Cardiovascular diseases (CVDs) are a heterogeneous group of clinical entities with atherosclerosis as the common etiopathogenic substrate. Together, they are the cause of death in most Europeans.1
In an article recently published in Revista Española de Cardiología, Cayuela et al.2 examined the changes over time in mortality from these conditions in the last 2 decades. The answers provided by their data are distinct, and even sometimes completely opposing, for each component cardiovascular cause. Although the age-standardized rates have decreased for most causes of death, the absolute numbers of deaths have increased for some causes.
This result undoubtedly reflects the heterogeneity of CVDs. The most alarming data concern the increase in deaths from “other heart diseases” and, to a lesser extent—because the number of deaths is much lower—from the entity “hypertensive diseases”. The conditions causing the most deaths are coronary heart disease (CHD) in men and stroke in women. The absolute numbers of both entities have decreased, as well as their standardized rates at all ages and their truncated rates for ages 35 to 64 years.
Although CHD and stroke share some risk factors, the attributable risk of each factor differs in each disease (smoking, cholesterol, diabetes, hypertension, and male sex in the first condition and largely hypertension in the second). Good control of all risk factors in secondary prevention reduces the recurrence of all types of CVD. We shall focus on CHD.
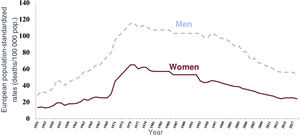
WHICH OF OUR ACTIONS HAVE REDUCED CORONARY MORTALITY?If we widen the window concerning trends in mortality from CHD in Spain to the 1950s (figure 1), we can clearly see that the downward trend that began in the 1970s began to flatten several decades ago.
Age-standardized mortality from coronary heart disease in Spain between 1950 and 2018 by sex. Adapted from the Spanish National Statistics Institute.12.
A reduction in the absolute number of deaths from CHD in a region typically involves 2 concurrent conditions: about half is due to a fall in incidence while the rest is due to a fall in acute deaths among those who develop the condition, according to IMPACT models.3,4
The incidence decrease is dependent both on primary prevention involving the systematic application of coronary risk functions to patient screening and the activation of the corresponding preventive measures5 and on public health-supported population-wide strategies involving health promotion interventions. The second condition relies on the creation of urgent care networks for acute processes (infarction and stroke codes)6 for applying therapeutic advances to patients showing symptoms indicative of CVD.7 The complex interaction of the factors influencing the number and survival of patients with CHD hinders a sufficiently clear determination of the causes of the decrease in CHD-related mortality based on a simple examination of mortality registry data.8
MORTALITY DATA QUALITYAs stressed by Cayuela et al.,2 mortality data are easy to obtain and have been collected for centuries in some countries. However, the robustness of a conclusion is never stronger than the quality of the supporting data. Cayuela et al. focus exclusively on 2 decades, a period in which identification of inflection points is difficult based on a simple visualization of the secular trends shown in figure 1. Inflection points have various causes: a) changes in the international classification of diseases; b) changes in the interest of certifying physicians in CVDs; c) improved life expectancy9; d) changes in diagnostic criteria; e) therapeutic advances6,7; and f) implementation of increasingly effective primary and secondary prevention measures.3,4 In addition, countries exhibit considerable variations in death certification.10
One factor confounding the comparisons and trends is poorly defined causes of death, such as essential hypertension (I10), cardiac arrest (I46), heart failure (I50), and atherosclerosis (I70), as well as the deaths coded as R00 to R09 (abnormalities of heart beat) and R96 to R99 (sudden death), which should not be used to certify death according to the World Health Organization (WHO).10,11 According to our calculations,12 these codes corresponded to 15% of all death diagnoses in Spain in 2018.12 This indicates only moderate certification quality (they represent < 5% in the United Kingdom and Finland).8 Of course, analysis of the trends in these causes of death raises questions about their interpretation. In addition, the WHO advises consideration of the redistribution and weighting of poorly defined causes of death before death rates are reported and compared among countries.8
Moreover, the WHO recommends that the code for dementia be used as the main diagnosis even when there are other concurrent causes of death, including CVD.10 This approach additionally compromises the identification of CHD as the main cause of death.
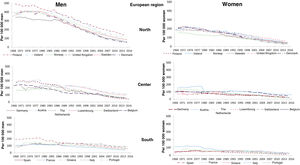
Some more light is shed through international comparisons facilitated by the use of the CHD mortality data compiled and standardized by the WHO since the 1970s. Figure 2 shows the trends in the last 50 years in standardized mortality from myocardial infarction in the population aged 0 to 64 years by sex in 3 country groups (Northern, Central, and Southern Europe).1 The higher the initial CHD mortality rate, the steeper the decrease, until recently. Moreover, all countries have achieved similar mortality rates in the present decade (about 100/100 000 for men and 50/100 000 for women). The slope is very gradual in southern countries and is more akin to a stabilization than a decrease in recent decades. The conclusions obtained from these figures is that, independently of the factors confounding international comparisons, all countries analyzed have converged on a structural inherent mortality rate from coronary disease that will be resistant to further decreases until atherosclerosis can be prevented and cured.
