 427.9, 428, 429.0 or 997.1) or the patient died during admission. In-hospital fatal cases with 410.X, ICD-9, or I21X, ICD-10 diagnosis in any position were also included. Finally, patients with codes ICD-9 410-414 or ICD-10 I20-I24, I46 and I49 as the main cause of death in the Catalan mortality registry were selected. All cases were anonymized and assigned a unique code. Both datasets were combined and checked for duplicate case-codes (transfers to a second hospital and in-hospital case-fatalities also listed in the mortality registry). Fatal cases registered in MDS hospital records and in the mortality registry were counted only once, in the MDS. The quality of both administrative registries has been previously validated.24,25
Myocardial infarction indicatorsCumulative incidence and 28-day case fatality (in-hospital, prehospital, and 28-day total) were calculated by year and sex for the population aged 35 to 74 years. Incidence rates were age-standardized (weights were 14, 14, 11, and 7 for age groups 35-44, 45-54, 55-64, and 65-74 years, respectively) using the 1976 European Standard Population, which was chosen over the 2013 European Standard Population to allow direct comparison with previous publications. Case fatality was standardized using weights derived from the distribution of MI events by age group (4, 13, 30 and 53 for the same age groups, respectively).26
Age-group specific cumulative MI incidence per 100 000 inhabitants was calculated as the annual total number of MI cases divided by the census population by year and sex. We also calculated the 28-day case fatality ratio as the percentage of the population who had an MI and who died (prehospital, in-hospital, and total) within 28 days of symptom onset.
REGICOR population-based database validationTo validate the results obtained from the LDM, we compared the MI incidence rates and 28-day case fatality in Girona with those of the REGICOR population-based MI registry,4,6 which operated in the same area in the overlapping 2008 to 2009 period for the population aged 35 to 74 years. Case-finding procedures in the REGICOR registry have been previously described.6 Briefly, MI cases were identified by registering all MI patients admitted to the regional coronary unit, by screening discharge records of patients admitted to all hospitals and clinics of the area, by screening medical transportation records, and by reviewing medical records corresponding to death certificates with ICD-9 codes 410-414.
Statistical analysisDifferences between REGICOR- and LDM-estimated incidence rates and case fatality were tested using the chi-square statistic and also comparing the point estimates and their 95% confidence intervals (95%CI). For incidence estimates between 1990 and 2000, we applied sex-specific correction coefficients (1124 for men and 1201 for women) to correct for the increase in the diagnostic sensitivity of troponin.4,27 Correction was not applied to case fatality, as the effect of the AHA/ESC definition in these MI indicators is negligible.
Joinpoint regression analysis was used to detect significant changes in trends limited to a maximum of 2 joinpoints; the Bayesian information criterion was applied to select the model that best fitted the data with the smallest number of joinpoints. Changes in annual percent change (APC) with 95%CI changes were calculated in each period defined by significant joinpoints. Population trends were represented with smoothed curves obtained by nonparametric regression using the locally weighted scatterplot smoothing (LOESS) function from R.
All statistical analysis was performed with R Statistical Package version 3.5.3. P-values<.05 were considered statistically significant.
RESULTSWe screened more than 4.9 million hospital discharge records and more than 70 000 death certificates from Catalonia produced between 2008 and 2019 to select and link 6054 fatal and nonfatal MI cases aged 35 to 74 years (4871 men, 1183 women) occurring in the study region of Girona (figure 1).
Case-selection diagram to estimate acute myocardial infarction incidence and 28-day case fatality in Girona in the population aged 35 to 74 years between 2008 and 2019, based on hospital discharge data and mortality registry
ICD, International Classification of Diseases; REGICOR, Registre Gironí del Cor (Girona Heart Registry).
