Atrioventricular block (AVB) in the presence of bradycardic drugs (BD) can be reversible, and pacemaker implantation is controversial. Our objective was to analyze the pacemaker implantation rate in the mid-term, after BD suspension, and to identify predictive factors.
MethodsWe performed a cohort study that included patients attending the emergency department with high-grade AVB in the context of BD. We studied the persistence of AVB after BD discontinuation, recurrence in patients with AVB resolution, and the predictive variables associated with pacemaker requirement at 3 years.
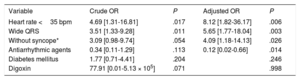
ResultsOf 127 patients included (age, 79 [71-83] years), BAV resolved in 60 (47.2%); among these patients, recurrence occurred during the 24-month median follow-up in 40 (66.6%). Pacemaker implantation was required in 107 patients (84.3%), despite BD discontinuation. On multivariable analysis, the variables associated with pacemaker need at 3 years were heart rate <35 bpm (OR, 8.12; 95%CI, 1.82-36.17), symptoms other than syncope (OR, 4.09; 95%CI, 1.18-14.13), and wide QRS (OR, 5.65; 95%CI, 1.77-18.04). Concomitant antiarrhythmic treatment was associated with AVB resolution (OR, 0.12; 95%CI, 0.02-0.66).
ConclusionsMore than 80% of patients with AVB secondary to BD require pacemaker implantation despite drug discontinuation. Predictive variables were wide QRS, heart rate <35 bpm, and clinical presentation other than syncope.
Keywords
Atrioventricular block (AVB) frequently develops in patients taking bradycardic drugs (BDs)1 such as beta-blockers, nondihydropyridine calcium antagonists, and digoxin.
BDs have classically been considered a reversible cause of AVB2–4 but it is difficult to determine if a patient's AVB is connected to these drugs per se or if there is an underlying conduction disorder. Moreover, few studies have analyzed the clinical course and prognosis of patients who develop AVB while taking BDs.1,5–8 According to European clinical practice guidelines,2 patients with reversible AVB, such as that caused by BDs, are not indicated for permanent pacemaker implantation (class III recommendation, level of evidence C). However, the new 2018 guidelines of the American College of Cardiology/American Heart Association (ACC/AHA)3 consider permanent pacemaker implantation to be “reasonable” in selected patients who have symptomatic second- or third-degree AVB and are undergoing medically necessary and stable antiarrhythmic or beta-blocker therapy, without the need for a washout period (class IIa recommendation, level of evidence B). Based on recent work,1,6,7 the guidelines additionally assert in the section on specific related recommendations that, although a BD overdose can cause reversible AVB, the therapeutic doses of these drugs do not generally cause AVB. Thus, controversy surrounds the management of high-grade AVB in patients receiving BD therapy.
The objective of this study was to analyze the need for pacemaker implantation in the short- and mid-term after BD discontinuation in a consecutive series of patients attending either of 2 emergency departments with symptomatic high-grade AVB in the presence of BDs. An additional aim was to identify the variables predicting pacemaker requirement in the short-term due to AVB persistence or during follow-up due to recurrence.
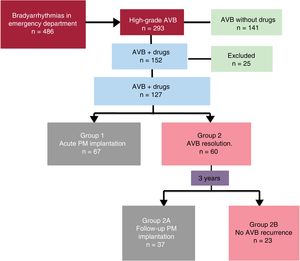
METHODSStudy populationThe present retrospective observational cohort study enrolled patients consecutively attending the emergency departments of 2 hospitals between January 2012 and December 2015. The study included all patients who, after their stay in the emergency department, were discharged with any of the following International Classification of Diseases, Ninth Revision, Clinical Modification codes: 426.0 (complete AVB), 426.1 (AVB and unspecified AVB), 426.6 (heart block), 426.9 (unspecified conduction disorder), 427.8 (other specified cardiac dysrhythmias), 427.9 (unspecified cardiac dysrhythmia), and 780.2 (syncope and collapse).9 Among the patients identified (figure 1), those who met the following criteria were selected:
- •
Diagnosis of third-degree AVB in sinus rhythm or second-degree Mobitz type II atrial fibrillation or 2:1 block.
