A healthy lifestyle (HLS) is essential to attaining optimal cardiovascular health. Our objective was to assess the association between a HLS score and the incidence of hard cardiovascular disease (CVD) events.
MethodsThe SUN project is a dynamic, prospective, multipurpose cohort of Spanish university graduates with a retention proportion of 92%. In 19 336 participants, we calculated a HLS score ranging from 0 to 10 points: never smoking, physical activity (> 20 METs-h/wk), Mediterranean diet adherence (≥ 4/8 points), low body mass index (≤ 22), moderate alcohol intake (women, 0.1-5g/d; men, 0.1-10g/d), low television exposure (≤ 2h/d), no binge drinking (≤ 5 alcoholic drinks anytime), taking a short afternoon nap (< 30min/d), meeting up with friends> 1h/d and working> 40h/wk.
ResultsAfter a median follow-up of 10.4 years, we identified 140 incident cases of CVD. After adjustment for potential confounders, the highest category of HLS score adherence (7-10 points) showed a significant 78% relative reduction in the risk of primary CVD compared with the lowest category (0-3 points) (adjusted HR, 0.22; 95%CI, 0.11-0.46). Each healthy habit was individually associated with a lower risk of CVD.
ConclusionsA HLS score including several simple healthy habits was associated with a lower risk of developing primary CVD. This index may be useful to reinforce CVD prevention without the need to include traditional risk factors.
Keywords
Although the usefulness of cardiovascular disease risk prediction models has been demonstrated (eg, Framingham, SCORE), they first need to be adapted and calibrated for the target population. More comparable concepts (risk percentiles or vascular age) have also been proposed to reduce the possible disparities in individual risk estimates.1 Indeed, up to 20% of cardiovascular events occur in the absence of the main determinants of cardiovascular risk (hypertension, hyperlipidemia, smoking, and diabetes).2 Accordingly, new factors contributing to ideal cardiovascular health have been identified3 that underlie modifiable lifestyle factors, which would be “determinants of the determinants”. A considerable number of cardiovascular events could be prevented with prompter intervention, namely, in these previous or distal (lifestyle habits) determinants, because in preventive medicine, the early bird catches the worm.4,5 Lifestyle habits determine cardiovascular risk independently of the genetic risk category.6
The priority in cardiovascular prevention should be primordial prevention,7 which acts before risk factors develop by changing the behaviors determining them.8–10 Thus, in addition to traditional risk factors, various other habits appear to have vascular benefits: a short afternoon nap,11 little time watching television,12 a Mediterranean alcohol consumption pattern,13 spending more time with friends,14 or the number of hours working.15
Here, we longitudinally analyzed the combined impact of 10 indicators of healthy lifestyle habits on cardiovascular event risk.
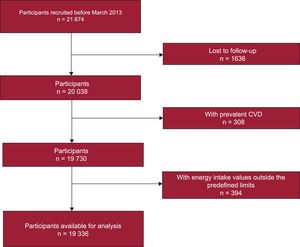
METHODSStudy PopulationSUN (“Seguimiento Universidad de Navarra” [University of Navarre Follow-up]) is a prospective, dynamic, and multipurpose cohort of Spanish university graduates that has been active since 1999. Its design has already been detailed.16 In total, 21 674 participants had been recruited by March 2013. The following individuals were excluded: those lost to follow-up (n = 1636; 92% retention), those who had baseline cardiovascular disease (CVD; acute coronary syndrome and stroke; n = 308), and those who had energy intake outside the predefined limits (n = 394; 1st and 99th percentiles for each sex). Finally, 19 336 participants remained in this study (Figure 1).
The research ethics committee of the University of Navarre approved the study protocol. Participants were informed in writing of the study characteristics, and voluntary completion of the first questionnaire was considered to automatically indicate participant consent.
Main Exposure VariablesThe baseline questionnaire collected information on sociodemographic, clinical, and lifestyle aspects and anthropometric variables. The reproducibility and validity of the reported anthropometric17 and physical activity18 data were evaluated in cohort subgroups. A previously validated19 136-question semiquantitative food-frequency questionnaire was applied. Alcohol consumption was recorded via this questionnaire and other questions related to alcohol consumption habits were included in the baseline questionnaire. Adherence to the Mediterranean diet was estimated with the score (0-8 points) developed by Trichopoulou et al.,20 although alcohol was excluded.