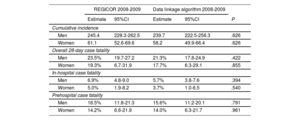
The 2008 to 2009 standardized MI incidence and the prehospital, in-hospital, and overall 28-day case fatality computed with the electronic LDM for the population aged 35 to 74 years did not significantly differ from the MI registry data for the REGICOR population (table 1). Estimates did not significantly differ by sex or by case fatality subtype.
REGICOR reference standardized myocardial infarction incidence rate per 100 000 inhabitants and 28-day case fatality results compared with hospital admissions and mortality registry figures obtained by the data linkage algorithm: for the population aged 35 to 74 years from 2008 to 2009, stratified by sex
| REGICOR 2008-2009 | Data linkage algorithm 2008-2009 | ||||
|---|---|---|---|---|---|
| Estimate | 95%CI | Estimate | 95%CI | P | |
| Cumulative incidence | |||||
| Men | 245.4 | 228.3-262.5 | 239.7 | 222.5-256.3 | .626 |
| Women | 61.1 | 52.6-69.6 | 58.2 | 49.9-66.4 | .626 |
| Overall 28-day case fatality | |||||
| Men | 23.5% | 19.7-27.2 | 21.3% | 17.8-24.9 | .422 |
| Women | 19.3% | 6.7-31.9 | 17.7% | 6.3-29.1 | .855 |
| In-hospital case fatality | |||||
| Men | 6.9% | 4.8-9.0 | 5.7% | 3.8-7.6 | .394 |
| Women | 5.0% | 1.9-8.2 | 3.7% | 1.0-6.5 | .540 |
| Prehospital case fatality | |||||
| Men | 16.5% | 11.8-21.3 | 15.6% | 11.2-20.1 | .791 |
| Women | 14.2% | 6.6-21.9 | 14.0% | 6.3-21.7 | .961 |
95%CI, 95% confidence interval; REGICOR, Registre Gironí del Cor.
In the population aged 35 to 74 years, women represented approximately 20% of the MI cases over the entire study period (ie, a 1:4 ratio). MI incidence trends for men aged 35 to 74 years showed a significant nonlinear trend with a joinpoint at 1994 in men, after which there was a significant 4.2% APC decrease. For women, the trend was linear with a significant steady APC decrease of 0.96% in the study period (figure 2). The average MI incidence rate from 1990 to 1994 was 310 (95%CI, 200-420) in men and 76 (95%CI, 53-99) in women, and 238 (95%CI, 188-288) and 60 (95%CI 48-72), respectively, from 2015 to 2019 (table 1 of the supplementary data).
Population trends of acute myocardial infarction (MI) incidence in the REGICOR (Registre Gironí del COR or Girona Heart Registry) region from 1990 to 2019 in the population aged 35 to 74 years by sex: joinpoints and annual percent change (APC) with 95% confidence interval (95%CI).
The 28-day case fatality showed a 3-phase trend between 1990 and 2019. In men, there was a significant annual decrease between 1995 and 2019, which was larger from 1995 to 2004 (–2.4%) than from 2004 to 2019 (–0.5%). In women, there was a significant annual reduction from 1995 to 2003 (APC=–3.8%) (figure 3). The average MI case fatality rate from 1990 to 1994 was 44% (95%CI, 38-50) in men and 49% (95%CI, 25-73) in women, and 20% (95%CI, 18-22) in men and 17% (95%CI, 11-23) in women from 2015 to 2019 (table 2 of the supplementary data).
Population trends of acute myocardial infarction (MI) 28-day case fatality in the REGICOR (REgistre GIroní del COR or Girona Heart Registry) region from 1990 to 2019 in the population aged 35 to 74 years by sex: joinpoints and annual percent change (APC) with 95% confidence interval (95%CI).