- •
Of these, we selected patients receiving treatment with any of the following BDs: beta-blockers, nondihydropyridine calcium antagonists, or digoxin. Type Ic antiarrhythmics (according to the Vaughan-Williams classification) and amiodarone were considered concomitant medications and were also discontinued in the patients included in the present analysis.
- •
Patients with any of the following comorbidities were excluded: acute coronary syndrome, hyperkalemia ≥ 6.5 mEq/L, digoxinemia> 2 ng/mL, AVB secondary to radiofrequency ablation, and clinical impossibility of drug discontinuation.
The protocol was approved by the relevant ethics committee.
Patient flowThe sample was divided into 2 groups (figure 1) based on whether the bradyarrhythmia resolved after a 48-hour BD washout period. This length of time was chosen because it is similar to that used in other studies1 and because it exceeds the average half-lives of the BDs analyzed. Group 1 comprised patients with persistent AVB who underwent pacemaker implantation, whereas group 2 comprised patients with AVB resolution who were discharged from the emergency department without a pacemaker. In the latter group, analysis was performed of the rate of symptomatic AVB recurrence motivating a repeat visit to the emergency department after BD discontinuation during a 3-year follow-up; these patients were divided into group 2 A, who had recurrence and required pacemaker implantation, and group 2 B, who did not have recurrence.
Variables analyzedDemographic variables were recorded, as well as cardiovascular risk factors, the symptoms motivating emergency department attendance, previous heart diseases, electrolytes, renal function measured by serum creatinine, heart rate, the presence of wide QRS, and the use of BDs and antiarrhythmic drugs. For more practical assessment and treatment, the variable heart rate at admission was divided into ranges to identify the cutoff point providing the best discriminatory power.
Also recorded were pacemaker therapy during the first admission or after discharge and events during follow-up: 3-year mortality and emergency department attendance due to symptomatic bradyarrhythmia, syncope, and trauma as secondary endpoints.
Finally, as primary endpoint, the need for pacemaker implantation was studied at 3 years of follow-up. AVB electrocardiographically recorded in patients was considered to be recurrence (the secondary endpoint mortality was considered absence of recurrence, except when ECG-documented AVB was recorded as the cause of death).
Follow-upFollow-up was performed by 2 cardiologists using the same protocol for all patients in both centers. The data examined to establish if the patients had experienced any recurrence or event during follow-up were collected from the hospital medical records and health center and via centralized telephone calls. Although the follow-up was completed in all patients, a 3-year follow-up cutoff was applied in the univariable and multivariable analyses performed to identify the variables associated with pacemaker indication at 3 years and to homogenize follow-up durations. To analyze trauma during follow-up and mortality, another cutoff was established at 3 years: this cutoff point was chosen because it is the longest follow-up possible for the most recently enrolled patients (those from 2015).
Statistical analysisThe chi-square test was used for qualitative variables; continuous variables were analyzed with the Mann-Whitney U test and are expressed as median [25th and 75th percentiles]. P <.05 was considered statistically significant. A multivariable logistic regression analysis was performed to predict pacemaker requirement at 3 years. In this analysis, we included the variables associated with P <.20 with AVB persistence and recurrence in the univariable analysis, applying stepwise selection and removing from the model those variables with P> .05.
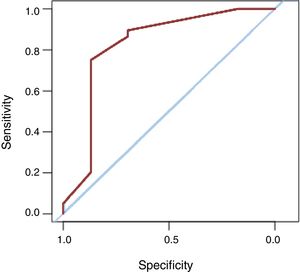
Next, the area under the receiver operating characteristic (ROC) curve of the logistic regression model was analyzed to predict pacemaker requirement at 3 years using only those variables significantly associated with pacemaker requirement at 3 years in the multivariable analysis. The sensitivity and specificity values of this model were determined by analyzing the different cutoff points and selecting the one offering the best results.
Data were analyzed using the R statistical package.