A score was calculated to evaluate adherence to a healthy lifestyle (HLS) (Table 1). One point was given to each participant for each of the following 10 habits: never smoking, moderate-to-high physical activity (> 20 MET-h/wk), Mediterranean diet (≥ 4 adherence points), body mass index (BMI) ≤ 22, moderate alcohol consumption (women, 0.1-5.0g/d; men, 0.1-10.0g/d; abstainers excluded), low television exposure (< 2h/d), no binge drinking (≤ 5 alcoholic drinks at anytime), taking a short afternoon nap (< 30min/d), meeting up with friends > 1h/d, and working at least 40h/wk.
Healthy Lifestyle Habit Score
| Score | |
|---|---|
| Smoking | |
| Never smoked | 1 |
| Smoked (active and exsmoker) | 0 |
| Physical activity (MET-h/wk) | |
| Physically active (> 20 MET-h/wk) | 1 |
| Not physically active (≤ 20 MET-h/wk) | 0 |
| Mediterranean diet pattern (Trichopoulou score)* | |
| High adherence (≥ 4) | 1 |
| Low adherence (< 4) | 0 |
| Body mass index | |
| ≤ 22 | 1 |
| > 22 | 0 |
| Moderate alcohol consumption | |
| Moderate consumption (women, 0.1-5.0 g/d; men, 0.1-10.0 g/d) | 1 |
| Abstention or high consumption (women, > 5 g/d; men > 10 g/d) | 0 |
| Time spent watching television | |
| Little time watching television (< 2 h/d) | 1 |
| Watching television ≥ 2 h/d | 0 |
| Binge drinking | |
| No binge drinking (≤ 5 alcoholic drinks at any time) | 1 |
| Binge drinking (> 5 alcoholic drinks at any time) | 0 |
| Having a short afternoon nap | |
| Short afternoon nap (0.1-0.5 h/d) | 1 |
| Not having afternoon nap or having a long nap (> 0.5 h/d) | 0 |
| Time with friends | |
| Spending time with friends (> 1 h/d) | 1 |
| Not spending time with friends (≤ 1 h/d) | 0 |
| Time working | |
| Long time working (≥ 40 h/wk) | 1 |
| Little time working (< 40 h/wk) | 0 |
In this HLS scale, the score obtained could range between 0 points (worst lifestyle) and 10 points (best lifestyle). Participants were categorized into 5 groups to ensure an adequate sample distribution with sufficient participants in each category.
Outcome AssessmentStudy outcomes were hard clinical events of primary CVD, defined as death from cardiovascular causes, incident nonfatal acute coronary syndrome (infarction with or without ST-segment elevation), or incident nonfatal stroke in participants without CVD at baseline. We confirmed the participants’ diagnoses reported in follow-up questionnaires (Q2-Q16) after requesting their medical records and reports by post. By reviewing the medical records, an expert committee of physicians classified the events. The “third universal definition of myocardial infarction” was applied to nonfatal coronary syndromes.21 Nonfatal stroke was defined as focal neurological deficit of sudden onset that lasted more than 24hours and had a vascular mechanism. Deaths were reported by next-of-kin, work colleagues, or postal authorities. Cardiovascular deaths were confirmed according to the 10th edition of the International Classification of Diseases via a review of medical records and reports with the permission of participants’ next-of-kin.
The Spanish National Death Index was checked every year to determine the cause of death of cohort members who died during follow-up. Information on the vital status and cause of death of the deceased was provided by the Spanish National Institute of Statistics through a specific agreement.
Assessment of CovariablesWe evaluated the prevalence of hypertension, type 2 diabetes mellitus, hypercholesterolemia, hypertriglyceridemia, and other CVDs (atrial fibrillation, paroxysmal tachycardia, coronary artery bypass surgery or another revascularization procedure, heart failure, aortic aneurysm, pulmonary embolism, and peripheral venous thrombosis).
Energy intake was calculated from the information collected in the semiquantitative food-frequency questionnaire at baseline and at the 10-year follow-up.
Statistical AnalysisThe following assumptions were made a priori: 3000 participants in each extreme HLS category; absolute risk, 1.5%; relative risk, 0.5 for high vs low levels; and 2-sided alpha risk of 5%. With these assumptions, the statistical power would be 87%.