Prehospital case fatality increased significantly between 1990 and 1995 in men (APC=2.2%), followed by a sharp decrease between 1995 and 2004 (APC=–1.8%), and stabilized thereafter (figure 4). In women, a decrease was also observed from 1995 to 2003 (APC=–3.2%). The average prehospital MI case fatality rate from 1990 to 1994 was 28% (95%CI, 24-32) in men and 34% (95%CI, 16-52) in women, and was 15% (95%CI, 13-17) in men and 14% (95%CI, 9-19) in women from 2015 to 2019 (table 3 of the supplementary data).
Population trends of acute myocardial infarction (MI) prehospital case fatality in the REGICOR (REgistre GIroní del COR or Girona Heart Registry) region from 1990 to 2019 in the population aged 35 to 74 years by sex: joinpoints and annual percent change (APC) with 95% confidence interval (95%CI).
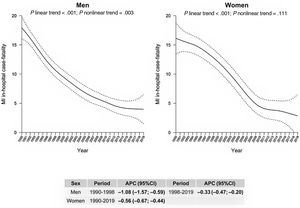
In contrast, in-hospital case fatality steadily decreased in women between 1990 and 2019 (APC=0.6%). Similarly, men experienced a reduction between 1990 and 1998 (APC=–1.08%) and from 1998 to 2019 (APC=0.33%) (figure 5). The average in-hospital MI case fatality rate from 1990 to 1994 was 16% (95%CI, 14-18) in men and 16% (95%CI, 9-23) in women, and was 4% (95%CI, 4-4) in men and 3% (95%CI, 2-4] in women from 2015 to 2019 (table 4 of the supplementary data).
Population trends of acute myocardial infarction (MI) in-hospital case fatality in the REGICOR (REgistre GIroní del COR or Girona Heart Registry) region from 1990 to 2019 in the population aged 35 to 74 years by sex: joinpoints and annual percent change (APC) with 95% confidence interval (95%CI).
The stratification of MI prehospital case fatality and incidence by age groups 35-44, 45-54, 55-64, and 65-74 years, showed similar trends in MI incidence except in women aged 65-74 years, who departed from the general decreasing trend (Figures 1 and 2 of the supplementary data).
In addition, we compared 28-day case fatality in hospitalized MI patients from 2008 to 2019 by dividing them in ST-segment elevation myocardial infarction (STEMI) (ICD-9 codes 410.0-410.6 and 410.8, and ICD-10 code I21. 3), non-STEMI (non-STEMI) (ICD-9 codes 410.7 and 410.9, and ICD-10 code I22.2) and undetermined with the remaining codes used to identify MI patients in our algorithm (see details in Methods section), with 2263, (48%), 1177 (21%) and 1516 (23%) patients, respectively. Their case fatality was 3.7%, 1.4% and 5.9%, respectively. STEMI and non-STEMI case fatality figures statistically differed, and undetermined MI type case fatality was significantly higher than the rest (all P<.003).
DISCUSSIONWe validated a LDM to estimate MI incidence and case fatality in the population aged 35 to 74 years in the province of Girona in the north-east of Spain. Our method yielded similar estimates to those of the REGICOR population-based registry, which operated in the same area until 2009. Data from the last 30 years in that region, showed a decrease in MI incidence since the 1990s in both men and women. Case fatality declined from the 1990s to 2000s, although most case fatality indicators, particularly, prehospital indicators, stabilized around 2002 to 2005 at around 15%. However, sudden death still took heavy toll in coronary heart disease, which should be addressed by public health authorities. The STEMI and non-STEMI 28-day case fatality remained stable at around 5% in the last decade studied (2010-2019) and the overall case fatality rate in patients hospitalized with an MI is now one-fourth of that in the 1990s, likely due to reduced revascularization times in STEMI.
To ensure optimal quality, the linkage of hospitalization and mortality data to estimate MI incidence and case fatality must be validated with exhaustive population-based registries, as has been done in Finland and UK studies.13,20,21 A lack of validation studies could explain the discrepancies observed between health care and registry data in Norway.17 In our case, the accuracy of LDM to assess the burden of MI in the province of Girona was tested against the REGICOR MI registry population data. Our results showed similar estimates in the LDM and the REGICOR registry, suggesting that the LDM can reliably be applied to the population aged 35 to 74 years, and revealed that the prehospital portion (ie, attributable to sudden death) remained stable at around 15% by the end of the study period.
