The resting 12-lead electrocardiogram (ECG) has been used in the evaluation of young asymptomatic individuals to detect pre-existing heart disease, but systematic ECG use is controversial and there are no data on this population in our environment. We aimed to determine the prevalence and spectrum of electrocardiographic findings in a population of secondary school students.
MethodsWe conducted an observational, cross-sectional study of resting ECG findings in all 13 to 14-year-old secondary school students in a region of the province of Gerona between 2009 and 2017. ECG findings were classified into 3 groups according to the modified criteria of Corrado et al.: normal ECG findings, ECG findings suggestive of adaptive changes, and pathologic findings. Students with pathologic ECG findings were referred to a tertiary hospital, and complementary tests were performed according to a pre-established protocol.
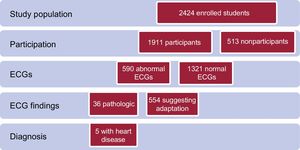
ResultsA total of 1911 ECGs were obtained, with a participation rate of 79% of all high school students. In all, 1321 students (69%) had a normal ECG, 554 (29%) showed ECG findings suggestive of adaptive changes, and 36 (2%) had pathologic ECG findings. Among the group with pathologic findings, 5 (14%) had cardiovascular disease. The prevalence of heart disease in this group of asymptomatic secondary school students was 0.3%.
ConclusionsOne third of the students had ECG findings that were mostly suggestive of physiological adaptation. One seventh of the students with pathologic ECG findings had pre-existing heart disease, although the overall prevalence of pre-existing heart disease was low.
Keywords
Most young people aged 13 to 14 years are in good health. Sudden cardiac death (SCD) is rare among these individuals but has a considerable social impact. The main causes of SCD reported in persons younger than 35 years are channelopathies and structural heart disease, particularly arrhythmogenic right ventricular dysplasia and hypertrophic cardiomyopathy.1–3 Heart disease leading to SCD among young people tends to progress with no prior symptoms and remains unnoticed until the fatal event, making early screening necessary.4
Cardiovascular screening of a healthy population based on a resting electrocardiogram (ECG) has aroused considerable debate,5,6 but no international consensus has been reached on recommended testing. There is only scant evidence in healthy young populations, and ECG screening programs in young people based on obsolete ECG criteria have shown little success in detecting underlying heart disease, hindering an assessment of cost-effectiveness in this population group.7,8
In Spain, experience with ECG screening is limited to soccer players9 and elite athletes,10 in whom the instrument has proven to be cost-effective.11,12 The European Society of Cardiology (ESC) published its initial recommendations for ECG interpretation in athletes in 200513 and has issued several updates by 201714-16 to lower the number of false-positive results.
The aim of the present study was to identify ECG changes in a young, asymptomatic, apparently healthy population to correlate pathologic ECG findings with a possible early diagnosis of underlying heart disease.
METHODSPopulation and Study PeriodThis was an observational, cross-sectional study of a young, apparently healthy cohort undergoing ECG screening to identify ECG changes. The study population included 2424 young students enrolled in the second year of compulsory secondary education at high schools throughout the area of Pla de l’Estany (Girona, Spain) from the 2009 to 2010 school year to the 2016 to 2017 school year. This area has a population of 30 152 inhabitants with 4 high schools and a total of 10 homerooms. The study was conducted using a voluntary nonprobabilistic sample.
Data CollectionA team composed of physicians and nurses visited area schools. The study included all students in the region who voluntarily signed the informed consent form, with authorization from their parents. All students underwent ECG screening according to current recommendations.17 The study was approved by the Clinical Research Ethics Committee of the Hospital Clínic de Barcelona, and the research team was committed to compliance with Organic Act 15/1999 on Personal Data Protection and with the ethical principles established in the Declaration of Helsinki.18
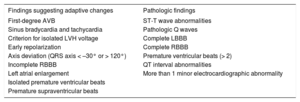
The aim of this study, conducted in a healthy young population, was to identify ECG changes according to the criteria listed in Table 1, based on the modified criteria of Corrado et al.,19 equivalent to the latest ESC recommendations.14-16 Two independent cardiologists separately analyzed all ECGs. Inconsistent tracings were resolved by a common consensus reading, using the criteria listed in Table 1.
