The number of heart-transplant recipients exceeding 20 years of follow-up is steadily increasing. However, little is known about their functional status, comorbidities, and mortality. Identifying the predictors of prolonged survival could guide the selection of candidates for the low number of available donors.
MethodsFunctional status, morbidities, and mortality of heart-transplant patients between 1984 and 1992 were analyzed. To identify predictors of 20-year survival, a logistic regression model was constructed using the covariates associated with survival in the univariate analysis.
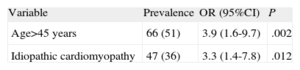
ResultsA total of 39 patients who survived 20 years (26% of patients transplanted before 1992) were compared to 90 recipients from the same period who died between 1 and 20 years post-transplantation. Major complications were hypertension, renal dysfunction, infections, and cancer. After a mean follow-up of 30 months, 6 survivors had died, yielding a mortality rate of 6% per year (vs 2.5%-3% in years 1-19). Causes of mortality were infection (50%), malignancy (33%), and allograft vasculopathy (17%). Long-term survivors were younger and leaner, and had nonischemic cardiomyopathy and lower ischemic time. Logistic regression identified recipient age <45 years (odds ratio=3.9; 95% confidence interval, 1.6-9.7; P=.002) and idiopathic cardiomyopathy (odds ratio=3; 95% confidence interval, 1.4-7.8; P=.012) as independent predictors for 20-year survival.
ConclusionsOne fourth of all heart-transplant patients in our series survived >20 years with the same graft, and most enjoy independent lives despite significant comorbidities. Recipient age <45 years and idiopathic cardiomyopathy were associated with survival beyond 2 decades. These data may help decide donor allocation.
Keywords
Advances in the medical and surgical treatment of heart failure in recent decades include the use of new drugs, cardiac resynchronization therapy-defibrillators, and ventricular assist devices; however, heart transplantation continues to be the treatment of choice for refractory cases.1–3 The enthusiasm shown when the first transplantation was performed by Christiaan Barnard in 1967 rapidly waned because of the common postoperative complications and the high early mortality associated with rejection and infection. The introduction of cyclosporin and other advances in the 1980s radically improved the prognosis of these patients and led to prolonged survival and widespread use of the technique.4 International and Spanish registries show that the median survival of transplanted patients is currently somewhat higher at 10 years, and about 14 years for those who survive the first year, which is the year with the highest incidence of complications.5,6
In the oldest transplantation programs, the group of transplanted patients with follow-up exceeding 20 years is now becoming numerous.7 However, no large series to date have described any transplantation recipients with more than 20 years of follow-up. There is only a small cohort,8 and therefore the clinical characteristics associated with prolonged survival are not well understood. Functional status, quality of life, comorbidities, and the incidence and causes of death in this period are also not well known, even though these are important aspects in patients who have received immunosuppressant medication for 20 years. This patient subgroup was the objective of our study.
METHODSA retrospective review was carried out using the databases, medical histories, and anatomic pathology reports related to patients who received a heart transplant at our hospital from September 1984 to May 2012. For parameters related to the follow-up of these patients, the patient's current status was confirmed by phone.
The patients in our study received transplants between September 1984 and May 1992. For this study, survival was defined as time to death or retransplantation due to graft failure. Our study excluded any patients who received a simultaneous heart and lung transplant as well as patients with heart retransplantation, shown in other studies to have a significantly different morbidity and mortality from that of de novo heart transplantation. All patients were classified into 3 groups according to clinical progress: patients who died within 1 year (group A), usually due to causes related to surgery and acute rejection or infectious complications, patients who survived the first year but did not survive 20 years (group B), and patients who survived more than 20 years with no need for retransplantation (group C). The last group was the subject of our study, and its characteristics are described in detail. A comparison with group B was established to identify the characteristics associated with long-term survival. The comparison group for patients from group A did not include patients who died in the early post-transplantation stage because the factors associated with early mortality have been investigated in numerous studies and are not of interest in identifying the factors associated with very long survival in surgical survivors.3,4
Immunosuppressive therapy in all patients started as triple therapy with cyclosporin, azathioprine, and prednisone. Most patients received induction therapy with muromonab (OKT3), 2 weeks initially and 1 week after 1987. Routine protocols for the withdrawal of steroids or other immunosuppressants were not used at our hospital, although a low threshold for the withdrawal of drugs causing significant adverse effects was maintained after the first year.
We analyzed 62 variables related to the recipients, donors, procedures, and events during follow-up, which are the same variables used in the Spanish registry.6
Statistical AnalysisIn the descriptive analysis of the variables, parameters with a normal distribution were described as the mean standard deviation and those with a non-normal distribution were described as the median (range). For the comparisons of quantitative variables, the Student t test was used in variables with normal distribution, and nonparametric tests if otherwise. All qualitative variables were compared by the χ2 test, and all survival rates were described using Kaplan-Meier curves.
