Keywords
INTRODUCTION
Atrial function has been studied under different clinical and experimental conditions. The contribution of the left atrium to ventricular filling has been used to evaluate atrial contractile function.1,2 Non-invasive estimation of left atrial contraction has normally been done assessing transmitral blood flow using conventional pulsed Doppler echocardiography. New tools, such as automatic boundary detection, have made it possible to validate various indexes of both systolic and diastolic left atrial function.3
Pulsed wave tissue Doppler imaging (PW-TDI) is a relatively new echocardiography tool for analyzing high amplitude and low frequency Doppler signals from the cardiac muscle.4 An excellent signal-to-noise ratio and the possibility of analyzing the data quantitatively are some of the new and attractive advantages of PW-DTI.5 This technique has been used to evaluate velocities and time intervals of the contraction and relaxation of both ventricles in different clinical situations.6-10 However, there are very few studies that have provided quantitative data on atrial function using PW-DTI.11
The aims of the present study were: a) to analyze and attempt to describe PW-TDI spectral patterns of the left atrial wall; b) to evaluate the reproducibility of the technique; and c) to study the relationship between PW-TDI patterns of the left atrium and those obtained through conventional pulsed Doppler echocardiography from transmitral and pulmonary vein flow velocities.
PATIENTS AND METHOD
Study Population
We studied left atrial wall velocities with PW-TDI in a consecutive group of subjects selected in the echocardiography laboratory when, regardless of the reason for the test, the echocardiographic studies were reported as normal and there was correct visualization of the atrial walls in the echocardiographic apical 4 chamber view. Exclusion criteria were as follows: a) the presence of structural heart disease; b) anomalies in baseline ECG, including the presence of a non-sinus rhythm; and c) unsuitable or poor quality spectral recordings with PW-TDI and conventional pulsed Doppler echocardiography. To account for the effect of aging on the normal patterns of conventional pulsed Doppler echocardiography as well as its possible effects on those of atrial PW-TDI, the study population was arbitrarily divided into 2 groups: group I (age <45 years) and group II (age >45 years). Thus, the first group included children, adolescents and young adults, and the second, older adults and elderly people. The centers' Ethics and Clinical Trials Committee approved the study and informed consent was obtained in all cases. All the echocardiographic and Doppler studies were carried out by two observers (MPP and DMG).
Transthoracic Echocardiogram
All the subjects underwent complete conventional bidimensional echocardiography. The anteroposterior dimension of the left atrium was obtained in M-mode from the parasternal long axis. The end-diastolic and end-systolic volumes of the left ventricle were measured in the apical 4 chamber view and the ejection fraction was calculated with Simpson's modified rule.
Pulsed Wave Tissue Doppler Imaging Acquisition of the Left Atrial Wall
The studies were done with the Sonos 5.500 system (Philips Medical System) via a wideband transducer (S4 fusion imaging: 2-4 MHz) and data digitally stored on optical disc for later analysis. The PW-TDI spectral signal filters were adjusted to obtain a Nyquist limit of ±20 cm/s. Gain was minimized to obtain a clear signal from the tissue with the lowest background noise possible. All the subjects were studied in the left lateral position in the end phase of expiration and in the apical 4 chamber view. The lateral wall of the left atrium was divided into 3 segments: basal, medial, and distal. The tissue Doppler imaging sample volume was placed in the center of these consecutive segments for analysis. Special care was taken to place the sample volume within the endocardial boundary to avoid the pulmonary vein entrance. The position of the transducer was adjusted to obtain the best possible alignment with the atrial wall. When analyzing the PW-TDI curve, the sample volume moved outside (epicardium) and inside the muscle of the atrial wall (atrial cavity) to ensure that the recording was obtained from the center of the wall. Likewise, when analyzing the basal lateral segment of the left atrium, it was of particular interest to move away from the mitral valve ring, so that in all cases the recording obtained was verified as differing in its morphology and velocity from the one obtained by placing the sample volume on the mitral ring. The PW-TDI measurements were determined by averaging the results obtained in the basal and medial segments of the lateral wall of the left atrium after interrogating each one 3 times. Simultaneous electrocardiographic recording made it possible to identify the different phases of each cardiac cycle such that the exact moment of each of the Doppler signals could be specified.