Classification of Electrocardiographic Findings
| Findings suggesting adaptive changes | Pathologic findings |
|---|---|
| First-degree AVB | ST-T wave abnormalities |
| Sinus bradycardia and tachycardia | Pathologic Q waves |
| Criterion for isolated LVH voltage | Complete LBBB |
| Early repolarization | Complete RBBB |
| Axis deviation (QRS axis < –30° or > 120°) | Premature ventricular beats (> 2) |
| Incomplete RBBB | QT interval abnormalities |
| Left atrial enlargement | More than 1 minor electrocardiographic abnormality |
| Isolated premature ventricular beats | |
| Premature supraventricular beats |
AVB, atrioventricular block; LBBB, left bundle-branch block; LVH, left ventricular hypertrophy; RBBB, right bundle-branch block.
The basic ECG measurements were evaluated: heart rate, P wave, PR segment, complex QRS, QT interval, and corrected QT interval. ECG changes were classified using the criteria described in the above point (Table 1) into 3 groups: ECG with no ECG changes, ECG findings suggesting adaptive changes, and pathologic ECG findings. Based on the new recommendations, axis deviation and left atrial enlargement were classified as suggesting adaptive changes.
Students with pathologic findings underwent further study according to the following protocol: all students were referred to the pediatric cardiology unit at a tertiary hospital for a detailed medical history, careful physical examination, ECG, and echocardiography. If the reason for referral was arrhythmia, the student also underwent 24-hour Holter monitoring according to protocol to detect any arrhythmogenic burden as well as conventional stress testing to identify exercise response. If the ECG findings suggested structural heart disease, cardiac magnetic resonance was performed.
Statistical AnalysisThe results are expressed as the mean±standard deviation for continuous variables with a normal distribution, as medians for continuous variables with a non-Gaussian distribution, and as percentages for categorical variables. The characteristics of students with and without ECG changes were compared by the chi-square test or the Fisher exact test for categorical variables. Quantitative variables were analyzed by the Student t test if normally distributed or by the Mann-Whitney U-test if nonnormally distributed. Statistical significance was set at P < .05. All statistical analyses were performed using SPSS 22.0 for Windows (SPSS Inc.; Chicago, Illinois, United States).
RESULTSIn all, 1911 students (79% of 2424 enrolled students) participated in ECG screening (Figure 1). A total of 254 students (92% participation) were studied in 2010, the year with the highest percentage, whereas only 61% (n=162) participated in 2015. The reasons for nonparticipation were unknown. The mean age of participants was 14 years. A total of 50.3% were girls. As of 2014, the mean height (163±8cm), mean weight (55±11kg), and mean body mass index (20.6±4) were also recorded. Information was also obtained on students’ regular physical activity: 48% of the population was sedentary. Soccer (n=167) was the most common regular sport. A total of 66% of the population had not undergone resting ECG before screening.
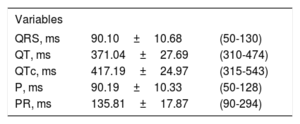
The basic ECG measurements were mean heart rate (range) 78.6±13.8 (35-143) bpm; maximum corrected QT segment, 543ms; and maximum PR interval, 294ms. All other measurements are listed in Table 2.
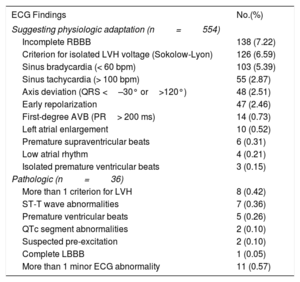
According to the classification used, 1321 (69%) students had normal ECG findings, 554 (29%) had ECG findings suggesting adaptive changes, and only 36 (2%) showed pathologic findings. The ECG findings are listed in Table 3.