In order to identify the characteristics associated with survival>20 years, a bivariate analysis that included characteristics of the recipient, donor, and surgery was performed. All variables associated with survival >20 years with a significance level of P<.1 were included in multivariate logistic regression models to identify predictive factors of very long survival. Statistical significance was defined as P<.05. All data were analyzed using SPSS 15.0 (Chicago, Illinois, United States).
ResultsFrom the first heart transplantation in 1984 until May 2012 at our hospital, 761 heart transplantations have been carried out in 736 patients, including 25 retransplantations and 30 heart-lung transplants. A total of 706 patients were included in the de novo heart transplantation survival curve at our hospital. The overall survival curve of our series is shown in Figure 1. The actuarial survival rates were 75% at 1 year, 64% at 5 years, 53% at 10 years, 40% at 15 years, and 26% at 20 years.
Of 183 transplants performed before May 1992, 39 patients survived and are the main focus of our study (Fig. 2). The general characteristics are shown in Table 1 and are compared to those of the control group, which included 90 patients who survived the first year but died before they completed 20 years of follow-up.
Characteristics of Patients Surviving >20 or <20 Years
| Characteristic | 20-year survivors (n=39) | Controls (n=90) | P |
| Age, years | 35.2±13.6 | 46.5±12.7 | <.001 |
| Male sex | 33 (84) | 83 (92.2) | .338 |
| BMI | 22±4.1 | 24.3±4.1 | .007 |
| Sex mismatch | |||
| Match | 31 (79) | 63 (70) | .289 |
| Male recipient-female donor | 4 (10) | 20 (22.5) | .258 |
| Female recipient-male donor | 3 (7) | 6 (6.7) | .411 |
| Weight mismatch>20% | 15 (38) | 18 (23.7) | .079 |
| Renal dysfunction | 7 (17) | 17 (20.7) | 1 |
| Insulin-dependent diabetes mellitus | 1 (2.5) | 4 (4.4) | 1 |
| Hypertension | 4 (10) | 13 (15.1) | .58 |
| Serologic group at risk of cytomegalovirus | 2 (9.1) | 3 (5.9) | .63 |
| Active smoking | 3 (7.6) | 10 (12.7) | .15 |
| Ex-smoker less than 10 years | 3 (7.6) | 1 (1.3) | .16 |
| Nonsmoker or ex-smoker >10 years | 33 (84) | 68 (86.1) | .78 |
| Inotropic treatment | 7 (18) | 29 (32.2) | .19 |
| Pretransplantation diagnosis | |||
| Dilated heart disease | 23 (59) | 24 (30) | .006 |
| Other etiologies | 16 (41) | 66 (70) | |
| Mechanical ventilation | 1 (2.5) | 13 (14.6) | .063 |
| Mechanical assist | 35 (11) | 82 (8) | .788 |
| History of extracorporeal circulation | 4 (10) | 24 (26.7) | .06 |
| Urgent transplantation | 23 (59) | 33 (45.8) | .14 |
| Donor age, years | 21.8±6.6 | 23.1±7.2 | .34 |
| Donor BMI | 23±3 | 23.3±3 | .72 |
| Cause of donor death, TBI | 35 (89) | 71 (92.2) | .73 |
| Median time of ischemia, min | 160 | 195 | .025 |
| Median time of extracorporeal circulation, min | 101 | 119 | .206 |
BMI, body mass index; TBI, traumatic brain injury.
Unless otherwise indicated, values are expressed as no. (%) or mean±standard deviation.
In the comparison of the two groups, the following variables showed a statistically significant association with survival >20 years: lower age and lower body mass index of the recipient, dilated cardiomyopathy as pretransplantation diagnosis, history of extracorporeal circulation, and lower time of ischemia during surgery. The following variables showed some trends but did not achieve statistical significance: weight disproportion>20% (if the donor was younger than the recipient) and mechanical ventilation. Other variables that were included, such as older donor age, history of diabetes mellitus, risk of cytomegalovirus (negative recipient and positive donor), and number of rejections in the first year post-transplantation were not associated with lower survival in our series.
Variables with P<.1 were included in the logistic regression model to identify those independently associated with prolonged survival (Table 2). Specifically, the model identified 2 variables: recipient age<45 years (4-fold probability of survival in excess of 20 years post-transplantation compared to the other age bracket) and idiopathic dilated cardiomyopathy as the reason for transplantation (3-fold probability of prolonged survival compared to other etiologies).
During a mean follow-up of 30 months, 6 of 39 recipients with very long survival died, which represents a survival of 84% and an average annual mortality of 6%. Only 1 patient was lost to follow-up. The actuarial survival curve at 20 years post-transplantation is shown in Figure 2. Of the deaths, 3 were due to infectious complications (pneumonia, septic shock due to peritonitis secondary to colon perforation, and sepsis of unknown origin), 2 to neoplasms (lung and tongue cancer), and 1 to heart failure associated with allograft vasculopathy.
