Mortality is high in acute aortic syndrome (AAS), which therefore requires early treatment. This study aimed to analyze changes in the diagnosis and treatment of AAS over 20 years at our center.
MethodsFrom 1999 to 2018, 451 patients diagnosed with AAS (336 men; mean age, 60.9±12.4 years) were prospectively included (270 type A and 181 type B). Clinical variables, diagnosis, treatment, and in-hospital complications were analyzed.
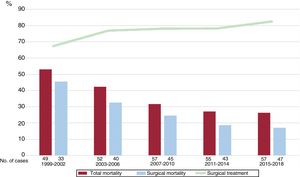
ResultsThe use of computed tomography (CT) as the first-line diagnostic technique increased from 62.8% to 94.2% (P <.001). Surgical treatment of type A AAS rose from 67.4% to 82.5% (P=.09). Mortality from type A AAS decreased significantly from 53.1% to 26.3% (P <.001) as a result of the fall in mortality from surgical treatment (from 45.4% to 17.0%; P <.001). The use of medical treatment alone for type B AAS decreased from 91.8% to 61.7% (P <.001) due to the greater use of endovascular treatment. Mortality from type B AAS showed no significant reduction (16.2% to 10.6%; P=.15).
ConclusionsThe diagnosis and treatment of AAS has changed substantially in the last 2 decades. CT has become the first-line diagnostic technique for AAS. In type A AAS, mortality has fallen significantly due to improvements in the results of surgical treatment. In type B AAS, the use of medical treatment alone has decreased due to the expansion of endovascular treatment, although in-hospital mortality has not decreased significantly.
Keywords
Acute aortic syndrome (AAS), one of the most serious cardiovascular emergencies, requires rapid diagnosis and treatment, with early work showing a 1% increase in mortality for each hourly delay in the appropriate therapy.1
Considerable progress has been made in the diagnosis of this entity in recent decades due to increased clinical suspicion and the use of imaging techniques.2,3
In addition, the improved management of this condition has been made possible by new therapeutic strategies in ascending aorta surgery,4 as well as the introduction and development of endovascular treatment.5–7 Moreover, better understanding of the diagnosis, management, and prognosis of AAS has been obtained from the publication of numerous multicenter registries.8–10 Nonetheless, these studies included centers with different levels of experience.11 Although the information obtained is useful, it is difficult to determine the actual changes in mortality and therapeutic management in recent decades.12 Most studies have reported results from single centers equipped with expert surgical teams whose patients were mainly referred from other centers, with a time from onset exceeding 24 to 48hours, which would not reflect the actual outcomes of AAS treatment over time.13 Little information is therefore available on the impact of the changes in the diagnostic and therapeutic management of this disease in recent decades. The purpose of the present study was therefore to analyze changes in the management and treatment of AAS in the last 20 years in a single center.
METHODSThis study prospectively included 451 consecutive patients diagnosed with AAS in our center from January 1, 1999, to December 31, 2018. The ascending aorta was affected in 270 of the patients (type A AAS), whereas only the descending aorta or aortic arch was affected in 181 patients. The patients were identified in the emergency department, imaging department, or other departments involved in the patients’ hospitalization. Diagnosis was based on clinical data, imaging results, surgical findings, and postmortem examination. The study outcomes were analyzed separately by considering five 4-year intervals over the 20-year study period. We analyzed demographic variables, cardiovascular risk factors, history of vascular disease, diagnostic techniques used, treatment applied, and in-hospital mortality. Patients previously diagnosed with ischemic heart disease, artery disease, or stroke were considered to have a history of atherosclerosis. Shock was defined as systolic blood pressure <80mmHg while impaired renal function was defined as creatinine > 1.5mg/100mL or estimated glomerular filtration <50mL/min/1.73 m2. We did not include patients with a history of AAS or whose AAS was traumatic or iatrogenic in nature.
Statistical analysisData were analyzed using Stata version 13.1 statistical package. Quantitative variables are expressed as mean±standard deviation and qualitative variables as percentage. Quantitative variables were compared between groups using the t test, whereas the chi-square test was used to compare qualitative variables. P <.05 was considered significant.
