The prevalence of heart failure remains high and represents the highest disease burden in Spain. Heart failure units have been developed to systematize the diagnosis, treatment, and clinical follow-up of heart failure patients, provide a structure to coordinate the actions of various entities and personnel involved in patient care, and improve prognosis and quality of life. There is ample evidence on the benefits of heart failure units or programs, which have become widespread in Spain. One of the challenges to the analysis of heart failure units is standardization of their classification, by determining which “programs” can be identified as heart failure “units” and by characterizing their complexity level. The aim of this article was to present the standards developed by the Spanish Society of Cardiology to classify and establish the requirements for heart failure units within the SEC-Excellence project.
Keywords
The estimated prevalence of heart failure (HF) is high and ranges from 7% to 8% in individuals older than 45 years.1 The Primary Care Clinical Database of the Spanish National Health System estimates 9.2 cases per 1000 population (8.1 men and 10.2 women) aged between 14 and 64 years and 35.5 cases per 1000 population in individuals aged 65 years or older (33.1 men and 37.3 women).2 These ratios are closer to those reported in European studies (approximately 1.5%).3 Heart failure is a health problem of the first order in Spain.4 Among heart diseases, this condition provokes the highest number of hospital admissions with prolonged hospital stay (mean 8.5 days in 2013) and is a major cause of mortality and hospital readmissions (9.7% and 20% in 2013, respectively),5 as well as loss of quality of life.6,7 Therefore, its systematic management is a priority to improve health outcomes and optimize resource use.8
Heart failure units (HFU) have been developed to systematize the diagnosis, treatment, and clinical follow-up of HF patients.9 The application of a universal HFU model is not feasible because of differences in organizational structures and the available resources. In fact, the main determinants of the final model are local conditions.10 There are many reasons underlying the need for HFU, which include epidemiological, clinical, therapeutic, and economic aspects.11–13
The benefits of HFUs or HF programs have been amply demonstrated in both observational and randomized studies, such as fewer emergency department visits and fewer readmissions (between 35% and 90%), improved treatment adherence, and increased survival.8,11–35 In Spain, the integration of cardiology and primary care has been shown to improve the management of HF.36,37 These findings have been confirmed by several meta-analyses, which have also shown that more complex models confer an additional survival benefit.38–40 Some studies have shown that these benefits are maintained in the long-term, although continuous intervention may be needed.41,42 Several performance measures have been proposed for HFUs, some of which address process management while others address process indicators and HFU outcomes.43
Heart failure units or HF programs currently face multiple challenges, namely, their widespread implementation in the health system, the incorporation of new clinical management strategies, and their integration within the different levels of the care process. Jaarsma et al.44 conducted a survey of 673 hospitals in 43 European countries and only 7 had specialized HF programs in more than 30% of their hospitals. The results of the recently published MOSAIC (Map of the Organization of Heart Failure in Spain) project show that the number and complexity of HFUs has grown slightly in recent years.45 Similar results have been found in other countries.46
One of the challenges to analysis of HFUs in Spain is to standardize their classification, by determining which “programs” can be identified as HF “units” and by characterizing their level of complexity. The European Society of Cardiology Heart Failure Association has proposed a set of standards for HF management programs.47
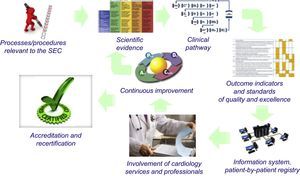
THE SPANISH SOCIETY OF CARDIOLOGY SEC-EXCELLENCE PROJECTThe Spanish Society of Cardiology (SEC) has made quality assurance in the clinical management of heart disease patients one of its priority objectives.48 Within the SEC-Quality project, the society has launched the SEC-Excellence project, which is dedicated to the evaluation and accreditation of healthcare processes in cardiology services. An overview of its basic philosophy is presented in the Figure. To be able to provide performance accreditation, it is essential to guarantee adherence to measurable and objective minimum goals and standards.49 Given the enormous impact of HF, and based on the above aspects, the SEC-Excellence project Executive Committee decided that HF was the first process to be developed.
The SEC-Excellence Heart Failure Project. Methodology Used to Determine Standards and Types of Heart Failure UnitsIn Spain, although attention and adherence to the recommendations of the European guidelines for cardiology services are excellent,50 there are marked differences in outcomes (mortality, readmissions) between hospitals.5 The preparation by the SEC of process and HFU standards is part of the strategy of the Spanish National Health System to manage chronicity51 and ischemic heart disease.52,53
The SEC-Excellence HF Committee was asked to define standards for the clinical management (process) of HF patients and the HFUs involving the participation of cardiology services. The committee comprised experts nominated by the Executive Committee of the SEC-Excellence project and the Heart Failure Section of the SEC. The committee developed a proposal for standards based on the available scientific, organizational, and managerial evidence, which included the document on standards and recommendations in the area of cardiology,48 INCARDIO,54 the guidelines of the European Society of Cardiology (ESC),55 the American College of Cardiology (ACC),56,57 and the NICE (National Institute for Health and Excellence),58–60 other scientific-professional institutions,61,62 and Spanish autonomous communities.63 The proposed standards were submitted to the presidents of the SEC-affiliated scientific sections and societies, and to the heads of the cardiology services that are members of the SEC.