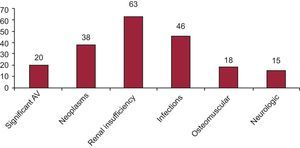
In the case of patient autonomy to perform daily activities, most (82%) of the 33 patients who survived at the time of the study were completely autonomous, whereas 6% were partially dependent and 12% were completely dependent. The functional limitations were attributed to osteomuscular diseases in half the cases, whereas the others were due to vascular and neurologic causes.
The incidence of common complications in transplanted patients was recorded during follow-up. In terms of infectious complications, 8 patients (20%) had hospitalizations for bacterial infections during the follow-up period, mainly respiratory, urinary, and soft tissues, and another 10 (26%) experienced major viral infections (4 due to cytomegalovirus, 1 herpetic encephalitis caused by herpes simplex virus 2, 3 cases of chicken pox zoster, 1 hepatitis B infection, and 2 hepatitis C infections, of which 1 had cirrhosis of the liver as a complication that required liver transplantation, which was successful).
In all, 38% of the survivors have had some kind of malignancy, mainly benign skin tumors (60%), followed by solid-organ neoplasms (tongue, lung, and liver), and only 1 presented a blood cancer.
After 20 years of transplantation, most (84%) patients presented with chronic kidney disease, with a mean estimated glomerular filtration rate of 59 mL/min. A total of 36% had stage 2 renal insufficiency, 48% had stage 3, and 15% had stage 4. At the time of writing, none had required definitive renal replacement therapy. Cardiovascular risk factors were very prevalent: 94% had hypertension, 87% had hyperlipidemia, and 15% had diabetes mellitus.
Patients underwent coronary angiography every 3 years according to our local protocol for the detection of allograft vasculopathy; this was often accompanied by intravascular ultrasound. A total of 35 (89%) patients presented some degree of allograft vasculopathy, although most (72%) had no significant coronary lesions. In the case of patients with an intravascular ultrasound study, 27% were classified as Stanford class II, 11% as Stanford class III, and 58% as Stanford class IV. To date, 3 of these recipients have required percutaneous revascularization (which failed in 1 case). Two of them had systolic graft dysfunction, with 40% left ventricular ejection fraction.
Nine patients presented significant arrhythmias. One of them required ablation for ventricular tachycardia, and 8 (20%) required pacemaker implantation for symptomatic bradyarrhythmia at some time during the course of their clinical progress.
Figure 3 shows the prevalence of the main complications in the long-term survival group.
In terms of immunosuppression, 1 or more components of the initial triple therapy had been withdrawn in most patients, such that 76% were being treated with 2 drugs at the time of the study. The most common combination was cyclosporin and corticosteroid (13 patients [43%]), followed by cyclosporin and azathioprine (5 patients [16%]), cyclosporin and mycophenolate mofetil (3 patients [10%]), cyclosporin plus everolimus (2 patients [6%]), and everolimus plus prednisone (3 patients [10%]). One patient received a combination of tacrolimus and mycophenolate and another, everolimus with mycophenolate.
Cyclosporin was usually switched due to renal dysfunction, azathioprine because of blood count abnormalities (leukocytopenia), and corticosteroids because of recurrent infections or metabolic disorders such as hard-to-control diabetes mellitus or osteoporosis. Patients with rare infections or malignancies with considerable repercussions eventually were switched to monotherapy.
DISCUSSIONAdvances implemented in recent decades in the management and follow-up of patients with heart transplantation have allowed prolonged survival rates to be obtained.4–6 At present, 20-year survival rates in the national and international registries are >20%, similar to the 26% reported in our series.5,6 As in the case of international registries, the initial mortality observed in our curve is high for the current standards due to the relative weight of the procedures carried out at the start of the series in the 1980s and early 1990s, but decreases when only recent surgical patients are taken into account. This is influenced not only by the learning curve, but also by advances in immunosuppression, prophylaxis of infectious diseases, and monitoring and management of the various types of rejection.
From the quantitative point of view, mortality after the first year becomes more stable and the mortality rate remains steady. Annual mortality was 2.5% in our series, 2.6% in the Spanish Heart Transplantation Registry, and 3.5% in the Registry of the International Society for Heart and Lung Transplantation (ISHLT).5,6 In comparison, the mortality of the general population between 55 and 60 years of age in Spain is approximately 0.5%.7 In comparison to these figures, recipients who have reached 20 years post-transplantation in our series showed a mortality rate of 6% per year of follow-up; however, this figure should be viewed with caution, due to the low numbers of patients and of deaths during follow-up.