Cox models were fitted (with age as the underlying time scale) to calculate the risk of primary CVD during follow-up according to HLS score (5 categories). Hazard ratios (HRs) and their 95% confidence intervals (95%CIs) were calculated by reference to the lowest scores (0-3). Person-years of follow-up were calculated for each participant, from the date of baseline questionnaire completion to the date of final questionnaire completion, date of death from cardiovascular causes, or date of nonfatal acute coronary syndrome or stroke, whichever occurred first. Linear trend tests were performed by considering the HLS score as a continuous variable.
A predefined multiplicative interaction was analyzed between sex and working hours (≥ 40h/wk) via a likelihood ratio test.
To control for possible confounding factors, a multivariable model was stratified by age decile and age at cohort entry. In addition, the multivariable model was adjusted for the following possible additional confounding factors: sex, type 2 diabetes mellitus, hypertension, other CVD events distinct from acute coronary syndrome and stoke, hypercholesterolemia, and hypertriglyceridemia.
To evaluate the individual contribution of each specific HLS factor to CVD risk, Cox models were fitted for each of the 10 indicators of healthy lifestyle habits by adjusting for the effect of the other HLS indicators.
A sensitivity analysis was performed to calculate the score by substituting the time spent watching television by the time spent sitting (< 2h/d) or by adjusting for the employment situation (unemployed or homemaker) and years of education (≤ 3, ≥ 4 years, master's/doctoral studies).
Because a history of CVD events distinct from acute coronary syndrome and stroke could prompt healthy changes in lifestyle habits, logistic regression models were used to analyze the association between HLS habits and other prevalent CVD events (atrial fibrillation, paroxysmal tachycardia, coronary artery bypass surgery or another revascularization procedure, heart failure, aortic aneurysm, pulmonary embolism, or peripheral venous thrombosis).
All reported P values are 2-sided and were considered statistically significant at P < .05.
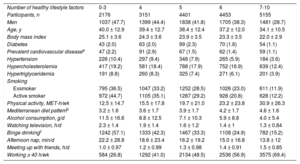
RESULTSThe participants’ baseline characteristics by HLS score are shown in Table 2. Participants with a better HLS were younger (34.1 years), were more likely to be women (71.3%), and had a lower BMI (≤ 22) and lower proportion of risk factors (diabetes, hypertension, dyslipidemia, and prevalent CVD).
Participants’ Baseline Characteristics According to the Number of Healthy Lifestyle Factors. SUN Project 1999-2017
| Number of healthy lifestyle factors | 0-3 | 4 | 5 | 6 | 7-10 |
| Participants, n | 2176 | 3151 | 4401 | 4453 | 5155 |
| Men | 1037 (47.7) | 1399 (44.4) | 1838 (41.8) | 1705 (38.3) | 1481 (28.7) |
| Age, y | 40.0 ± 12.9 | 39.4 ± 12.7 | 38.4 ± 12.4 | 37.2 ± 12.0 | 34.1 ± 10.5 |
| Body mass index | 25.1 ± 3.6 | 24.3 ± 3.6 | 23.9 ± 3.5 | 23.3 ± 3.5 | 22.0 ± 2.9 |
| Diabetes | 43 (2.0) | 63 (2.0) | 99 (2.3) | 70 (1.6) | 54 (1.1) |
| Prevalent cardiovascular diseasea | 47 (2.2) | 91 (2.9) | 67 (1.5) | 62 (1.4) | 59 (1.1) |
| Hypertension | 226 (10.4) | 297 (9.4) | 348 (7.9) | 265 (5.9) | 184 (3.6) |
| Hypercholesterolemia | 417 (19.2) | 581 (18.4) | 788 (17.9) | 752 (16.9) | 639 (12.4) |
| Hypertriglyceridemia | 191 (8.8) | 260 (8.3) | 325 (7.4) | 271 (6.1) | 201 (3.9) |
| Smoking | |||||
| Exsmoker | 795 (36.5) | 1047 (33.2) | 1252 (28.5) | 1026 (23.0) | 611 (11.9) |
| Active smoker | 972 (44.7) | 1105 (35.1) | 1287 (29.2) | 928 (20.8) | 628 (12.2) |
| Physical activity, MET-h/wk | 12.5 ± 14.7 | 15.5 ± 17.8 | 19.7 ± 21.0 | 23.2 ± 23.8 | 30.9 ± 26.3 |
| Mediterranean diet patternb | 3.2 ± 1.6 | 3.6 ± 1.7 | 3.9 ± 1.7 | 4.2 ± 1.7 | 4.6 ± 1.6 |
| Alcohol consumption, g/d | 11.5 ± 16.6 | 8.8 ± 12.5 | 7.1 ± 10.3 | 5.9 ± 8.8 | 4.0 ± 5.4 |
| Watching television, h/d | 2.3 ± 1.4 | 1.9 ± 1.4 | 1.6 ± 1.2 | 1.4 ± 1 | 1.3 ± 0.84 |
| Binge drinkingc | 1242 (57.1) | 1333 (42.3) | 1467 (33.3) | 1108 (24.9) | 782 (15.2) |
| Afternoon nap, min/d | 22.2 ± 28.8 | 18.6 ± 23.4 | 16.2 ± 19.2 | 15.0 ± 16.8 | 13.8 ± 12 |
| Meeting up with friends, h/d | 1.0 ± 0.97 | 1.2 ± 0.99 | 1.3 ± 0.98 | 1.4 ± 0.91 | 1.5 ± 0.85 |
| Working ≥ 40 h/wk | 584 (26.8) | 1292 (41.0) | 2134 (48.5) | 2536 (56.9) | 3575 (69.4) |
Data represent No. (%) or mean ± standard deviation.