RESULTSThe patient flow diagram of the study can be seen in figure 1. Of the 152 patients who attended the emergency department with high-grade AVB while taking BDs, we studied 127 patients meeting the inclusion criteria. Thus, 25 patients were excluded (due to acute coronary syndrome [n=12], clinical impossibility of drug discontinuation [n=7], digoxinemia> 2 ng/mL [n=4], and hyperkalemia ≥ 6.5 mEq/L [n=2]).
Of the 127 patients finally included (age, 79 [71-83] years; 50.4% men), 52.8% (n=67) still had AVB after BD discontinuation (group 1); the remainder (n=60) recovered atrioventricular conduction and were discharged without pacemaker implantation (group 2). The mean follow-up duration was 24 months and 2 patients (1.5%) were lost to follow-up. During this period, 40 patients in group 2 (66.6%) had AVB recurrence and underwent pacemaker implantation; in 37 of these, the block recurred in the 3 years after emergency department discharge (group 2 A).
In the overall sample, 107 patients (84.36%) required acute pacemaker implantation or implantation during follow-up despite drug discontinuation; 104 required the pacemaker implantation at the 3-year follow-up (groups 1 and 2 A), whereas the AVB resolved and did not recur after drug discontinuation in only 23 (18.1%; group 2 B) (figure 1). The median time to AVB recurrence was 65 [12-201] days.
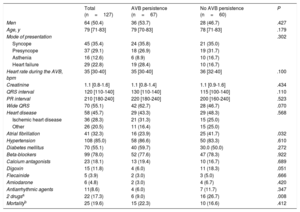
Baseline characteristics and univariable analysis: variables related to the need for acute pacemaker implantationAtrioventricular conduction recovery was more frequent in patients taking 2 negative chronotropic drugs (particularly digoxin) or with narrow QRS, a higher heart rate, or atrial fibrillation (table 1). Notably, all patients receiving treatment with 2 drugs had atrial fibrillation.
Patient characteristics according to persistence (group 1) or not (group 2) of AVB after emergency department attendance
| Total (n=127) | AVB persistence (n=67) | No AVB persistence (n=60) | P | |
|---|---|---|---|---|
| Men | 64 (50.4) | 36 (53.7) | 28 (46.7) | .427 |
| Age, y | 79 [71-83] | 79 [70-83] | 78 [71-83] | .179 |
| Mode of presentation | .302 | |||
| Syncope | 45 (35.4) | 24 (35.8) | 21 (35.0) | |
| Presyncope | 37 (29.1) | 18 (26.9) | 19 (31.7) | |
| Asthenia | 16 (12.6) | 6 (8.9) | 10 (16.7) | |
| Heart failure | 29 (22.8) | 19 (28.4) | 10 (16.7) | |
| Heart rate during the AVB, bpm | 35 [30-40] | 35 [30-40] | 36 [32-40] | .100 |
| Creatinine | 1.1 [0.8-1.6] | 1.1 [0.8-1.4] | 1.1 [0.9-1.6] | .434 |
| QRS interval | 120 [110-140] | 130 [110-140] | 115 [100-140] | .110 |
| PR interval | 210 [180-240] | 220 [180-240] | 200 [160-240] | .523 |
| Wide QRS | 70 (55.1) | 42 (62.7) | 28 (46.7) | .070 |
| Heart disease | 58 (45.7) | 29 (43.3) | 29 (48.3) | .568 |
| Ischemic heart disease | 36 (28.3) | 21 (31.3) | 15 (25.0) | |
| Other | 26 (20.5) | 11 (16.4) | 15 (25.0) | |
| Atrial fibrillation | 41 (32.3) | 16 (23.9) | 25 (41.7) | .032 |
| Hypertension | 108 (85.0) | 58 (86.6) | 50 (83.3) | .610 |
| Diabetes mellitus | 70 (55.1) | 40 (59.7) | 30.0 (50.0) | .272 |
| Beta-blockers | 99 (78.0) | 52 (77.6) | 47 (78.3) | .922 |
| Calcium antagonists | 23 (18.1) | 13 (19.4) | 10 (16.7) | .689 |
| Digoxin | 15 (11.8) | 4 (6.0) | 11 (18.3) | .051 |
| Flecainide | 5 (3.9) | 2 (3.0) | 3 (5.0) | .666 |
| Amiodarone | 6 (4.8) | 2 (3.0) | 4 (6.7) | .420 |
| Antiarrhythmic agents | 11(8.6) | 4 (6.0) | 7 (11.7) | .347 |
| 2 drugsa | 22 (17.3) | 6 (9.0) | 16 (26.7) | .008 |
| Mortalityb | 25 (19.6) | 15 (22.3) | 10 (16.6) | .412 |
AVB, atrioventricular block.