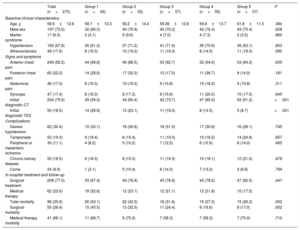
RESULTSOf the 451 patients with AAS, 336 were men (74.5%) and 115 were women (25.5%); the overall mean age was 60.9±12.4 (range, 28-89) years. Demographic data and the cardiovascular disease history of patients with type A AAS are detailed in table 1, whereas those of patients with type B AAS are shown in table 2. Patients with type B AAS were older than those with type A AAS (63.0±11.4 vs 59.5±12.6 years; P <.001). Hypertension was highly prevalent in both type A and type B patients (67.8% vs 76.8%; P <.01). There were no significant changes in patient characteristics among the different 4-year intervals of the study. In addition, no differences were found in exploratory signs and symptoms or in electrocardiographic or chest radiography abnormalities. The use of computed tomography (CT) as the first-line diagnostic technique for AAS (types A and B) increased from 62.8% to 94.2% between the first and last intervals studied (P <.001). In contrast, the use of transesophageal echocardiography (TEE) as a diagnostic technique decreased from 32.5% to 5.7%. A minority of patients were diagnosed using transthoracic echocardiography (TTE) or magnetic resonance imaging alone.
Demographic data, clinical presentation, diagnosis, treatment, and complications in patients with type A AAS
| Total (n=270) | Group 1 (n=49) | Group 2 (n=52) | Group 3 (n=57) | Group 4 (n=55) | Group 5 (n=57) | P | |
|---|---|---|---|---|---|---|---|
| Baseline clinical characteristics | |||||||
| Age, y | 59.5±12.6 | 58.7±12.3 | 58.2±14.4 | 59.36±12.8 | 59.8±13.7 | 61.6±11.5 | .384 |
| Male sex | 197 (73.0) | 32 (65.3) | 40 (76.9) | 40 (70.2) | 42 (76.4) | 43 (75.4) | .628 |
| Marfan syndrome | 17 (6.3) | 2 (4.1) | 5 (9.6) | 4 (7.0) | 4 (7.3) | 2 (3.5) | .860 |
| Hypertension | 183 (67.8) | 30 (61.2) | 37 (71.2) | 41 (71.9) | 39 (70.9) | 36 (63.1) | .603 |
| Atherosclerosis | 48 (17.8) | 8 (16.3) | 10 (19.2) | 11 (19.3) | 8 (14.5) | 11 (19.3) | .090 |
| Signs and symptoms | |||||||
| Anterior chest pain | 249 (92.2) | 44 (89.8) | 46 (88.5) | 53 (92.7) | 52 (94.5) | 54 (94.3) | .635 |
| Posterior chest pain | 60 (22.2) | 14 (28.6) | 17 (32.3) | 10 (17.5) | 11 (36.7) | 8 (14.0) | .181 |
| Abdominal pain | 46 (17.0) | 8 (16.3) | 10 (19.2) | 9 (15.8) | 10 (18.2) | 9 (15.8) | .311 |
| Syncope | 47 (17.4) | 8 (16.3) | 9 (17.3) | 9 (15.6) | 11 (20.0) | 10 (17.5) | .645 |
| Initial diagnostic CT | 204 (75.6) | 29 (59.2) | 34 (65.4) | 42 (73.7) | 47 (85.5) | 52 (91.2) | <.001 |
| Initial diagnostic TEE | 50 (18.5) | 14 (28.9) | 12 (23.1) | 11 (19.3) | 8 (14.5) | 5 (8.7) | <.001 |
| Complications | |||||||
| Severe hypotension | 82 (30.4) | 15 (30.1) | 16 (30.8) | 18 (31.5) | 17 (30.9) | 16 (28.1) | .745 |