Atrial fibrillation, paroxysmal tachycardia, coronary artery bypass surgery or another revascularization procedure, heart failure, aortic aneurysm, pulmonary embolism, or peripheral venous thrombosis.
Participants were followed up for a median of 10.4 years. There were 140 incident cases of CVD (0.72%): 37 deaths from cardiovascular causes (26.4%), 64 nonfatal acute coronary syndromes (45.7%), and 39 nonfatal strokes (27.9%).
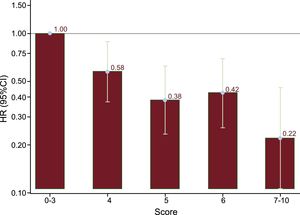
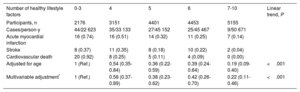
Participants with a better HLS (7-10 points) showed a significant and inverse association with risk of primary cardiovascular events vs the worst HLS category (0-3 points) (HR, 0.22; 95%CI, 0.11-0.46; linear trend P < .001) (Table 3).
Hazard Ratio (95% Confidence Interval) of Incident Cardiovascular Disease (Cardiovascular Disease, Acute Myocardial Infarction, and Stroke) According to the Number of Healthy Lifestyle Factors. SUN Project 1999-2017
| Number of healthy lifestyle factors | 0-3 | 4 | 5 | 6 | 7-10 | Linear trend, P |
|---|---|---|---|---|---|---|
| Participants, n | 2176 | 3151 | 4401 | 4453 | 5155 | |
| Cases/person-y | 44/22 623 | 35/33 133 | 27/45 152 | 25/45 467 | 9/50 671 | |
| Acute myocardial infarction | 16 (0.74) | 16 (0.51) | 14 (0.32) | 11 (0.25) | 7 (0.14) | |
| Stroke | 8 (0.37) | 11 (0.35) | 8 (0.18) | 10 (0.22) | 2 (0.04) | |
| Cardiovascular death | 20 (0.92) | 8 (0.25) | 5 (0.11) | 4 (0.09) | 0 (0.00) | |
| Adjusted for age | 1 (Ref.) | 0.54 (0.35-0.84) | 0.36 (0.22-0.59) | 0.39 (0.24-0.64) | 0.19 (0.09-0.40) | <.001 |
| Multivariable adjustment* | 1 (Ref.) | 0.58 (0.37-0.89) | 0.38 (0.23-0.62) | 0.42 (0.26-0.70) | 0.22 (0.11-0.46) | <.001 |
Unless otherwise indicated, the data represent No. (%) or hazard ratio (95% confidence interval).
The relationship between a better score on the healthy lifestyle index and lower risk of primary CVD is shown in Figure 2.
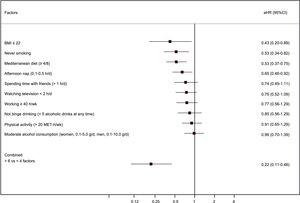
The score estimates of all healthy habit indicators were individually associated with a lower risk of cardiovascular events (Table 4). However, the greatest benefit in terms of a decreased risk of primary CVD was obtained using a combination of all lifestyle habits in the HLS score (Figure 3).