Flow Analysis Via Conventional Pulsed Doppler Echocardiography
Transmitral flow tracings were obtained with conventional pulsed Doppler echocardiography in the apical 4 chamber view with the sample volume placed at the free ends of both mitral leaflets. At the end of expiration the following parameters were obtained: E-wave velocity, A-wave velocity, E/A ratio, E-wave deceleration time (the slope from the peak of the E-wave to the baseline value), and isovolumetric relaxation time (interval from the closing of the aortic valve to the beginning of ventricular filling). Likewise, the pulsed Doppler echocardiography recordings of the left upper pulmonary vein were obtained by placing the sample volume approximately 1 cm within the vein. All the tracings were obtained during an apnea phase. The different measurements carried out in the pulmonary vein were: S-wave velocity, D-wave velocity, S/D ratio, and retrograde atrial A'-wave velocity. The mean of at least three consecutive beats was calculated.
The filling patterns used to characterize diastolic physiology were: normal, alterations in relaxation, pseudonormal, and restrictive, in line with conventional echocardiographic criteria.12
Statistical Analysis
The results are expressed as mean ± standard deviation (SD). The normal distribution of all the quantitative variables was verified with the Kolmogorov-Smirnov test with Lilliefors correction. Means were compared with Student's t test. Chi-squared test was used for the qualitative variables. Pearson's correlation test was used to obtain correlations between the PW-TDI velocities and the transmitral and pulmonary vein flow velocities. The kappa coefficient was used to study concordance between the atrial velocities obtained through PW-TDI and blood flow velocities determined by conventional pulsed Doppler echocardiography (atrial PW-TDI vs transmitral flow and atrial PW-TDI vs pulmonary vein flow). The kappa index indicates moderate agreement if it is >0.4, marked agreement if >0.6, high agreement if >0.8 and absolute agreement if =1.13 All comparisons were bilateral and were considered significant at a P-value of <.05. To evaluate interobserver variability, the data were evaluated by 2 independent observers. In 30 subjects, a single observer repeated the measurements to calculate intraobserver variability. Intraobserver and interobserver variability for the measurement of atrial PW-TDI velocities and the transmitral and pulmonary vein flow velocities were calculated with the intraclass correlation coefficient. Values <0.4 indicate low reliability; between 0.4 and 0.75 adequate to good, and >0.75 excellent reliability.14
RESULTS
Characteristics of the Population
The demographic and echocardiographic characteristics of the study population are shown in Table 1. We evaluated 110 subjects and 90 of these entered the study: there were 50 women and 40 men with a mean age of 48±22 years (range, 9-75 years). Twenty subjects were rejected because the PW-TDI recordings were unsuitable. Despite the 2 study groups were quite homogeneous, the subjects in group II (age >45 years) presented higher systolic blood pressure and greater atrial size. Age was closely correlated to the size of the left atrium (r=0.7; P<.001). In addition, differences were found in transmitral and pulmonary vein flow velocities in both groups, as shown in Table 1.
Pulsed Wave Tissue Doppler Imaging of the Left Atrial Wall
The left atrial wall generates a triphasic signal formed by a positive A1 wave, followed by two negative A2 and A3 waves. The time sequence of the ECG, left atrial flow and transmitral and pulmonary vein flow indicate that the A1 component of the atrial wall occurs during ventricular systole and corresponds to the atrial relaxation period. This wave could be due to the movement of the mitral ring during ventricular systole towards the base of the left atrial wall. The A2 wave is produced during early diastolic filling (the passive phase of ventricular filling) and the A3 wave coincides with atrial contraction (late ventricular or active filling).
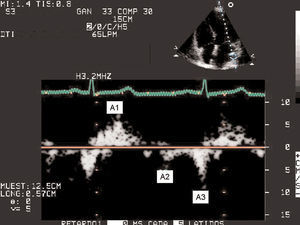
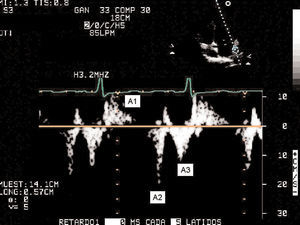
The youngest subjects (group I) present a high-velocity A2 wave pattern and an A2/A3 ratio >1 (Figure 1). As age increases (group II), the A2 wave velocity decreases whereas that of the A3 wave increases. This means that the A2/A3 ratio is >1 (Figure 2). These differences between groups were statistically significant, as shown in Table 2. In contrast, no differences were found in the A1 wave velocities between the 2 age groups (13.5±3.9 cm/s in group I vs 13.1±5.4 cm/s in group II; P=.59).