| Tamponade | 52 (19.3) | 9 (18.4) | 8 (15.4) | 11 (19.3) | 10 (18.2) | 14 (24.6) | .657 |
| Peripheral or mesenteric ischemia | 30 (11.1) | 4 (8.2) | 5 (10.2) | 7 (12.2) | 6 (10.9) | 8 (14.0) | .465 |
| Chronic kidney disease | 50 (18.5) | 9 (18.3) | 8 (15.3) | 11 (19.3) | 10 (18.1) | 12 (21.0) | .478 |
| Coma | 24 (8.9) | 1 (2.1) | 5 (10.4) | 8 (14.0) | 7 (13.2) | 3 (6.8) | .794 |
| In-hospital treatment and follow-up | |||||||
| Surgical treatment | 208 (77.0) | 33 (67.4) | 40 (76.9) | 45 (78.9) | 43 (78.2) | 47 (82.5) | .447 |
| Medical therapy | 62 (23.0) | 16 (32.6) | 12 (23.1) | 12 (21.1) | 12 (21.8) | 10 (17.5) | |
| Total mortality | 96 (35.6) | 26 (53.1) | 22 (42.3) | 18 (31.6) | 15 (27.3) | 15 (26.3) | .002 |
| Surgical mortality | 55 (26.4) | 15 (45.5) | 13 (32.5) | 11 (24.4) | 8 (18.6) | 8 (17.0) | .002 |
| Medical therapy mortality | 41 (66.1) | 11 (68.7) | 9 (75.0) | 7 (58.3) | 7 (58.3) | 7 (70.0) | .710 |
AAS, acute aortic syndrome; CT, computed tomography; TEE, transesophageal echocardiography.
Values represent No. (%) or mean±standard deviation.
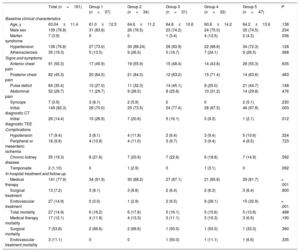
Demographic data, clinical presentation, diagnosis, complications, treatment, and changes in patients with type B AAS
| Total (n=181) | Group 1 (n=37) | Group 2 (n=34) | Group 3 (n=31) | Group 4 (n=32) | Group 5 (n=47) | P | |
|---|---|---|---|---|---|---|---|
| Baseline clinical characteristics | |||||||
| Age, y | 63.04±11.4 | 61.0±12.5 | 64.6±11.2 | 64.8±10.6 | 60.6±14.2 | 64.2±13.6 | .138 |
| Male sex | 139 (76.8) | 31 (83.8) | 26 (76.5) | 23 (74.2) | 24 (75.0) | 35 (74.5) | .234 |
| Marfan syndrome | 7 (3.9) | 0 | 0 | 1 (3.4) | 4 (12.5) | 2 (4.3) | .036 |
| Hypertension | 139 (76.8) | 27 (73.0) | 30 (88.24) | 26 (83.9) | 22 (68.8) | 34 (72.3) | .128 |
| Atherosclerosis | 35 (19.3) | 5 (13.5) | 9 (26.5) | 5 (16.7) | 7 (24.1) | 9 (26.5) | .568 |
| Signs and symptoms | |||||||
| Anterior chest pain | 91 (50.3) | 17 (45.9) | 19 (55.9) | 15 (48.4) | 14 (43.8) | 26 (55.3) | .635 |
| Posterior chest pain | 82 (45.3) | 20 (64.5) | 21 (84.0) | 12 (63.2) | 15 (71.4) | 14 (63.6) | .463 |
| Pulse deficit | 64 (35.4) | 10 (27.0) | 11 (32.3) | 14 (45.1) | 8 (25.0) | 21 (44.7) | .148 |
| Abdominal pain | 52 (28.7) | 11 (29.7) | 9 (26.5) | 8 (25.8) | 10 (31.2) | 14 (29.8) | .476 |
| Syncope | 7 (3.9) | 3 (8.1) | 2 (5.9) | 0 | 0 | 2 (5.1) | .230 |
| Initial diagnostic CT | 149 (82.3) | 26 (70.0) | 25 (73.5) | 24 (77.4) | 28 (87.5) | 46 (97.8) | .003 |
| Initial diagnostic TEE | 26 (14.4) | 10 (26.9) | 7 (20.6) | 5 (16.1) | 3 (9.3) | 1 (2.1) | .012 |
| Complications | |||||||
| Hypotension | 17 (9.4) | 3 (8.1) | 4 (11.8) | 2 (6.4) | 3 (9.4) | 5 (10.6) | .324 |