Hazard Ratio (95% Confidence Interval) of Incident Cardiovascular Disease (Cardiovascular Disease, Acute Myocardial Infarction, and Stroke) According to Healthy Lifestyle Habits. SUN Project 1999-2017
| Participants, n | Cases/person-y | Adjusted by age | Multivariable adjustmenta | |
|---|---|---|---|---|
| Abstinence from smoking | ||||
| No (active smokers and exsmokers) | 10 153 | 113/104 317 | 1 (Ref.) | 1 (Ref.) |
| Yes | 9183 | 27/92 729 | 0.49 (0.32-0.75) | 0.53 (0.34-0.82) |
| Physical activity (> 20 MET-h/wk) | ||||
| No | 11 382 | 85/118 324 | 1 (Ref.) | 1 (Ref.) |
| Yes | 7954 | 55/78 722 | 0.94 (0.66-1.33) | 0.91 (0.65-1.29) |
| Mediterranean diet patternb | ||||
| No | 7526 | 59/78 809 | 1 (Ref.) | 1 (Ref.) |
| Yes | 11 810 | 81/118 237 | 0.54 (0.38-0.77) | 0.53 (0.37-0.75) |
| Body mass index (≤ 22) | ||||
| No | 11 895 | 132/120 608 | 1 (Ref.) | 1 (Ref.) |
| Yes | 7441 | 8/76 437 | 0.31 (0.15-0.64) | 0.43 (0.20-0.89) |
| Moderate alcohol consumptionc | ||||
| No | 9967 | 77/101 297 | 1 (Ref.) | 1 (Ref.) |
| Yes | 9369 | 63/95 748 | 1.05 (0.75-1.47) | 0.99 (0.70-1.39) |
| Time spent watching television | ||||
| ≥ 2 h/d | 5684 | 55/58 711 | 1 (Ref.) | 1 (Ref.) |
| < 2 h/d | 13 652 | 85/138 335 | 0.71 (0.50-1.00) | 0.75 (0.52-1.09) |
| Binge drinkingd | ||||
| Binge drinking | 5932 | 36/60 472 | 1 (Ref.) | 1 (Ref.) |
| Never binge drinking | 13 404 | 104/136 574 | 0.75 (0.50-1.13) | 0.85 (0.56-1.29) |
| Short afternoon nap (0.1-0.5 h/d) | ||||
| Not taking afternoon nap or having a long nap | 8308 | 72/86 031 | 1 (Ref.) | 1 (Ref.) |
| Yes | 11 028 | 68/111 014 | 0.63 (0.45-0.89) | 0.65 (0.46-0.92) |
| Spending time with friends (> 1 h/d) | ||||
| No | 7374 | 102/76 395 | 1 (Ref.) | 1 (Ref.) |
| Yes | 11 962 | 38/120 651 | 0.69 (0.46-1.04) | 0.74 (0.49-1.11) |
| Time spent working, h/wk | ||||
| < 40 h/wk | 9215 | 79/93 433 | 1 (Ref.) | 1 (Ref.) |
| ≥ 40 h/wk | 10 121 | 61/103 612 | 0.88 (0.61-1.25) | 0.77 (0.53-1.11) |
Unless otherwise indicated, the data represent hazard ratio (95% confidence interval).
Adjusted by sex, age, year of questionnaire completion, diabetes, cardiovascular disease, hypertension, hypercholesterolemia, hypertriglyceridemia, and all variables shown in the Table.
As expected, participants with higher cumulative exposure to smoking (> 20 packets/y) had a higher risk of CVD than those who had never smoked (HR, 2.39; 95%CI, 1.41-4.04), and active smokers (HR, 2.74; 95%CI, 1.69-4.43) had higher risk than exsmokers (HR, 1.49; 95%CI, 0.92-2.42) vs those who had never smoked. There were no significant differences for each category for the time since smoking cessation.
Multiple sensitivity analyses were performed with the other possible confounding factors listed in the Methods section and, for all factors, the calculated estimates were maintained in the same direction as the estimates obtained in the main analyses.
A history of other CVDs (eg, atrial fibrillation, heart failure, pulmonary embolism) was associated with higher CVD risk and a healthier lifestyle. However, the only habit directly associated with a history of other CVDs was no binge drinking. There was no other significant association for the other factors used in the score. Thus, the possible confounding effect of history of other CVDs was probably not relevant in this study (Table 5).