Electrocardiographic Findings
| ECG Findings | No.(%) |
|---|---|
| Suggesting physiologic adaptation (n=554) | |
| Incomplete RBBB | 138 (7.22) |
| Criterion for isolated LVH voltage (Sokolow-Lyon) | 126 (6.59) |
| Sinus bradycardia (< 60 bpm) | 103 (5.39) |
| Sinus tachycardia (> 100 bpm) | 55 (2.87) |
| Axis deviation (QRS <–30° or>120°) | 48 (2.51) |
| Early repolarization | 47 (2.46) |
| First-degree AVB (PR> 200 ms) | 14 (0.73) |
| Left atrial enlargement | 10 (0.52) |
| Premature supraventricular beats | 6 (0.31) |
| Low atrial rhythm | 4 (0.21) |
| Isolated premature ventricular beats | 3 (0.15) |
| Pathologic (n=36) | |
| More than 1 criterion for LVH | 8 (0.42) |
| ST-T wave abnormalities | 7 (0.36) |
| Premature ventricular beats | 5 (0.26) |
| QTc segment abnormalities | 2 (0.10) |
| Suspected pre-excitation | 2 (0.10) |
| Complete LBBB | 1 (0.05) |
| More than 1 minor ECG abnormality | 11 (0.57) |
AVB, atrioventricular block; ECG: electrocardiogram; LBBB, left bundle-branch block; LVH, left ventricular hypertrophy; RBBB, right bundle-branch block.
ECG changes were found in 590 (31%) students, with 554 ECGs classified as suggesting adaptive changes. The most common were right bundle-branch block (7.22%, n=138), left ventricular hypertrophy based on a single Sokolow-Lyon voltage criterion (6.59%, n=126), and sinus bradycardia (5.39%, n=103).
Pathologic Electrocardiographic FindingsPathologic findings were identified in 36 patients, who were then referred to the pediatric cardiology unit for further testing. The 3 most common pathologic findings were as follows: more than 1 ECG finding suggesting adaptive changes (n=11), more than 1 criterion for left ventricular hypertrophy (n=8), and ST-T abnormalities (n=7).
Cardiologic Assessment of Patients with Pathologic ElectrocardiogramAll students referred underwent echocardiography, which identified 1 case of bicuspid aortic valve type I, 1 of mitral valve prolapse, and 2 of left ventricular hypertrophy with interventricular septum of up to 13mm. In 1 student, echocardiography suggested coronary fistula, which was later confirmed by cardiac magnetic resonance. This student had ST-segment abnormalities on ECG. The ECG was repeated in a student with a maximum corrected QT segment of 543ms, and showed a standardized corrected QT segment with no structural heart disease. A total of 17 students underwent 24-hour Holter testing, which identified first-degree atrioventricular block alternating with second-degree atrioventricular block, Mobitz I, in 1 student whose medical history reported recurrent syncope. A total of 11 underwent conventional stress testing, but no arrhythmic events were identified during exercise. The student with left bundle-branch block on ECG had no structural heart disease. In the end, Wolff-Parkinson-White syndrome was confirmed and ablated by electrophysiologic study in 1 patient involved in a high-performance sport. Consequently, the overall rate of heart disease was 0.3% (n=5) of the study population.
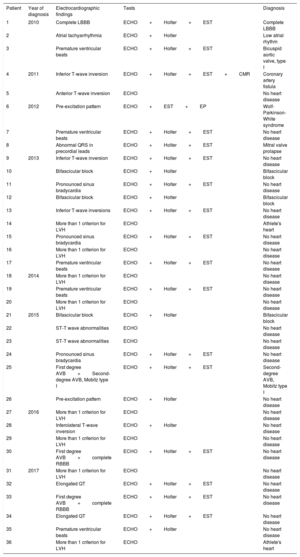
Correlation Between Pathologic Electrocardiographic Findings and Underlying Heart DiseaseTable 4 correlates ECG findings with conditions detected by complementary tests. There was correlation in the 2 cases of left ventricular hypertrophy with repolarization abnormalities along with ECG evidence of hypertrophy (Sokolow-Lyon). These 2 cases of left ventricular hypertrophy did not meet the criteria for hypertrophic cardiomyopathy, as the interventricular septal measurements were 13mm. Athlete's heart was classified as regular practice of sport (soccer or basketball), no family history of hypertrophic cardiomyopathy, and factors suggesting the gray zone of left ventricular hypertrophy according to the ESC20 (no family history of hypertrophic cardiomyopathy, absence of T-wave inversion on ECG, symmetric left ventricular hypertrophy, and normal diastolic pattern on echocardiography).