The committee developed and defined 3 aspects: a) the classification and nomenclature of HFUs; b) standards for the different types of units proposed, and c) standards for general care processes in HF. Each cardiology department will be able to request accreditation for the HF care process and for the different types of units available. The accreditation process will begin when a service voluntarily applies to the SEC-Excellence committee for inclusion in the assessment process. The SEC-Excellence committee will examine adherence to the standards (Table 1, Table 2, and Table 3) through an external audit process, which will be validated by members of the SEC-Excellence HF Committee. Adherence to quality standards by a service or unit may lead to accreditation for Excellence in HF by the SEC. The accreditation of Excellence in HF will not be indefinite, but will be periodically reviewed to ensure that the service continues to meet the proposed quality and performance standards. To ensure the feasibility of the process, a pilot phase will be initially conducted with a small group of hospitals that will include a regionally balanced distribution of services and types of units (according to their degree of complexity). After verifying the reliability of the process, all public and private cardiology services and units will be able to voluntarily apply for accreditation in Excellence in HF by the SEC.
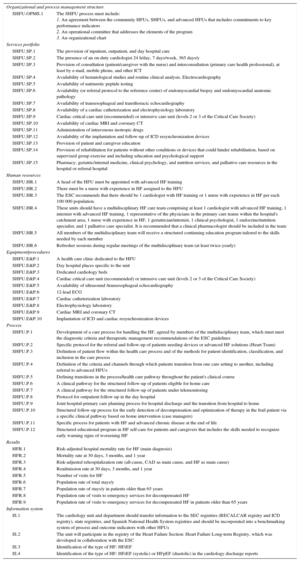
Standards for Community Heart Failure Units
| Organizational and process management structure | |
| CHFU.OPMS.1 | The CHFU process should include the following domains: 1. An agreement between the stakeholders and institutions based on a regionally-based care agreement that includes commitments to key performance indicators 2. An operational committee that addresses the elements of the program 3. An organizational chart |
| Services portfolio | |
| CHFU.SP.1 | Definition of the geographical area and population (integrated primary care teams) |
| CHFU.SP.2 | Integration into a single services portfolio that includes all the resources useful to the HF management process, whether hospital-based, primary care-based, or community-based |
| CHFU.SP.3 | Provision of inpatient, outpatient, and day hospital care |
| CHFU.SP.4 | Provision of consultation (patient/caregiver with nurses) and interconsultation (primary care health professional) by at least e-mail, mobile phone, and other ICT |
| CHFU.SP.5 | Availability of hematological studies and routine clinical analysis. Electrocardiography |
| CHFU.SP.6 | Availability of natriuretic peptide testing |
| CHFU.SP.7 | Availability of transthoracic echocardiography |
| CHFU.SP.8 | Provision of patient and caregiver education |
| CHFU.SP.9 | Provision of rehabilitation in the hospital or in a referral hospital for patients without other conditions or devices that hinder rehabilitation, based on supervised group exercise and including education and psychological support |
| CHFU.SP.10 | Pharmacy service and possibility of interconsultation in the hospital or referral hospital with geriatric/internal medicine, clinical psychology, nutrition, and social support services, and palliative care resources |
| Human resources | |
| CHFU.HR.1 | A head of the CHFU must be formally appointed. The head must have training in HF |
| CHFU.HR.2 | There must be a nurse with experience in HF assigned to the CHFU |
| CHFU.HR.3 | These units should have a multidisciplinary HF care team comprising at least 1 cardiologist and/or internist trained in HF, 1 representative of the physicians in the primary care teams within the hospital's catchment area, and 1 nurse with experience in HF |
| CHFU.HR.4 | The ESC recommends that there should be 1 cardiologist or internist trained in HF and 1 nurse with experience in HF per each 100 000 population |
| CHFU.HR.5 | Training workshops for family physicians, hospital nurses, and primary care nurses |