Odds Ratio (95% Confidence Interval) of Prevalent C ardiovascular Disease (Atrial Fibrillation, Paroxysmal Tachycardia, Doronary Artery Bypass Surgery or Another Revascularization Procedure, Heart Failure, Aortic Aneurysm, Pulmonary Embolism, or Peripheral Venous Thrombosis) According to Healthy Lifestyle Habits. SUN Project 1999-2017
| Cases, n | OR (95%CI)a | |
|---|---|---|
| Abstinence from smoking | ||
| No (active smokers and exsmokers) | 211 | 1 (Ref.) |
| Yes | 115 | 0.95 (0.75-1.19) |
| Physical activity (> 20 MET-h/wk) | ||
| No | 187 | 1 (Ref.) |
| Yes | 139 | 1.04 (0.82-1.31) |
| Mediterranean diet patternb | ||
| No | 97 | 1 (Ref.) |
| Yes | 229 | 1.03 (0.80-1.31) |
| Body mass index (≤ 22) | ||
| No | 263 | 1 (Ref.) |
| Yes | 63 | 0.96 (0.69-1.33) |
| Moderate alcohol consumptionc | ||
| No | 186 | 1 (Ref.) |
| Yes | 140 | 0.88 (0.70-1.11) |
| Time spent watching television | ||
| ≥ 2 h/d | 104 | 1 (Ref.) |
| < 2 h/d | 222 | 0.96 (0.75-1.22) |
| Binge drinkingd | ||
| Binge drinking | 68 | 1 (Ref.) |
| Never binge drinking | 258 | 1.25 (0.95-1.65) |
| Short afternoon nap (0.1-0.5 h/d) | ||
| Not taking afternoon nap or having a long nap | 145 | 1 (Ref.) |
| Yes | 181 | 0.89 (0.71-1.11) |
| Spending time with friends (> 1 h/d) | ||
| No | 184 | 1 (Ref.) |
| Yes | 142 | 1.05 (0.83-1.33) |
| Time spent working | ||
| < 40 h/wk | 177 | 1 (Ref.) |
| ≥ 40 h/wk | 149 | 0.70 (0.55-0.90) |
95%CI, 95% confidence interval; OR, odds ratio.
There was no significant interaction between sex and working hours (≥ 40h/wk; P for interaction = .951).
DISCUSSIONThis prospective cohort study found an inverse association between a HLS score and CVD risk. This score combines traditional indicators of lifestyle habits (never smoking, physical activity, Mediterranean diet, BMI ≤ 22, and moderate alcohol consumption) with other factors not typically included in cardiovascular risk scores (television exposure < 2h/d, no binge drinking, taking a short afternoon nap, meeting up with friends more than 1h/d, and working at least 40h/wk).
Not smoking, performing physical activity, and having a healthy diet pattern are habits proposed by the American Heart Association to improve cardiovascular health.22 However, other lifestyle factors can effectively prevent CVDs.2
Other studies23,24 have analyzed the combined impact of various lifestyle habits. New investigations have been performed to develop cardiovascular health scores that integrate novel lifestyle habits for primordial prevention. The results obtained in our younger cohort of both sexes agree with those of previous studies that were limited to an elderly population25 or women.26
The Mediterranean diet score proposed by Trichopoulou et al.20 included alcohol intake. However, it was considered a separate lifestyle element because other studies have shown an independent effect of both moderate and excessive alcohol consumption on survival.13 In another analysis of this cohort,12 there was a positive and independent association between time spent watching television and all-cause mortality. A previous study found that participants who took a brief afternoon nap (< 30min/d) had lower risk of obesity (HR, 0.67; 95%CI, 0.46-0.96) than those who did not.11 Another of the factors included in this index was a BMI ≤ 22, due to previous findings that the incidence of metabolic risk factors increases above this threshold.27 Hu et al.28 determined that the most important risk factor for type 2 diabetes mellitus is a high BMI and even that a BMI from 23.0 to 24.9 was associated with higher risk of type 2 diabetes mellitus. In addition, in an exhaustive study recently published by the Global Burden of Disease group, with a sample size exceeding 68 million participants, an elevated BMI (from 22) was associated with death.29 Prospective studies have analyzed the protective effect of social relationships,14 whose biological mechanism might be based on inflammatory markers30 and could impact other healthy habits such as physical activity.31 The association between working hours and CVD is more controversial.32 Various socioeconomic factors have been proposed to explain the association between working hours and mortality. O’Reilly and Rosato15 found that professionals/managers who worked more than 40h/wk had lower risk of death than those who worked less time. Although these results appear to agree with those of recent work,33 other studies found higher risk of coronary heart disease and stroke in people who work more hours.34,35 Careful interpretation of these results is required due to the risk of bias from healthy workers. The socio-occupational homogeneity of the SUN cohort, together with the control for multiple confounding factors, reduces this possibility but does not eliminate it.