Although several articles on the long-term follow-up of transplant patients have been published in recent years, most of these studies had a follow-up period of the first 15 years8–13 and only a few lasted as long as 20 years.14,15 In various studies, particularly in those published more recently, the factors associated with longer survival were consistent with those identified in our series. These included low recipient age,11,13 lower body mass index at the time of transplantation,11,12 nonischemic diagnosis prior to transplantation,11–13 and lower graft ischemia time.11,12
In contrast, other factors identified in these series, such as low donor age,13 serologic group at risk of cytomegalovirus infection,14 smoking,14 and history of diabetes mellitus,14 which have been found to be predictors, were not associated with survival>20 years in our series. Several reasons that might explain this discrepancy in our series include donor age, which was much lower in all cases, in keeping with the practice at that time. Nonetheless, the low percentage of patients with acknowledged smoking, diabetes mellitus, and serologic group at risk of cytomegalovirus infection in our series prevented an appropriate assessment of their influence in our study.
An analysis of the late causes of death after heart transplantation show that allograft vasculopathy and neoplasms predominate after the first year. In patients who survive the first decade, when allograft vasculopathy is more prevalent, cancer appears to be the main cause of death. Large series with 15 years of follow-up report malignancies as the leading cause of death (35.8%), followed by allograft vasculopathy (24.7%) and infections caused by microorganisms other than cytomegalovirus (8.6%). In our patients, there were few deaths. However, the same causes of death, with slightly different prevalences, were observed after 20 years of the transplantation; predominance of infections was observed, followed by neoplasms, and allograft vasculopathy in 1 case.14
The progress of these patients is characterized by the usual complications associated with transplantation and chronic immunosuppression, such as recurrent bacterial and viral infections, chronic kidney disease, hypertension, diabetes mellitus, hyperlipidemia, and neoplasms. In our series, most patients (84%) presented some degree of renal dysfunction after 20 years of transplantation, a figure that appears to be consistent with the rate of kidney disease (65%) reported by the ISHLT registry at 10 years of follow-up; it is very likely that prolonging follow-up in these patients to 20 years would show figures highly consistent with ours. In the ISHLT registry, 4% of patients were receiving renal replacement therapy at 10 years post-transplantation. None of our 39 patients are in the dialysis program, although 15% presented creatinine clearance<30mL/min, which means that, over time, some might require replacement therapy. Similar to international experience, in our hospital's cohort of transplant patients before 1992 who died within 20 years, 4% required hemodialysis before they died.
In terms of the prevalence of cardiovascular risk factors, we have no data beyond 5 years in the ISHLT registry for comparison. However, the figures from this registry seem consistent with ours, as most patients already present hypertension and hyperlipidemia at 5 years, similar to the patients in our series.
Among osteomuscular complications, osteoporosis is the most common and is associated with significant functional limitation in many cases. This frequency is probably due to prolonged exposure to corticosteroids, and was the cause of corticosteroid discontinuation in many cases.
Despite all these complications, the quality of life of patients in our series appears to very acceptable, as 82% of subjects were independent for activities of daily living. In international registries, this parameter has been similarly assessed, but data are only shown for the first 5 years of follow-up, with figures for complete autonomy of around 90%. This is the first time the parameter has been assessed after more than 2 decades of immunosuppression.
In series that evaluated the early progress of transplantation, acute rejection has been described as a major cause of mortality. Over the years, however, it becomes less common and even though most patients at 20 years receive significantly lower immunosuppression, in our series there were virtually no events that could be related to acute cellular rejection. We cannot rule out that this privileged subgroup of recipients may have some degree of immunologic tolerance of their respective grafts. Therefore, in our case we preferred to decrease the immunosuppressive burden considerably.
LimitationsThis study has several limitations. First, it is a retrospective study conducted at a single center, and therefore we cannot rule out the presence of local factors that could have affected the outcomes and/or follow-up. The relatively low number of patients in the survivor group after 20 years post-transplantation, although obviously justifiable, means that the conclusions of the statistical analysis should be viewed with caution.
Second, the quality of life data were assessed and collected by the cardiologist who performed the follow-up at the outpatient clinic, rather than by a standardized tool such as a validated questionnaire.
CONCLUSIONSOne fourth of all heart-transplant patients from the start of our experience achieved survival >20 years with the same graft. Predictors of this favorable outcome included recipient age<45 years and idiopathic dilated cardiomyopathy as a pretransplantation diagnosis. The complications and mortality that affect these patients are those known to be present in the late phase following heart transplantation, although with a slightly higher incidence. However, functional status is favorable in most of these recipients, which confirms the net benefit of transplantation in this subgroup.
New studies to identify recipient and donor characteristics that predict very long-term survival in large series may contribute to better allocation of the few donors currently available.
CONFLICTS OF INTERESTNone declared.