Data are expressed as No. (%) or as median [interquartile range]
There were no significant differences in 3-year mortality between groups 1 and 2 (table 1).
Of the 40 patients with AVB recurrence, 16 (40%) had syncope, 8 (20%) had presyncope, and 16 (40%) had asthenia and effort intolerance.
There was a tendency for a higher incidence of trauma requiring emergency department treatment at 3 years of follow-up in group 2 than in group 1 (13.3% [n=8] vs 4.4% [n=3]; P=.11). During the complete follow-up, group 1 patients had 2 traumatic brain injuries and 1 had hip fracture. Group 2 patients had 7 traumatic brain injuries and 2 had rib fractures.
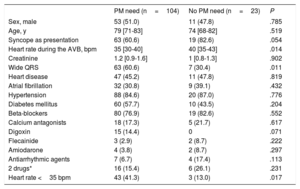
Comparison of groups 1 and 2 A with group 2 B. Variables associated with the mid-term need for pacemaker implantationThe 23 patients whose AVB had not recurred 3 years after BD discontinuation (table 2) had a higher heart rate in the emergency department, as well as a higher prevalence of narrow QRS, clinical presentation as syncope or presyncope (vs asthenia or heart failure), and concomitant antiarrhythmic treatment. Although few patients were receiving treatment with digoxin, the need for pacemaker implantation was particularly high in this group.
Patient characteristics according to need for pacemaker implantation
| PM need (n=104) | No PM need (n=23) | P | |
|---|---|---|---|
| Sex, male | 53 (51.0) | 11 (47.8) | .785 |
| Age, y | 79 [71-83] | 74 [68-82] | .519 |
| Syncope as presentation | 63 (60.6) | 19 (82.6) | .054 |
| Heart rate during the AVB, bpm | 35 [30-40] | 40 [35-43] | .014 |
| Creatinine | 1.2 [0.9-1.6] | 1 [0.8-1.3] | .902 |
| Wide QRS | 63 (60.6) | 7 (30.4) | .011 |
| Heart disease | 47 (45.2) | 11 (47.8) | .819 |
| Atrial fibrillation | 32 (30.8) | 9 (39.1) | .432 |
| Hypertension | 88 (84.6) | 20 (87.0) | .776 |
| Diabetes mellitus | 60 (57.7) | 10 (43.5) | .204 |
| Beta-blockers | 80 (76.9) | 19 (82.6) | .552 |
| Calcium antagonists | 18 (17.3) | 5 (21.7) | .617 |
| Digoxin | 15 (14.4) | 0 | .071 |
| Flecainide | 3 (2.9) | 2 (8.7) | .222 |
| Amiodarone | 4 (3.8) | 2 (8.7) | .297 |
| Antiarrhythmic agents | 7 (6.7) | 4 (17.4) | .113 |
| 2 drugs* | 16 (15.4) | 6 (26.1) | .231 |
| Heart rate <35 bpm | 43 (41.3) | 3 (13.0) | .017 |
AVB, atrioventricular block; PM, pacemaker.
Data are expressed as No. (%) or median [interquartile range].
Multivariable analysis with multiple logistic regression (table 3) showed that pacemaker need due to irreversible AVB or AVB recurrence at the 3-year follow-up was significantly associated with the following: heart rate <35 bpm (odds ratio [OR]=8.12; 95% confidence interval [95%CI], 1.82-36.17; P=.006), wide QRS on ECG (OR=5.65; 95%CI, 1.77-18.04; P=.003), and a clinical presentation other than syncope or presyncope (OR=4.09; 95%CI, 1.18-14.13; P=.026). Concomitant antiarrhythmic treatment was a protective factor (OR=0.12; 95%CI, 0.02-0.66; P=.014). This model had an area under the ROC curve discrimination of 0.82 (0.71-0.94) (figure 2) to identify patients requiring a pacemaker at 3 years of follow-up despite BD discontinuation. A probability value of 0.85 with 75% sensitivity and 87% sensitivity was chosen because it provided the best discriminatory power.