In Finland, the FINMONICA and FINAMI population registries have successfully validated comparable procedures with similar ICD code selection.13 Sensitivity was higher for patients who died within 28 days after symptom onset of the index hospitalization (> 90%) and was lower for patients aged 75 years or older (< 80%). Other studies have estimated the specificity and sensitivity of a comparable procedure to establish the incidence of nonfatal coronary heart disease and stroke in a cohort21 rather than a population MI registry; sensitivity was very high (> 92% for men and women in all age groups, 96% overall) and specificity was only fair (> 60% in all subgroups, 70% overall) for detection of those events in the cohort.
Of note, before 1990, hospital records contained more coding errors, compared with recent data, which contributed to poor specificity and sensitivity.12,20 Linking electronic hospitalization and mortality data may provide a more reliable indicator that is relatively easy to apply, which would contribute to public health policy and responses related to MI incidence and case fatality. After validation, this LDM could be implemented in other Spanish or European regions to facilitate comparison of MI incidence and case fatality among different locations as well as their trends. MI incidence estimates were calculated in 1997 and 1998 in several Spanish regions and showed significant differences. Analyzing the incidence trends could help to better understand this interregional variability in MI mortality rates, which has also been observed for decades among Spanish regions.28 MI incidence trends were estimated for a shorter period several years ago in several European countries, and all participating regions showed similar slow reduction trends to those found in our study.4 These findings indicate the importance of monitoring the trends of the burden of MI, not only with population mortality rates but also with reliable estimates of population incidence.
The definition of fatal and nonfatal cases must be standardized in LDM estimation of coronary heart disease burden because sex and age characteristics of prehospital case-fatalities may differ from those of hospitalized patients. Regional and country variability in the diagnosis of sudden or out-of-hospital deaths could hamper comparison of 28-day case fatality data, particularly for prehospital deaths. Calculation of long-term trends of MI incidence requires the adjustment of older MI definitions (eg, regarding troponin sensitivity).4,10 This adjustment does not vary across Europe, as shown by studies that applied very similar adjusted definitions in southern and northern Europe.4,27 To preserve comparability, we used published definitions in our adjusted estimates to calibrate pre-2000 rates.
We found a decline in MI incidence until 2019 in our data, consistent with the observation of declining MI hospitalization rates and case fatality from 1997 to 2011 in the United States.29 Throughout Europe, there was also a steady decrease in the age-adjusted incidence rates of MI for both sexes from 1990 to 2017.30 Specifically, recent studies have shown declining MI incidence and case fatality in the Netherlands,16 Sweden,18 Finland and in regions of France, Germany, Italy, and Spain,4 as well as in Zagreb, Croatia.31 A decline in MI incidence and in first hospitalizations for MI has been reported in Norway17 and Denmark,14 respectively. Finally, in Estonia, where MI case fatality has decreased in the whole population, incidence has diminished only in women, remaining stable in men.4 For most other European regions, data are unavailable or have not been obtained with a common standard protocol, hampering comparability.