Correlation of Electrocardiographic Findings With Underlying Heart Disease
| Patient | Year of diagnosis | Electrocardiographic findings | Tests | Diagnosis |
|---|---|---|---|---|
| 1 | 2010 | Complete LBBB | ECHO+Holter+EST | Complete LBBB |
| 2 | Atrial tachyarrhythmia | ECHO+Holter | Low atrial rhythm | |
| 3 | Premature ventricular beats | ECHO+Holter+EST | Bicuspid aortic valve, type I | |
| 4 | 2011 | Inferior T-wave inversion | ECHO+Holter+EST+CMR | Coronary artery fistula |
| 5 | Anterior T-wave inversion | ECHO | No heart disease | |
| 6 | 2012 | Pre-excitation pattern | ECHO+EST+EP | Wolf-Parkinson-White syndrome |
| 7 | Premature ventricular beats | ECHO+Holter+EST | No heart disease | |
| 8 | Abnormal QRS in precordial leads | ECHO+Holter+EST | Mitral valve prolapse | |
| 9 | 2013 | Inferior T-wave inversion | ECHO+Holter+EST | No heart disease |
| 10 | Bifascicular block | ECHO+Holter | Bifascicular block | |
| 11 | Pronounced sinus bradycardia | ECHO+Holter+EST | No heart disease | |
| 12 | Bifascicular block | ECHO+Holter | Bifascicular block | |
| 13 | Inferior T-wave inversions | ECHO+Holter+EST | No heart disease | |
| 14 | More than 1 criterion for LVH | ECHO | Athlete's heart | |
| 15 | Pronounced sinus bradycardia | ECHO+Holter+EST | No heart disease | |
| 16 | More than 1 criterion for LVH | ECHO | No heart disease | |
| 17 | Premature ventricular beats | ECHO+Holter+EST | No heart disease | |
| 18 | 2014 | More than 1 criterion for LVH | ECHO | No heart disease |
| 19 | Premature ventricular beats | ECHO+Holter+EST | No heart disease | |
| 20 | More than 1 criterion for LVH | ECHO | No heart disease | |
| 21 | 2015 | Bifascicular block | ECHO+Holter | Bifascicular block |
| 22 | ST-T wave abnormalities | ECHO | No heart disease | |
| 23 | ST-T wave abnormalities | ECHO | No heart disease | |
| 24 | Pronounced sinus bradycardia | ECHO+Holter+EST | No heart disease | |
| 25 | First degree AVB+Second-degree AVB, Mobitz type I | ECHO+Holter+EST | Second-degree AVB, Mobitz type I | |
| 26 | Pre-excitation pattern | ECHO+Holter | No heart disease | |
| 27 | 2016 | More than 1 criterion for LVH | ECHO | No heart disease |
| 28 | Inferolateral T-wave inversion | ECHO+Holter | No heart disease | |
| 29 | More than 1 criterion for LVH | ECHO | No heart disease | |
| 30 | First degree AVB+complete RBBB | ECHO+Holter+EST | No heart disease | |
| 31 | 2017 | More than 1 criterion for LVH | ECHO | No heart disease |
| 32 | Elongated QT | ECHO+Holter+EST | No heart disease | |
| 33 | First degree AVB+complete RBBB | ECHO+Holter+EST | No heart disease | |
| 34 | Elongated QT | ECHO+Holter+EST | No heart disease | |
| 35 | Premature ventricular beats | ECHO+Holter | No heart disease | |
| 36 | More than 1 criterion for LVH | ECHO | Athlete's heart |
AVB, atrioventricular block; ECHO, echocardiography; EST, exercise stress test; LBBB, left bundle-branch block; LVH, left ventricular hypertrophy; RBBB, right bundle-branch block.
There was also correlation in the case of coronary fistula and T-wave abnormalities (T-wave inversion). In the patient with valve disease, there was no clear correlation with ECG findings.
DISCUSSIONThis is the first Spanish study to investigate ECG changes in a large sample of the young, healthy population. Two main aspects of the study should be highlighted: the high prevalence of ECG findings (31%), mainly suggesting physiologic adaptation, and the low prevalence of underlying heart disease (0.3%).