Factors associated with AVB persistence or recurrence at 3 years
| Variable | Crude OR | P | Adjusted OR | P |
|---|---|---|---|---|
| Heart rate <35 bpm | 4.69 [1.31-16.81] | .017 | 8.12 [1.82-36.17] | .006 |
| Wide QRS | 3.51 [1.33-9.28] | .011 | 5.65 [1.77-18.04] | .003 |
| Without syncope* | 3.09 [0.98-9.74] | .054 | 4.09 [1.18-14.13] | .026 |
| Antiarrhythmic agents | 0.34 [0.11-1.29] | .113 | 0.12 [0.02-0.66] | .014 |
| Diabetes mellitus | 1.77 [0.71-4.41] | .204 | .246 | |
| Digoxin | 77.91 [0.01-5.13 × 105] | .071 | .998 |
AVB, atrioventricular block; OR, odds ratio.
Our results show that almost 85% of patients who attend an emergency department with AVB while taking BDs ultimately require permanent pacemaker implantation. These data are in line with those published previously,1,5–8 but our work involves a series of patients from 2 centers and a larger sample size, enabling more robust analysis. In addition, 4 independent variables were identified that could help to predict patients who will eventually require a permanent pacemaker or, in contrast, to identify patients, fewer than 20%, who will not require a pacemaker in the mid-term.
The ramifications of these results are substantial because they indicate the need to consider a change to the clinical practice. First, according to our findings and those of other studies,1,5–8 AVB is rarely attributable to BDs alone. Rather, the results seem to indicate that these drugs reveal a latent conduction disorder. In addition, the delay to pacemaker implantation, imposed to determine whether the block resolves with drug discontinuation, can have deleterious consequences for patients due to reduced cardiac output or the need for a temporary pacemaker, with the associated comorbidities,6 as well as for the health care system due to a prolonged hospital stay, particularly that in the emergency department or coronary care unit.
In the mid-term, the clinical recurrence of AVB can have severe repercussions for patients, such as syncope, trauma, and fractures. These are particularly impactful in vulnerable elderly patients,10 who are more susceptible to developing bradycardia secondary to BD therapy.11
Although BD use is a relatively frequent finding in the presence of symptomatic AVB, few studies have analyzed its clinical course.1,6 Those results, similar to those published by other authors, such as Zeltser et al.,1 indicate a recurrence rate close to 50%. In an interesting study, Knudsen et al.6 analyzed patients under treatment with BDs who required temporary pacemaker implantation due to AVB: about 90% ultimately required a permanent pacemaker, with a nonnegligible complication rate. In this context, some authors have proposed pacemaker implantation independently of BD use.12 Notable considerations include the waste of resources due to the need for patient monitoring while the BD is eliminated, as well as the risk of a clinical deterioration in these patients while they await definitive treatment. In addition, the risk of syncope or sudden cardiac death is negligible in patients who have been discharged after restoration of atrioventricular conduction. In contrast, it should not be forgotten that pacemaker implantation is still an invasive procedure, one that is not complication-free. Accordingly, it is essential to identify those patients who will benefit from the device. A specially designed comparative study is required to investigate the prognosis of early pacemaker implantation in patients who recover from pharmacological AVB vs a conservative strategy.