| CHFU.HR.6 | Training rotations for primary care physicians with a special interest in HF in the hospital CHFU |
| CHFU.HR.7 | Refresher sessions during regular meetings of the working group (at least twice a year) |
| Equipment/procedures | |
| CHFU.E&P.1 | A health care clinic dedicated to the CHFU |
| CHFU.E&P.2 | Day hospital places specific to the unit |
| CHFU.E&P.3 | Dedicated cardiology beds |
| CHFU.E&P.4 | Cardiac critical care unit or intensive care unit (Critical Care Society levels 2 or 3) |
| CHFU.E&P.5 | Availability of an ultrasonographer |
| CHFU.E&P.6 | 12-lead ECG |
| Process | |
| CHFU.P.1 | Development of a process or integrated care pathway for HF management, agreed by members of the multidisciplinary team, which must fulfil the diagnostic criteria and therapeutic management recommendations of the ESC guidelines |
| CHFU.P.2 | Definition of patient flow within the process/health care pathway, and of the methods of patient identification, classification, and inclusion in the care process |
| CHFU.P.3 | Definition of the criteria and channels through which patients transition from one care setting to another, including referral to specialized and advanced HFUs |
| CHFU.P.4 | Definitions of transitions within the process/health care pathway throughout the patient's clinical course |
| CHFU.P.5 | A clinical pathway for the structured follow-up of patients eligible for home care |
| CHFU.P.6 | A clinical pathway for the structured follow-up of patients under telemonitoring |
| CHFU.P.7 | Protocol for outpatient follow-up in the day hospital |
| CHFU.P.8 | Joint hospital-primary care planning process for hospital discharge and the transition from hospital to home |
| CHFU.P.9 | Structured follow-up process for the early detection of decompensation and optimization of therapy in the frail patient via a specific clinical pathway based on home intervention (case managers) |
| CHFU.P.10 | Specific process for patients with HF and advanced chronic disease at the end of life |
| CHFU.P.11 | Structured educational program in HF self-care for patients and caregivers that includes the skills needed to recognize early warning signs of worsening HF |
| Results | |
| HFR.1 | Risk-adjusted hospital mortality rate for HF (main diagnosis) |
| HFR.2 | Mortality rate at 30 days, 3 months, and 1 year |
| HFR.3 | Risk-adjusted rehospitalization rate (all-cause, CAD as main cause, and HF as main cause) |
| HFR.4 | Readmission rate at 30 days, 3 months, and 1 year |
| HFR.5 | Number of visits for HF |
| HFR.6 | Population rate of total stays/y |
| HFR.7 | Total population rate stays/y in patients older than 65 years |
| HFR.8 | Population rate of visits to emergency services for decompensated HF |
| HFR.9 | Population rate of visits to emergency services for decompensated HF in patients older than 65 years |
| Information system | |
| IS.1 | The cardiology unit and department should transfer information to the SEC registries (RECALCAR registry and others), state registries, and Spanish National Health System registries and should be incorporated into a benchmarking system of process and outcome indicators with other HFUs |
| IS.2 | The unit will participate in the registry of the Heart Failure Section: Heart Failure Long-term Registry, developed in collaboration with the ESC |
| IS.3 | The type of HF: HFrEF (systolic) or HFpEF (diastolic), should be identified in cardiology discharge reports |
CAD, coronary artery disease; CHFU, community heart failure unit; E&P, equipment and procedures; ECG, electrocardiogram; ESC, European Society of Cardiology; HF, heart failure; HFpEF, heart failure with preserved ejection fraction; HFU, heart failure unit; HFrEF, heart failure with reduced ejection fraction; HR, human resources; ICT, information and communications technology; IS, information systems; OPMS, organizational and process management structure; P, process; R, results; SEC, Spanish Society of Cardiology; SP, services portfolio.