The difference between the separate effect of each of the indicators of healthy habits, only some of which are significant, and the combined effect of several factors is that the whole is probably more than the sum of its parts. In addition, similar results (with no significance for some individual elements but significance for the sum) have previously been published in the assessment of combination diet and cardiovascular risk scores20 or in the effect of various lifestyle factors on mortality.26
Unsurprisingly, adherence to various lifestyle habits that are beneficial individually would have a greater synergistic effect than a single habit in particular. The number of healthy habits should increase if individuals are concerned about maintaining ideal cardiovascular health or are encouraged to do so.36 Our findings stress this combined impact of various indicators of comprehensive healthy lifestyle habits. Even without consideration of classic variables key to cardiovascular epidemiology such as blood pressure, cholesterol, triglycerides, and glucose, a HLS is strongly associated with a reduced risk of primary CVD. This message is probably easier to convey to the general population and provides them with better control of their own health, that is, adequate training to improve their health (empowerment), and helps them to enjoy some much needed freedom from their laboratory values. All this allows us to advance beyond the clinical environment and expand the health promotion viewpoints according to the population strategy of cardiovascular prevention.5
Strengths and LimitationsThe present study has a number of important limitations. First, the variables used as the foundation for this score were self-reported and their reproducibility was not validated, except physical activity18 and BMI.17 There may be a classification bias if some of the participants overestimated or exaggerated their healthy habits. Nevertheless, if there were some degree of misclassification, it would be expected to be non-differential, which would make the bias more likely to tend to null. In addition, the lifestyle information was collected in the baseline questionnaire. Our analyses assumed that the habits remained stable throughout the study, but there may be some changes, which would probably lead to underestimation of the protective effects of a HLS.
Second, the cohort is restricted to university graduates, which limits the generalization of the results to the general population. Such extrapolation should be based on biological mechanisms and not on mere statistical “representativeness”.37 However, the restriction to university graduates reduces the possible confounding effects of educational level and also improves the quality of the information provided. This improves the internal validity of the study.
Third, the participants were young, mainly women, with a high educational level and few risk factors. Thus, as was expected, there were few cardiovascular events during follow-up. This might be associated with lower statistical power but the estimated power appears adequate (estimated power, 87%).
Despite adjustment by multiple confounding factors, there may still be some residual confounding.
On the other hand, the strengths of the present study include its prospective design with a prolonged follow-up period, a relatively large sample size, and high retention. In addition, validation studies were available for a considerable number of variables, the outcomes were confirmed using medical records, reducing the misclassification of endpoints, the models were adjusted by a large number of covariables to control for possible confounding, and the findings were found to be robust in sensitivity analyses.
CONCLUSIONSIn this cohort of university graduates, a HLS score constructed with 10 simple variables was associated with risk of primary CVD. These results indicate the importance of promoting a comprehensive HLS to maintain cardiovascular health and permit rapid patient evaluation in clinical practice. Further cohort and intervention studies are required to analyze populations at high cardiovascular risk and with participants from other socioeconomic and educational levels to confirm the results and extrapolate them to the general population.
FUNDINGThe SUN study has received funding from the Spanish Government-Instituto de Salud Carlos III and the European Regional Development Fund (RD 06/0045, CIBERObn, grants PI10/02658, PI10/02293, PI13/00615, PI14/01668, PI14/01798, PI14/1764, and G03/140), the Regional Government of Navarre (45/2011, 122/2014), and the University of Navarre.
CONFLICTS OF INTERESTNone declared.
- –
A HLS is key to achieving optimal cardiovascular health.
- –
Primordial prevention should be a priority to change behaviors determining the development of cardiovascular risk factors.
- –
Our study extends the healthy lifestyle pattern based on traditional habits to some novel factors, such as social relationships, alcohol consumption, work, television exposure, and an afternoon nap.
- –
The results show an inverse association between the HLS score and the risk of CVD.
- –
This simple lifestyle score will empower patients and give them a certain independence from laboratory values and greater control over their cardiovascular health beyond the clinical environment.
We would like to thank all of the participants for their involvement in the project and the members of the SUN study for their contribution.