The innovative aspect of the present work is that it identifies variables that help to predict those patients attending an emergency department with BD-associated AVB who will eventually require a definitive pacemaker. These variables, which can be obtained in the first bedside evaluation, predict the clinical course and reduce possible complications due to a delay to the permanent treatment. They also indicate patient groups with different behaviors who should be the focus of future studies for further knowledge advances. Notably, although the need for pacemaker implantation (acute or during follow-up) was high in all groups, a pacemaker was ultimately required by 90% of patients with wide QRS and a very low heart rate (< 35 bpm) or with a clinical presentation other than syncope. In addition, patients under treatment with groups Ic and II antiarrhythmic agents13 (flecainide, propafenone, and amiodarone) in combination with BDs appear to have fewer intrinsic conduction disorders and to recover normal conduction without the need for pacemakers. This could be explained by the effect of these drugs on the His-Purkinje system and on cell refractoriness.14–17 For their part, beta-blockers, nondihydropyridine calcium antagonists, and digoxin are characterized by their stronger negative chronotropic effects due to their direct action on the sinoatrial and atrioventricular nodes and lack of action on intra-Hisian and infra-Hisian conduction.18–22 This finding reinforces the belief that His-Purkinje involvement and its correct identification are crucial for clinical decision making. Indeed, the electrocardiographic variables independently associated with the eventual need for pacemaker implantation (wide QRS and heart rate <35 bpm) indicate an infra-Hisian location of the AVB. This location should not be affected by beta-blockers, calcium antagonists, or digoxin, which would reinforce the hypothesis of an underlying conduction disorder with a high risk of recurrence even without BDs. Although few patients were being treated with digoxin (n=15), their recurrence rate was very high, which is why it should be taken into account, despite not being included in the logistic regression model.
Another interesting finding is that patients with more latent symptoms, such as asthenia and heart failure, seem to more frequently have a more permanent conduction system disorder than those who initially have syncope or presyncope, whose bradyarrhythmia is more likely to resolve without recurrence. A possible explanation for this finding could be that, while a sudden clinical presentation such as syncope may be related to paroxysmal AVB, heart failure or asthenia could be related to persistent AVB that has become established during a sufficiently prolonged period to lead to more durable symptoms. Regarding the literature, our data fail to confirm the findings of Osmonov et al.,7 which indicated that a history of heart failure could protect against pacemaker need.
LimitationsThe present article has some limitations. First, because the data were retrospectively collected, the variables analyzed were those described in the medical records. Thus, there may be other variables that more accurately predict recurrence. However, this characteristic does not invalidate the findings reported in the present work, which also offer excellent predictive capacity. Moreover, our prospective analysis of the diagnostic classification of the enrolled patients minimized the possibility of missing patients who should have been included in the study.
This study did not exclude patients taking group I and III antiarrhythmic agents, as done in similar studies, although we only included patients taking beta-blockers, nondihydropyridine calcium antagonists, or digoxin. These drugs have a more marked effect on the His-Purkinje system and may have a clearer relationship with AVB development, as shown by our results.
Finally, the small number of patients with antiarrhythmic therapy in the present study limited our ability to draw definitive conclusions, although the results nonetheless show that these drugs may have different implications and should be analyzed in future studies with larger sample sizes. Other drugs such as ivabradine were not included in the analysis because their main effect is on the sinoatrial node; some authors23,24 have already published an effect, albeit minor, of ivabradine on the atrioventricular node.
CONCLUSIONSIn most patients with AVB taking BDs, the bradyarrhythmia persists or recurs after drug discontinuation, indicating the presence of an intrinsic conduction disorder. In the mid-term, more than 80% of such patients require pacemaker implantation. Predictive variables can help to identify patients who will require a pacemaker, without the need to wait for new recurrences and avoiding the associated complications.
FUNDINGNo funding has been received to support this study.
CONFLICTS OF INTERESTNone to declare.
- –
AVB in patients taking BDs is a frequent clinical challenge with controversial management.
- –
Few studies have analyzed the clinical course and prognosis of these patients but the current literature indicates a high rate of AVB recurrence, despite drug discontinuation.
- –
The present study provides data on the largest patient sample to date with the longest follow-up period.
- –
A high rate of pacemaker implantation was found, both acute and during follow-up, and several predictive variables were identified.
- –
Also analyzed were the rates of syncope and injuries associated with AVB recurrence, which are elevated, particularly considering their clinical impact in elderly patients.
- –
The high discriminatory power of the predictive model, based on clinical and electrocardiographic characteristics, facilitates the early identification of patients with AVB taking BDs who will ultimately require a permanent pacemaker.