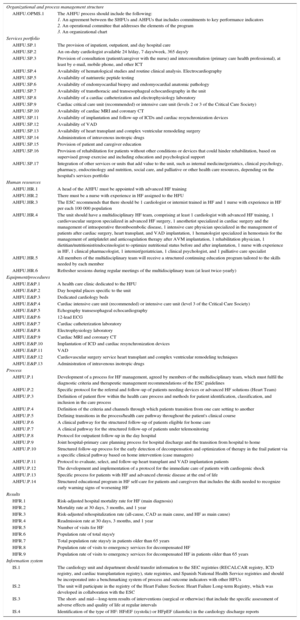
Standards for Specialized Heart Failure Units
| Organizational and process management structure | |
| SHFU.OPMS.1 | The SHFU process must include: 1. An agreement between the community HFUs, SHFUs, and advanced HFUs that includes commitments to key performance indicators 2. An operational committee that addresses the elements of the program 3. An organizational chart |
| Services portfolio | |
| SHFU.SP.1 | The provision of inpatient, outpatient, and day hospital care |
| SHFU.SP.2 | The presence of an on-duty cardiologist 24 h/day, 7 days/week, 365 days/y |
| SHFU.SP.3 | Provision of consultation (patient/caregiver with the nurse) and interconsultation (primary care health professional), at least by e-mail, mobile phone, and other ICT |
| SHFU.SP.4 | Availability of hematological studies and routine clinical analysis. Electrocardiography |
| SHFU.SP.5 | Availability of natriuretic peptide testing |
| SHFU.SP.6 | Availability (or referral protocol to the reference center) of endomyocardial biopsy and endomyocardial anatomic pathology |
| SHFU.SP.7 | Availability of transesophageal and transthoracic echocardiography |
| SHFU.SP.8 | Availability of a cardiac catheterization and electrophysiology laboratory |
| SHFU.SP.9 | Cardiac critical care unit (recommended) or intensive care unit (levels 2 or 3 of the Critical Care Society) |
| SHFU.SP.10 | Availability of cardiac MRI and coronary CT |
| SHFU.SP.11 | Administration of intravenous inotropic drugs |
| SHFU.SP.12 | Availability of the implantation and follow-up of ICD resynchronization devices |
| SHFU.SP.13 | Provision of patient and caregiver education |
| SHFU.SP.14 | Provision of rehabilitation for patients without other conditions or devices that could hinder rehabilitation, based on supervised group exercise and including education and psychological support |
| SHFU.SP.15 | Pharmacy, geriatric/internal medicine, clinical psychology, and nutrition services, and palliative care resources in the hospital or referral hospital |
| Human resources | |
| SHFU.HR.1 | A head of the HFU must be appointed with advanced HF training |
| SHFU.HR.2 | There must be a nurse with experience in HF assigned to the HFU |
| SHFU.HR.3 | The ESC recommends that there should be 1 cardiologist with HF training or 1 nurse with experience in HF per each 100 000 population. |
| SHFU.HR.4 | These units should have a multidisciplinary HF care team comprising at least 1 cardiologist with advanced HF training, 1 internist with advanced HF training, 1 representative of the physicians in the primary care teams within the hospital's catchment area, 1 nurse with experience in HF, 1 geriatrician/internist, 1 clinical psychologist, 1 endocrine/nutrition specialist, and 1 palliative care specialist. It is recommended that a clinical pharmacologist should be included in the team |
| SHFU.HR.5 | All members of the multidisciplinary team will receive a structured continuing education program tailored to the skills needed by each member |
| SHFU.HR.6 | Refresher sessions during regular meetings of the multidisciplinary team (at least twice-yearly) |
| Equipment/procedures | |
| SHFU.E&P.1 | A health care clinic dedicated to the HFU |
| SHFU.E&P.2 | Day hospital places specific to the unit |
| SHFU.E&P.3 | Dedicated cardiology beds |
| SHFU.E&P.4 | Cardiac critical care unit (recommended) or intensive care unit (levels 2 or 3 of the Critical Care Society) |
| SHFU.E&P.5 | Availability of ultrasound /transesophageal echocardiography |
| SHFU.E&P.6 | 12-lead ECG |
| SHFU.E&P.7 | Cardiac catheterization laboratory |
| SHFU.E&P.8 | Electrophysiology laboratory |
| SHFU.E&P.9 | Cardiac MRI and coronary CT |
| SHFU.E&P.10 | Implantation of ICD and cardiac resynchronization devices |
| Process | |
| SHFU.P.1 | Development of a care process for handling the HF, agreed by members of the multidisciplinary team, which must meet the diagnostic criteria and therapeutic management recommendations of the ESC guidelines |
| SHFU.P.2 | Specific protocol for the referral and follow-up of patients needing devices or advanced HF solutions (Heart Team) |
| SHFU.P.3 | Definition of patient flow within the health care process and of the methods for patient identification, classification, and inclusion in the care process |
| SHFU.P.4 | Definition of the criteria and channels through which patients transition from one care setting to another, including referral to advanced HFUs |
| SHFU.P.5 | Defining transitions in the process/health care pathway throughout the patient's clinical course |
| SHFU.P.6 | A clinical pathway for the structured follow-up of patients eligible for home care |
| SHFU.P.7 | A clinical pathway for the structured follow-up of patients under telemonitoring |
| SHFU.P.8 | Protocol for outpatient follow-up in the day hospital |
| SHFU.P.9 | Joint hospital-primary care planning process for hospital discharge and the transition from hospital to home |
| SHFU.P.10 | Structured follow-up process for the early detection of decompensation and optimization of therapy in the frail patient via a specific clinical pathway based on home intervention (case managers) |
| SHFU.P.11 | Specific process for patients with HF and advanced chronic disease at the end of life |