| Peripheral or mesenteric ischemia | 18 (9.9) | 4 (10.8) | 4 (11.0) | 3 (9.7) | 3 (9.4) | 4 (8.5) | .723 |
| Chronic kidney disease | 35 (19.3) | 8 (21.6) | 7 (20.6) | 7 (22.6) | 6 (18.8) | 7 (14.9) | .592 |
| Tamponade | 2 (1.10) | 0 | 1 (2.9) | 0 | 1 (3.1) | 0 | .092 |
| In-hospital treatment and follow-up | |||||||
| Medical therapy | 141 (77.9) | 34 (91.9) | 30 (88.2) | 27 (87.1) | 21 (65.6) | 29 (61.7) | < .001 |
| Surgical treatment | 13 (7.2) | 3 (8.1) | 3 (8.8) | 2 (6.4) | 2 (6.3) | 3 (6.4) | .800 |
| Endovascular treatment | 27 (14.9) | 0 (0.0) | 1 (2.9) | 2 (6.5) | 9 (28.1) | 15 (32.9) | < .001 |
| Total mortality | 27 (14.9) | 6 (16.2) | 6 (17.6) | 5 (16.1) | 5 (15.6) | 5 (10.6) | .488 |
| Medical therapy mortality | 17 (12.1) | 4 (11.8) | 4 (13.3) | 3 (11.1) | 3 (10.3) | 3 (6.9) | .190 |
| Surgical mortality | 7 (53.8) | 2 (66.6) | 2 (66.6) | 1 (50.0) | 1 (50.0) | 1 (33.3) | .360 |
| Endovascular treatment mortality | 3 (11.1) | 0 | 0 | 1 (50.0) | 1 (11.1) | 1 (6.6) | .335 |
AAS, acute aortic syndrome; CT, computed tomography; TEE, transesophageal echocardiography.
Values represent No. (%) or mean±standard deviation.
Most patients with type A AAS were surgically treated (77.0%), with a tendency for an increase in the frequency of surgical treatment during the study period (from 67.4% to 82.5%, P = .09). The mortality from type A AAS significantly decreased from 59.2% to 26.3% over time (P <.001). This decline was largely due to a fall in mortality from surgical treatment, which reduced from 45.5% in the first study period to 17.0% in the last period (P <.001) (figure 1).
Most patients with type B AAS were medically treated (80.1%). This percentage decreased in the last decade—from 91.8% to 61.7% (P <.001)—due to greater use of endovascular treatment (table 2). The frequency of surgical treatment was largely stable throughout the study, varying between 6% and 8%. The mortality of type B AAS nonsignificantly decreased from 16.2% to 10.6% (P=.15) (figure 2).
DISCUSSIONOur results show that mortality from AAS has significantly decreased in the last 2 decades due to greater use of surgical treatment and lower surgery-related mortality. For type B AAS, the use of medical therapy alone has fallen as a result of greater use of endovascular treatment. Mortality from type B AAS has decreased, but not significantly. These results are important, particularly given the lack of changes in demographic variables and in the acute onset of complications. The improved outcomes appear to be the result of better understanding of the entity, optimization of the diagnosis, and improvements in surgical, anesthetic, and intraoperative techniques.