Fig. 1. Spectral recording of pulsed wave tissue Doppler echocardiography in group I (age <45 years).
Fig. 2. Spectral recording of pulsed wave tissue Doppler echocardiography in group II (age >45 years).
Relationship Between Transmitral Flow Patterns and Atrial Pulsed Wave Tissue Doppler Imaging Patterns
The mean velocities of the E and A waves, E/A ratio, E-wave deceleration time, and isovolumetric relaxation time in both groups are shown in Table 1. We found that the mean velocity of the E wave was directly correlated with that of the A2 wave (r=0.55; P<.001) and inversely with the atrial PW-TDI A3 wave (r=-0.52; P<.001). Likewise, the greater the transmitral flow A wave velocity the greater the A3 wave velocity (r=0.55; P<.001) and the lower the atrial PW-TDI A2 wave velocity (r=-0.52; P<.001). When the transmitral and atrial PW-TDI flow patterns were analyzed as a whole, a moderate concordance between them was found (kappa =0.584; P<.0001). This concordance stayed constant in all the age groups (Table 3).
Relationship Between the Pulmonary Vein and Atrial Pulsed Wave Tissue Doppler Imaging Flow Patterns
A reduction in anterograde diastolic D-wave velocity occurred in pulmonary vein flow with age (51.9±13.9 vs 42.7±13.4 cm/s; P=.01) without significant changes in anterograde systolic S-wave velocity (62.9±14.1 vs 57.4±14.3 cm/s; P=.15). Retrograde atrial wave (A') velocity increased with time from 15.1±6.5 to 19.4±8.0 cm/s (P=.02). Despite these changes, the S/D ratio remained >1 in most of the subjects studied. These evolutionary patterns seem to be due to the steady increase in the contribution of atrial contraction to ventricular filling. Regarding atrial PW-TDI, a weak inverse correlation was found between A3-wave velocity and D-wave velocity in pulmonary vein flow (r=-0.34; P=.01) and a positive correlation, also weak, between atrial PW-TDI A2/A3 ratio and D-wave velocity in pulmonary vein flow (r=0.41; P=.002).
Interobserver and Intraobserver Variability
The interobserver and intraobserver variability for the measurements of all the left atrium PW-TDI parameters (A1, A2, A3, and A2/A3) and the transmitral and pulmonary vein flow velocities measured by the intraclass correlation coefficient were 0.65 and 0.60, respectively.
DISCUSSION
The main finding of the present work is that the left atrial wall shows a typical and replicable PW-TDI pattern made up of three waves, one positive (A1) and two negative (A2 and A3), that seem to correspond, respectively, to atrial relaxation, early ventricular filling and atrial contraction. Furthermore, quantitative data on the left atrial wall velocities have been obtained from a group of subjects without structural heart disease over a broad age range. As far as we know, this is the first work that attempts to approach the study of left atrial function via PW-TDI and which provides morphological and quantitative information.
Left Atrial Function
Left atrial function has been widely studied.15-17 In essence, the atrial cavity acts as a reservoir because this cavity receives blood during ventricular systole. In addition, it functions as a conduit or passage for blood from the pulmonary veins to the ventricular cavity during ventricular diastole. Finally, it has an important booster pump function (when sinus rhythm is present) due to its capacity for presystolic contraction that coincides with the active phase of left ventricle filling during late diastole. This booster pump function plays an important role in the maintenance of cardiac output in patients with severe systolic dysfunction.
In this work we have shown that it is possible to try to evaluate the function of the left atrium through PW-TDI, since each wave of the tissue pattern described seems to correspond to each of the main actions of the left atrium during the cardiac cycle. Thus, the A1 wave corresponds to the reservoir function, the A2 wave to the blood conduit or passage function and the A3 wave to the atrial contraction function. Furthermore, in accordance with what truly occurs, we showed that the atrial contraction wave acquires greater prominence with the age.