| SHFU.P.12 | Structured educational program in HF self-care for patients and caregivers that includes the skills needed to recognize early warning signs of worsening HF |
| Results | |
| HFR.1 | Risk-adjusted hospital mortality rate for HF (main diagnosis) |
| HFR.2 | Mortality rate at 30 days, 3 months, and 1 year |
| HFR.3 | Risk-adjusted rehospitalization rate (all-cause, CAD as main cause, and HF as main cause) |
| HFR.4 | Readmission rate at 30 days, 3 months, and 1 year |
| HFR.5 | Number of visits for HF |
| HFR.6 | Population rate of total stays/y |
| HFR.7 | Population rate of stays/y in patients older than 65 years |
| HFR.8 | Population rate of visits to emergency services for decompensated HF |
| HFR.9 | Population rate of visits to emergency services for decompensated HF in patients older than 65 years |
| Information system | |
| IS.1 | The cardiology unit and department should transfer information to the SEC registries (RECALCAR registry and ICD registry), state registries, and Spanish National Health System registries and should be incorporated into a benchmarking system of process and outcome indicators with other HFUs |
| IS.2 | The unit will participate in the registry of the Heart Failure Section: Heart Failure Long-term Registry, which was developed in collaboration with the ESC |
| IS.3 | Identification of the type of HF: HFrEF |
| IS.4 | Identification of the type of HF: HFrEF (systolic) or HFpEF (diastolic) in the cardiology discharge reports |
CAD, coronary artery disease; CT, computed tomography; E&P, equipment and procedures; ECG, electrocardiogram; ESC, European Society of Cardiology; HF, heart failure; HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; HFU, heart failure unit; HR, human resources; ICD, implantable cardioverter defibrillator; ICT, information and communications technology; IS, information systems; MRI, magnetic resonance imaging; OPMS, organizational and process management structure; P, process; R, results; SEC, Spanish Society of Cardiology; SHFU, specialized heart failure unit; SP, services portfolio.
Standards of Advanced Heart Failure Units
| Organizational and process management structure | |
| AHFU.OPMS.1 | The AHFU process should include the following: 1. An agreement between the SHFUs and AHFUs that includes commitments to key performance indicators 2. An operational committee that addresses the elements of the program 3. An organizational chart |
| Services portfolio | |
| AHFU.SP.1 | The provision of inpatient, outpatient, and day hospital care |
| AHFU.SP.2 | An on-duty cardiologist available 24 h/day, 7 days/week, 365 days/y |
| AHFU.SP.3 | Provision of consultation (patient/caregiver with the nurse) and interconsultation (primary care health professional), at least by e-mail, mobile phone, and other ICT |
| AHFU.SP.4 | Availability of hematological studies and routine clinical analysis. Electrocardiography |
| AHFU.SP.5 | Availability of natriuretic peptide testing |
| AHFU.SP.6 | Availability of endomyocardial biopsy and endomyocardial anatomic pathology |
| AHFU.SP.7 | Availability of transthoracic and transesophageal echocardiography in the unit |
| AHFU.SP.8 | Availability of a cardiac catheterization and electrophysiology laboratory |
| AHFU.SP.9 | Cardiac critical care unit (recommended) or intensive care unit (levels 2 or 3 of the Critical Care Society) |
| AHFU.SP.10 | Availability of cardiac MRI and coronary CT |
| AHFU.SP.11 | Availability of implantation and follow-up of ICDs and cardiac resynchronization devices |
| AHFU.SP.12 | Availability of VAD |
| AHFU.SP.13 | Availability of heart transplant and complex ventricular remodeling surgery |
| AHFU.SP.14 | Administration of intravenous inotropic drugs |
| AHFU.SP.15 | Provision of patient and caregiver education |
| AHFU.SP.16 | Provision of rehabilitation for patients without other conditions or devices that could hinder rehabilitation, based on supervised group exercise and including education and psychological support |
| AHFU.SP.17 | Integration of other services or units that add value to the unit, such as internal medicine/geriatrics, clinical psychology, pharmacy, endocrinology and nutrition, social care, and palliative or other health care resources, depending on the hospital's services portfolio |
| Human resources | |
| AHFU.HR.1 | A head of the AHFU must be appointed with advanced HF training |
| AHFU.HR.2 | There must be a nurse with experience in HF assigned to the HFU |
| AHFU.HR.3 | The ESC recommends that there should be 1 cardiologist or internist trained in HF and 1 nurse with experience in HF per each 100 000 population |
| AHFU.HR.4 | The unit should have a multidisciplinary HF team, comprising at least 1 cardiologist with advanced HF training, 1 cardiovascular surgeon specialized in advanced HF surgery, 1 anesthetist specialized in cardiac surgery and the management of intraoperative thromboembolic disease, 1 intensive care physician specialized in the management of patients after cardiac surgery, heart transplant, and VAD implantation, 1 hematologist specialized in hemostasis for the management of antiplatelet and anticoagulation therapy after AVM implantation, 1 rehabilitation physician, 1 dietitian/nutritionist/endocrinologist to optimize nutritional status before and after implantation, 1 nurse with experience in HF, 1 clinical pharmacologist, 1 internist/geriatrician, 1 clinical psychologist, and 1 palliative care specialist |