The present study confirms that patients with type B AAS are older and more likely to have history of hypertension and atherosclerosis than those with type A AAS.8,14 In addition, patients with type A AAS have a higher frequency of hypotension and tamponade. The main contributors to the survival of patients with AAS include clinical suspicion and early diagnosis.15 In this regard, the use of CT as the first-line diagnostic technique increased over the 20-year study period due to the decrease in TEE. This higher use of CT, also reported in other studies,9 is because CT is a less invasive technique and can visualize the entire length of the aorta and evaluate the arterial branches. In addition, CT can be easily performed and interpreted by specialists with an intermediate level of experience. Due to recent advances in image quality, the usefulness of TTE in the diagnosis of aortic dissection has been confirmed, particularly when it involves the aortic root. Its use in emergency departments has become standard procedure for patients with chest pain or dyspnea. CT and TTE are considered complementary techniques and to be very useful in the diagnosis of this disease.16
The present series revealed an increase in the last 2 decades in the surgical treatment of type A AAS from 67% to 78% and a marked decrease in surgical mortality from 45% to 19%. In the same time period, registries such as IRAD,9 which only included patients treated in centers of excellence in aortic diseases, determined a decrease in surgical treatment mortality from 25% to 18%. Undoubtedly, the improvements in surgical outcomes are due to advances in cardiopulmonary bypass and in cerebral perfusion, cardiopulmonary bypass, and postoperative care strategies.11,14
The use of endovascular treatment has markedly increased in the last decade as an alternative to medical or surgical treatment in patients with type B AAS. Now, more than 30% of patients with type B AAS in our center undergo endovascular treatment in the acute phase, a similar percentage to that reported in the IRAD registry.9 This high percentage of interventional management shows that this treatment is indicated not only for major complications, such as mesenteric or peripheral ischemia or the presence of incipient signs of aortic rupture, but also for other complications such as persistent pain, poor blood pressure control, and aortic dilatation.17 The mortality of endovascular treatment has been markedly decreased through better patient selection and improved surgical experience.18,19 Various studies have shown the benefit of endovascular treatment vs open surgery in the management of complicated type B dissections.20,21 The potential mid-to-long-term impact of this treatment in patients with uncomplicated type B aortic dissection has only been demonstrated in a randomized study.22 The present study showed a nonsignificant decrease in mortality in patients with type B AAS. Notably, the mortality of patients with type B AAS who underwent endovascular treatment was similar to that of patients who were medically treated alone.
LimitationsThis study has several limitations. Although we analyzed the changes in the diagnosis, management, and mortality of acute aortic syndrome in our center in the last 2 decades, no information was available on some variables that may have influenced the results, such as the time between symptom onset and diagnosis or treatment. We also did not record if patients had directly attended the emergency department or if they had been referred from another center. However, all patients included in this series had a symptom to diagnosis interval less than 48hours. Finally, we did not differentiate between aortic dissection and intramural hematoma, although more than 80% of the patients had classic aortic dissections and it seems highly unlikely that this percentage would have changed during the study period. Undoubtedly, the results of this study cannot reflect the changes in treatment and outcomes for this entity in other Spanish centers. It is likely that the creation of an aortic disease unit and its consolidation as a referral center for this condition have been critical to the optimization of the diagnostic and therapeutic process for this disease.
CONCLUSIONSThe diagnosis and treatment of AAS have undergone major changes in the last 2 decades. CT has become the diagnostic technique of choice. Mortality from type A AAS has highly significantly decreased due to the stronger indication for surgery and the improved outcomes of surgical treatment. In type B AAS, medical therapy alone is less frequent due to the introduction of endovascular treatment; nonetheless, mortality has not significantly decreased. More studies are required to confirm if the improvements in these outcomes is generalizable to most hospital centers or is influenced by the creation of a referral center for aortic disease.
FUNDINGThis study was partially financed by the Cardiovascular Research Network (RD12/0042/0018) and the Instituto de Salud Carlos III, Spanish Ministry of Health.
CONFLICTS OF INTERESTI. Ferreira-González is Editor-in-Chief of Revista Española de Cardiología; the editorial procedure established by REC Publications has been followed to guarantee the impartial handling of the manuscript. None of the other authors has a conflict of interest related to the content of this publication.
- –
AAS has high morbidity and mortality and requires early treatment.
- –
Dissections of the ascending (type A) and descending (type B) aorta require urgent surgical or endovascular treatment to improve survival.
- –
Due to advances in diagnostic and therapeutic techniques, various registries have obtained pertinent information on this entity.
- –
However, it is difficult to analyze the effects of these advances on AAS survival.
- –
The results of this consecutive series of patients diagnosed with AAS in a single center during a 20-year period show that CT has become the diagnostic technique of choice.
- –
Mortality from type A AAS has highly significantly decreased due to the stronger indication for surgery and the improved outcomes of surgical treatment.
- –
In type B AAS, the frequency of medical therapy alone has fallen due to the development of endovascular treatment but mortality has not significantly decreased.
To Dr Jordi Soler-Soler for creating the structure and style of work that enabled the development of this clinical research line.