The contribution of atrial contraction to filling has already been extensively studied through Doppler echocardiography.18,19 Thus, it has been demonstrated that this contribution depends on numerous factors, such as atrial contractility,17 preload,20 postload,21 heart rate,22 age,23 autonomic tone,24 atrioventricular conduction,25 respiration,26 and electrical cardioversion,27 among others. The mean pressure of the left atrium has been studied under different loading conditions in animals with and without mitral regurgitation. The pulmonary vein flow parameters correlated well with mean atrial pressure under such loading conditions, which in both cases show alterations.27 In a recent study of left atrial function in which acoustic quantification was used, Spencer et al.28 show that reservoir, conduit and booster pump functions can be evaluated through studying the waves obtained with automatic boundary detection.
Age-Related Changes in Doppler Echocardiography Parameters
As age increases there is a gradual reduction in the capacity of the myocardium to relax and recover its elasticity, leading to a gradual reduction of left ventricular pressure and a slowing down of ventricular filling.29 Thus, with aging, transmitral flow E-wave velocity decreases and A-wave velocity increases, leading to an E/A ratio <1, with some prolonged E-wave deceleration and isovolumetric relaxation times. In the present study, not onl y were these evolutionary changes accurately reproduced, but also, via the PW-TDI study, it was verified that the left atrium seemed to experience similar changes as well. There was a steady increase in the velocity of the wall corresponding to atrial contraction (A3) and a decrease in early ventricular filling wave velocity (A2), such that an age-related A2/A3 ratio <1 could be observed in most cases. These variations significantly correlated with those of the transmitral flow obtained through conventional pulsed Doppler echocardiography. However, the correlation between the atrial PW-TDI and pulmonary vein flow velocities was less frequent, and when significant the correlation was weak. This might be the result of the few changes that are observed over time in pulmonary vein flow patterns (slight increase in SV, slight decrease in DV and an almost constant S/D ratio >1) in subjects without concomitant structural heart disease.
Study Limitations
The limitations of the present study include the dependency of the measurements on the operators' skills and the need for a suitable acoustic window to carry out studies of acceptable quality. However, if the echocardiographist has been trained in Doppler echocardiography images and the equipment used is technologically suitable, these limitations are purely relative. The arbitrary division of the population into 2 age groups could influence the results; however, the fact that we know that Doppler echocardiography recordings offer a clear evolutionary pattern forces us to carry out an analysis of this type. New studies with a greater number of subjects could further divide the age groups to corroborate our results with greater precision.
In addition, and most importantly, we have to take into account the intrinsic limitations of the technique, such as dependency on the angle of incidence (this requires the best possible alignment between the ultrasound beam and the main displacement vector of the wall analyzed), the changing situation of the sample volume and its variable position during the cardiac cycle, and the problem of analyzing the movement of a cardiac segment as if this was taking place in a single direction and not as it actually occurs, that is, with complex movements in multiple directions. Finally, although the clinical applicability of this technique is unknown, we believe that it can open a new path to the study of atrial movement and function.
Conclusions
It is possible to replicate studies of left atrial wall velocity via PW-TDI. Pulmonary vein flow velocity and, in particular, transmitral flow velocity recordings obtained via conventional pulsed Doppler echocardiography seem to be related to the recordings of the left atrial wall obtained through PW-TDI. This makes new quantitative data available which could be useful for the study of atrial function. These data should be corroborated by studies with a more complex methodology thus leading to possible applications in different clinical and hemodynamic situations.
ACKNOWLEDGMENT
We would like to thank María Jesús Cascales, SRN, and María José G. Villalba, SRN, at our Centers' Cardiology Unit for their assistance with the study. We also thank Francisco Almagro, the Unit's secretary for his administrative support.
Correspondence: Dr. M. Pérez-Paredes.
Laboratorio de Ecocardiografía. Unidad de Cardiología.
Hospital Universitario Morales Meseguer.
Avda. Marqués de los Vélez, s/n. 30008 Murcia. España.
E-mail: matiasperez@medynet.com