| AHFU.HR.5 | All members of the multidisciplinary team will receive a structured continuing education program tailored to the skills needed by each member |
| AHFU.HR.6 | Refresher sessions during regular meetings of the multidisciplinary team (at least twice-yearly) |
| Equipment/procedures | |
| AHFU.E&P.1 | A health care clinic dedicated to the HFU |
| AHFU.E&P.2 | Day hospital places specific to the unit |
| AHFU.E&P.3 | Dedicated cardiology beds |
| AHFU.E&P.4 | Cardiac intensive care unit (recommended) or intensive care unit (level 3 of the Critical Care Society) |
| AHFU.E&P.5 | Echography transesophageal echocardiography |
| AHFU.E&P.6 | 12-lead ECG |
| AHFU.E&P.7 | Cardiac catheterization laboratory |
| AHFU.E&P.8 | Electrophysiology laboratory |
| AHFU.E&P.9 | Cardiac MRI and coronary CT |
| AHFU.E&P.10 | Implantation of ICD and cardiac resynchronization devices |
| AHFU.E&P.11 | VAD |
| AHFU.E&P.12 | Cardiovascular surgery service heart transplant and complex ventricular remodeling techniques |
| AHFU.E&P.13 | Administration of intravenous inotropic drugs |
| Process | |
| AHFU.P.1 | Development of a process for HF management, agreed by members of the multidisciplinary team, which must fulfil the diagnostic criteria and therapeutic management recommendations of the ESC guidelines |
| AHFU.P.2 | Specific protocol for the referral and follow-up of patients needing devices or advanced HF solutions (Heart Team) |
| AHFU.P.3 | Definition of patient flow within the health care process and methods for patient identification, classification, and inclusion in the care process |
| AHFU.P.4 | Definition of the criteria and channels through which patients transition from one care setting to another |
| AHFU.P.5 | Defining transitions in the process/health care pathway throughout the patient's clinical course |
| AHFU.P.6 | A clinical pathway for the structured follow-up of patients eligible for home care |
| AHFU.P.7 | A clinical pathway for the structured follow-up of patients under telemonitoring |
| AHFU.P.8 | Protocol for outpatient follow-up in the day hospital |
| AHFU.P.9 | Joint hospital-primary care planning process for hospital discharge and the transition from hospital to home |
| AHFU.P.10 | Structured follow-up process for the early detection of decompensation and optimization of therapy in the frail patient via a specific clinical pathway based on home intervention (case managers) |
| AHFU.P.11 | Protocol to evaluate, select, and follow-up heart transplant and VAD implantation patients |
| AHFU.P.12 | The development and implementation of a protocol for the immediate care of patients with cardiogenic shock |
| AHFU.P.13 | Specific process for patients with HF and advanced chronic disease at the end of life |
| AHFU.P.14 | Structured educational program in HF self-care for patients and caregivers that includes the skills needed to recognize early warning signs of worsening HF |
| Results | |
| HFR.1 | Risk-adjusted hospital mortality rate for HF (main diagnosis) |
| HFR.2 | Mortality rate at 30 days, 3 months, and 1 year |
| HFR.3 | Risk-adjusted rehospitalization rate (all-cause, CAD as main cause, and HF as main cause) |
| HFR.4 | Readmission rate at 30 days, 3 months, and 1 year |
| HFR.5 | Number of visits for HF |
| HFR.6 | Population rate of total stays/y |
| HFR.7 | Total population rate stays/y in patients older than 65 years |
| HFR.8 | Population rate of visits to emergency services for decompensated HF |
| HFR.9 | Population rate of visits to emergency services for decompensated HF in patients older than 65 years |
| Information system | |
| IS.1 | The cardiology unit and department should transfer information to the SEC registries (RECALCAR registry, ICD registry, and cardiac transplantation registry), state registries, and Spanish National Health Service registries and should be incorporated into a benchmarking system of process and outcome indicators with other HFUs |
| IS.2 | The unit will participate in the registry of the Heart Failure Section: Heart Failure Long-term Registry, which was developed in collaboration with the ESC |
| IS.3 | The short- and mid—long-term results of interventions (surgical or otherwise) that include the specific assessment of adverse effects and quality of life at regular intervals |
| IS.4 | Identification of the type of HF: HFrEF (systolic) or HFpEF (diastolic) in the cardiology discharge reports |
AHFU, advanced heart failure unit; CAD, coronary artery disease; CT, computed tomography; E&P, equipment and procedures; ECG, electrocardiogram; ESC, European Society of Cardiology; HF, heart failure; HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; HFU, heart failure unit; HR, human resources; ICD, implantable cardioverter defibrillator; ICT, information and communications technology; IS, information systems; MRI, magnetic resonance imaging; OPMS, organizational and process management structure; P, process; SP, services portfolio; R, results; SEC, Spanish Society of Cardiology; SHFU, specialized heart failure unit; VAD, ventricular assist device.