Our study identified a higher percentage of ECG findings than earlier series.6,21 These differences may be explained by the criteria used, the study population, and the interpretation and heterogeneity of ECG findings suggesting adaptive changes used in the various series. Cardiovascular screening began in the 2009 to 2010 school year and used the modified ECG criteria described by Corrado et al.,19 which excluded the isolated criterion of left ventricular hypertrophy as a pathologic ECG finding, in an attempt to lower the rate of false positives. Dhutia et al.22 compared various ECG criteria and concluded that later updates improved the effectiveness of cardiovascular screening. In this study, other modifications were made to minimize false-positive results, based on the evidence reported, defining left atrial enlargement and axis deviation as ECG findings suggesting adaptive changes.23 ECG was used for screening based on the meta-analysis results reported by Harmon et al.,24 who compared cardiovascular screening consisting of medical history, physical examination, or ECG, and determined that ECG was the most efficient approach to detecting underlying heart disease. ECG is an inexpensive, noninvasive instrument that is rapid, reproducible, and essential in cardiology. It shows good sensitivity and specificity for detecting SCD-related heart disease, although systematic use in the general population is still controversial.25,26 There is scant evidence of ECG screening in young people, although the consensus is to recommend it for athletes.27
In Japan, systematic screening of a healthy young population showed a prevalence of 0.01% to 0.04% for underlying heart disease among secondary school students28 according to ECG criteria now obsolete. Another Asian study showed a prevalence of 7% pathologic ECGs when using various ECG criteria.6 The most prevalent heart disease detected by ECG screening is Wolff-Parkinson-White syndrome, congenital abnormalities of the coronary arteries, and hypertrophic cardiomyopathy.29 These data agree with our study, which observed 1 case of Wolff-Parkinson-White syndrome, 1 case of coronary abnormality, and 2 cases of left ventricular hypertrophy which did not meet the criteria for hypertrophic cardiomyopathy. There were no cases of arrhythmogenic right ventricular dysplasia or channelopathies.
A low correlation was observed between ECG findings and underlying heart disease. Challoumas et al.30 described a correlation between coronary fistula and T-wave abnormalities on electrocardiography. The case of pre-excitation was confirmed to be Wolff-Parkinson-White syndrome. However, the detection of bicuspid aorta valve and mitral valve prolapse may have been incidental. There were no cases of hypertrophic cardiomyopathy, and only 2 cases were identified of athlete's heart. It is still a challenge to determine whether an ECG finding is pathologic or suggests adaptive changes, and accurate classification has considerable impact on treatment.
SCD has a number of causes, with a low proportion of underlying heart disease, most of them undetectable on ECG. The overdiagnosis of structural heart disease in asymptomatic patients may lead to emotional stress in affected students and excessive costs for the health system due to unnecessary additional tests. The detection of pathologic changes or structural heart disease does not imply that the prognosis can be improved, nor any assurance that the prognosis will not worsen due to poor medical practice. At present, there are reasonable doubts regarding the effectiveness and safety of ECG-based cardiovascular screening.
CONCLUSIONSIn an unselected youth population, ECG-based cardiovascular screening identified 31% of ECG changes, most of them suggesting adaptive changes. Underlying heart disease was identified in 1 of every 7 students with pathologic ECG findings, although the overall prevalence of underlying heart disease in the study population was low. In view of the study results, the research team concluded that reasonable doubts remain about the effectiveness and safety of ECG as a large-scale cardiovascular screening instrument in the healthy young population.
FUNDINGThe study was partially funded with a research grant from the Ministry of Education, Culture and Sport. None of the article authors have received financial compensation.
CONFLICTS OF INTERESTNone declared.
- –
Routine ECG screening is recommended in athletes to prevent SCD, but there is little evidence on routine ECG screening in the general population using current ECG criteria. Early detection of underlying heart disease leading to SCD in young people is a significant public health challenge, as SCD is a fatal event in apparently healthy individuals.
- –
This study provides descriptive data on the ECG findings of a broad, representative population sample of young secondary school students. The prevalence of ECG changes was high, although most suggested adaptive changes. Underlying heart disease was identified in only 0.3% of the population.
.
We would like to express our appreciation to the Banyoles Primary Care Center, the City Council of Banyoles, the School of Medicine of the University of Girona, and the Professional Association of Physicians of Girona for their assistance.