Despite the evidence of declining case fatality, the data for an out-of-hospital decrease are less clear. In Sweden and the United States, studies in the first decade of the 2000s already showed a greater case fatality decrease for in-hospital cases compared with out-of-hospital cases.29,30 In our study, the decline in prehospital case fatality ended in the early 2000s, as also observed in Augsburg (Germany) and in Brianza/Varese (Italy).4 This stabilization of prehospital case fatality trends may be related to the unchanged trends in delayed arrival to hospitals among persons with MI symptoms.31,32
Our findings indicate that both AMI incidence and case fatality tended to decrease in the recent 30-year study period. However, all trends tended to flatten in the last decade, with prehospital case fatality remaining as high as 15% (figure 4, figure 6). Automatic external defibrillators were deployed in public areas in 2011 and primary prevention successfully reduced some risk factors (cholesterol and hypertension).33,34 The reasons for this stagnation remain to be identified. However, several candidate factors can be suggested: the increasing obesity pandemic and the growing prevalence of type 2 diabetes mellitus.35,36
The MDS covers the 88 hospitals in Catalonia that provide acute care,37 thereby recording all patients admitted for MI. Hospital transfers generate duplicate patient records; however, each patient is identified with a unique code, making it possible to track transferred patients and follow-up each case. The mortality registry, which includes the same identification code, was used to detect out-of-hospital MI deaths. Furthermore, including the “fatal case with insufficient data” MONICA MI category protects against underestimating the actual MI incidence because this category includes approximately 12% of all cases, which in turn represent about 20% of fatal cases. In addition, the validity of the MDS and mortality registry coding for cardiovascular diseases has previously been examined and confirmed.24,25 Finally, the decrease in incidence and case fatality parallels that of MI population mortality rates.38,39
We limited the age range to 35 to 74 years because there are very few MI cases in individuals younger than 34 years and because the diagnostic precision of MI in death certificates has been validated for that age range alone.25
CONCLUSIONSIn Girona, the MI incidence and case fatality started to significantly decrease around 1990 to 1995 in the population aged 35 to 74 years. The decrease in incidence was sharper in men, and the decrease in case fatality was initially sharper in women. Overall, the incidence decrease was slow but continuous. Unfortunately, the prehospital case fatality of MI remains around 15%, presumably due to sudden death, and all subtypes of case fatality trends flattened at the end of the study period. STEMI and non-STEMI case fatality was around 5% between 2008 and 2019.
FUNDINGThis study was funded by the Carlos III Health Institute and the European Regional Development Fund (FIS-14/00449, FIS-PI081327, FIS-INTRASALUD-PI1101801, PI21/00163, PI21/00040, CB16/11/00229 from CIBERCV, CB06/02/0029 from CIBERESP), Agència de Gestió d’Ajuts Universitaris de Recerca (AGAUR) of Catalonia (2021SGR00144).
ETHICAL CONSIDERATIONSThe project was approved by the Parc de Salut Mar ethics committee (95/548/I and 2015/6420/I).
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCENone.
AUTHORS’ CONTRIBUTIONSDesigned the REGICOR reference study or the Linked-Data Method: J Marrugat, I R Dégano, J Sala, R. Masia, R. Elosua, R. Ramos.
Fundraising for the project: J. Marrugat, J. Sala, R. Ramos, R. Elosua.
Statistical analysis: I. Subirana, A. Camps-Vilaró, I. R. Dégano.
Statistical analysis interpretation: J. Marrugat, I. R. Dégano, J. Sanchis, R. Masia, R. Elosúa, I. Palomo, M. Cainzos-Achirica, H. Tizón-Marcos, I. Subirana, R. Ramos.
Manuscript preparation: A. Camps, J. Marrugat, I.R. Dégano.
Manuscript approval: A. Camps, J. Marrugat, I. R. Dégano, J. Sala, R. Masia, R. Elosua, I. Palomo, J. Sanchis, H. Tizón-Marcos, I. Subirana, R. Ramos, M. Cainzos-Achirica.
CONFLICTS OF INTERESTJ. Sanchis is editor-in-chief of Rev Esp Cardiol. The journal's editorial procedure to ensure impartial handling of the manuscript has been followed. The remaining authors declare no conflicts of interest regarding this manuscript.
The authors are grateful to the PADRIS (Programa d’Analítica de Dades per a la Recerca i la Innovació en Salut [Data Analysis Program for Health Research and Innovation]) staff for their support in the extraction of hospital admissions and mortality data. The REGICOR contributors appear in full roster at the REGICOR website.40