Based on their level of complexity (services portfolio), the SEC will classify the HFUs into the following types of unit:
- •
Community heart failure unit (CHFU)
- •
Specialized heart failure unit (SHFU)
- •
Advanced heart failure unit (AHFU)
Table 1, Table 2, and Table 3 show the characteristics and standards of these types of units.
Heart Failure Units StandardsThe standards selected for each type of unit cover the following domains:
- •
Organizational and process management structure
- •
Services portfolio
- •
Human resources
- •
Equipment/procedures
- •
Care process
- •
Information system
- •
Performance indicators
The main aim of these units is the development of a nurse-led multidisciplinary program, which amalgamates the care processes and services in primary and hospital care for HF patients through the creation of a hospital-based multidisciplinary HFU, whose most important organizational and management elements have been described by Abel Diéguez et al.64 and Comín-Colet et al.36
Organizational and Process Management StructureA common standard for the 3 types of HFU is that they have a care process management structure that must include at least the following: a) an agreement between the stakeholders and institutions based on a regionally-based care agreement that includes commitments to key performance indicators; b) an operational committee that addresses the elements of the program, and c) an organizational chart. The program must necessarily integrate primary care, especially in the case of CHFUs and SHFUs.
Services PortfolioThe services portfolio of a CHFU should fulfil the basic requirements to ensure the implementation of the program (Table 1). It is important to integrate within a single services portfolio all the resources dedicated to the HF management process, whether hospital-based or provided by primary care centers. It is recommended that primary care professionals integrated within the program can order a natriuretic peptide test if they suspect HF.60
Human ResourcesA head of the CHFU should be formally appointed. In hospitals in areas with less than 250 000 population, the multidisciplinary team may be led by an internist with advanced HF training. It is recommended that the person in charge of training should have completed a minimum of 1-year's advanced HF training (European curriculum)65 or ACC level 1.66The CHFU should be assigned a nurse with experience in HF12,67–71 (equivalent to a specialist HF nurse in other countries) who, in hospitals in areas with less than 250 000 inhabitants, can deal with noncardiological processes. The CHFU should have a multidisciplinary HF care team comprising at least 1 specialist HF cardiologist and/or internist trained in HF, 1 representative of the physicians in the primary care teams within the hospital's catchment area, and 1 nurse with experience in HF. The ESC recommends that there should be 1 cardiologist or internist trained in HF and 1 nurse with experience in HF per each 100 000 population.47
Equipment/proceduresAny acute care hospital within the Spanish National Health System probably has the equipment needed to develop a systematic HF management program coordinated by a CHFU.
Care ProcessThe development of a clinical pathway or care route for the integrated management of HF, agreed by the multidisciplinary team, is the core element characterizing CHFUs. This process should incorporate the diagnostic criteria and therapeutic management recommendations of the ESC guidelines, which have been endorsed by the SEC.55 The channels of interaction between primary care and the CHFU are the minimum standards for CHFU accreditation36:
- •
Definition of patient flow within the care process/health care pathway and of the methods of their identification, classification, and inclusion in the health care process.
- •
Definition of the criteria and channels through which patients transition from one care setting to another, including referral to the SHFU and AHFU.
- •
Definition of the transitions within the care process/health care pathway throughout the patient's clinical course.61,67
- •
The development of a clinical pathway for the structured follow-up of patients eligible for home care.13,19,21,26,34
- •
The development of a clinical pathway for the structured follow-up of patients under telemonitoring.
- •
Protocol for outpatient follow-up in the day hospital.
- •
Joint hospital-primary care planning process for hospital discharge and the transition from hospital to home.61,67
- •
Structured follow-up process for the early detection of decompensations and optimization of therapy in the frail patient via a specific clinical pathway based on home intervention (case managers).67,69
- •
Specific process for patients with HF and advanced chronic disease at the end of life.69
- •
Structured educational program in HF self-care for patients and caregivers that includes the skills needed to recognize early warning signs of worsening HF.
An essential element of the SEC-Excellence project is the development of information systems for the creation of registries72 that will enhance understanding of the cardiology care processes in Spain. The standards chosen for this domain are:
- •
The CHFU and cardiology department should transfer information to the SEC registries (RECALCAR registry and others), state registries, and Spanish National Health System and should be incorporated into a benchmarking system of process and outcome indicators with other HFUs.