Trends in standardized coronary heart disease mortality rates in various Northern, Central, and Southern European countries between 1968 and 2018 by sex. Adapted from the Spanish National Statistics Institute.12
Unfortunately, using mortality data from 2 decades, we cannot confirm the highly interesting hypothesis concerning the competing causes of death or the possible progressive restriction of coronary morbidity and mortality to ever older ages due to the reduced lethality of CHD.13 It is difficult to verify these phenomena, which are plausible from the epidemiological perspective, for various reasons. These include lower certification quality at advanced ages, the prioritization of diagnoses such as dementia over CHD,8,10 and the chronification of many cases that would have once been fatal, with the patients ultimately dying from competing causes that would be impossible to identify in mortality registries.
SCARCE DATA ON MYOCARDIAL INFARCTION INCIDENCEGiven the above, there is an evident need to obtain incidence, lethality, and mortality data in randomized representative population samples with sufficient statistical power to adequately answer the questions posed.10,14 In particular, these questions include competing causes of death in patients with chronic CHD, which can be perfectly quantified in a population-based cohort study. It is highly likely that the primary and secondary prevention measures have led to various phenomena when the CHD of 30 or 40 years ago is compared with that of the present day: first, the delayed onset of the first symptoms of CHD; second, the reduced severity/lethality of new cases; and finally, the delayed death of patients with chronic CHD, which is additionally masked by competing causes of death.
The data available in Europe, including the Girona region, indicate that the incidence of CHD has fallen from 1985 to 2010 at close to 4.2% per year in men and 4.0% in women aged 35 to 74 years.14 The decreases in 28-day lethality (the percentage of deaths in those who have the disease) are also marked: 2.0% and 2.4% per year, respectively.14 This reduced lethality from CHD is very well-explained by the contribution of the treatment of acute CHD to the reduction in population mortality, already seen in in-hospital mortality.7
This observation represents a health care success that is partly attributable to the efforts of primary prevention, which avoids some of the new cases, to the improved treatment of potentially fatal cases, and to the efforts of secondary prevention, which minimizes CHD recurrence. The findings support the mortality reductions detected by Cayuela et al.2
CONCERN ABOUT LIMITED DATA ON CEREBROVASCULAR DISEASEAs in most CVDs, the downward trend in cerebrovascular disease mortality has been stabilizing in Europe in recent decades. However, few data are available on the trends in cerebrovascular diseases, as well as their lethality and mortality in Spain. Cayuela et al.2 neatly describe how the standardized cerebrovascular disease mortality rates for all ages and those truncated at ages 35 to 64 years have been decelerating in men in Spain but stabilizing in women, particularly from 2014 onward.
In recent decades, this decline in both the morbidity and mortality of cerebrovascular diseases has been attributed to various factors related to the improved treatment of these patients and the general population. In primary prevention, the use has increased of antihypertensives and combination therapies, particularly in patients considered at high risk. Disease understanding has also improved, as well as the control of the main cardiovascular risk factors and the health-promoting activities of public health. During the acute phase, the implementation of stroke units and the infarction code in various Spanish cities and the introduction of thrombolytic treatment have helped to decrease its lethality and the associated complications in these patients. In secondary prevention, the use of antiplatelet agents and anticoagulants, together with other therapeutic options, has contributed to reductions in the recurrence and mortality of cerebrovascular disease.
Of the cerebrovascular diseases, coded as I60 to I69,11 each subtype has a distinct pathophysiology and exhibits partial differences in the importance of each risk factor. Hemorrhagic stroke is the cerebrovascular disease with the highest mortality. Its main risk factor is hypertension and, as well observed by Cayuela et al., hypertensive diseases and their mortality have increased in recent years.2 Accordingly, the changes over time in blood pressure values must be assessed in population studies because we can alter the trends in mortality from cerebrovascular disease seen thus far.
AND WHAT NEXT?These improvements in mortality and incidence must not distract us from our objectives: CHD and stroke are the leading individual causes of death in Europe and in the rest of the planet. They are also the main cause of quality-adjusted life years lost, which reflects their major impact on the quality of life of survivors.15
Finally, we still have some way to go before sufficiently understanding the causes and trends in atherosclerosis: we do not know why some patients develop atherosclerotic plaques (there are no known sufficient or necessary causes) nor which of those patients who already have them will experience the instability of at least one plaque that triggers an acute coronary event.16 The coming years will see extensive research into the immune phenotype, into the multiomic characterization of the epigenome, transcriptome, metabolome, and microbiome, and into the study of the epigenetic influence of social factors on the resistance to or accelerated onset of atherosclerosis and its manifestations.17
Thus, CVD is still far from being beaten and clinical and basic research must be focused on clarifying the mechanisms and triggers of atherosclerotic plaques and the causes of their stabilization and destabilization. This research will enable us to focus on the elements required to cure atherosclerosis, with the team responsible probably deserving a Nobel Prize.
FUNDINGThis work received funding from: CIBERCV; CIBERESP; European Regional Development Funds (ERDF); FIS-14/00449, FIS-PI18/00030, FIS-INTRASALUD-PI1101801; Agència de Gestió d’Ajuts Universitaris de Recerca (AGAUR) de Catalunya, 2017SGR222, and Sociedad Española de Cardiología, Proyectos de Investigación Clínica 2019 (13224).
CONFLICTS OF INTERESTNone of the authors declare any conflict of interest.