- •
It is recommended that the CHFU participate in the in the registry of the Heart Failure Section (Heart Failure Long-term Registry), which was developed in collaboration with the ESC.73
- •
The type of HF (HF with reduced ejection fraction [systolic] or preserved ejection fraction [diastolic]), should be identified in cardiology discharge reports.
Outcomes research is receiving increasing attention, especially in relation to the delivery of services,74–76 and is used to compare health services77 and performance between countries. Outcome indicators related to mortality and readmissions are among those most commonly used, and include risk adjustment methods to allow comparison of services. A key aspect of the SEC-Excellence project is to obtain outcome indicators for their comparison with the information available on patient management (information systems). The indicators selected for the CHFU are:
- •
Risk-adjusted hospital mortality rate for HF (main diagnosis).
- •
Mortality rate at 30 days, 3 months, and 1 year.
- •
Risk-adjusted rehospitalization rate (all-cause, coronary artery disease as main cause, and HF as main cause).
- •
Readmission rate at 30 days, 3 months, and 1 year.
- •
Number of visits for HF.
- •
Population rate of total stays/year.
- •
Total population rate stays/year in patients older than 65 years.
- •
Population rate of visits to emergency services for decompensated HF.
- •
Population rate of visits to emergency services for decompensated HF in patients older than 65 years.
The aim is for the SEC to provide the cardiology services, cardiology units, and CHFUs that participate in its registries with a benchmarking mechanism so that this information can be incorporated into a continuous improvement program in each unit and service.
Specialized Heart Failure UnitsThese units should be able to develop a comprehensive HF management program,47 excluding techniques which, due to their complexity, safety, and efficiency, require an AHFU. This section refers only to those aspects that differentiate the SHFU from the CHFU.
Services PortfolioThe services portfolio of an SHFU must ensure the near-complete implementation of the program (Table 2). Most SHFUs serve areas with more than 250 000 population. In these SHFUs, the cardiology service or unit should have dedicated beds and an on-duty cardiologist, and the SHFU should have day hospital places dedicated to the unit. The services portfolio of the SHFUs should also include: cardiac magnetic resonance imaging and coronary computed tomography, the ability to administer intravenous inotropic drugs, and the ability to place implantable cardioverter-defibrillators and resynchronization devices and provide follow-up for these patients.
Human ResourcesThe head of the AHFU should be a cardiologist and should be formally appointed. It is recommended that the head of training should have completed a minimum of 2-years’ advanced HF training (European curriculum)65 or ACC level 3.66 The SHFU should have a nurse with experience in HF assigned to the unit. The proportion of cardiologists trained in HF and nurses with experience in HF is the same as that for CHFUs.
Equipment/proceduresAn SHFU must have the equipment needed to deliver its services portfolio, which includes a consulting office and day hospital places specific to the unit, conventional hospital beds dedicated to cardiology, a cardiac intensive care unit (recommended) or intensive care unit, ultrasound and transesophageal echocardiography in the cardiology service or unit, and a cardiac catheterization, electrophysiology, cardiac magnetic resonance imaging, and coronary computed tomography laboratory. The SHFU must be able to implant implantable cardioverter-defibrillators and cardiac resynchronization devices.
Care ProcessThe most relevant requirements of this domain are the development of a HF management process, agreed by members of the multidisciplinary team, which must meet the diagnostic criteria and therapeutic management recommendations of the ESC guidelines,55 and the development of a specific protocol for the referral and follow-up of HF patients needing devices or advanced solutions (Heart Team), which is the most specific standard for SHFUs. The remaining standards are the same as those for processes in CHFUs.
Information SystemThe standards of this domain overlap with those of CHFUs. In addition to these standards, the cardiology units linked to the SHFU should participate in the registries of the Cardiac Catheterization and Interventional Cardiology Section and the Electrophysiology and Arrhythmias Section (ablation and implantable cardioverter-defibrillator).
Outcome IndicatorsThe outcome indicators are similar to those of CHFUs.
Advanced Heart Failure UnitsThese units should be able to develop a comprehensive HF management program,47 including techniques which, due to their complexity, safety, and efficiency, require an AHFU. This section addresses only the differences between AHFUs and the SHFUs.
Services PortfolioThe AHFU services portfolio AHFU must ensure the complete implementation of the program (Table 3). In the AHFU, the cardiology service or unit should have dedicated beds, an on-duty cardiologist, and the AHFU should have day hospital places dedicated to the unit. In addition to the SHFU services portfolio, the AHFU should also include endomyocardial biopsy, ventricular assist devices, heart transplant, and complex ventricular remodeling surgery.
Human ResourcesThe head of the AHFU should be a cardiologist and should be formally appointed. It is recommended that the head of training should have completed a minimum of 3-years’ advanced HF training (European curriculum)65 or the ACC level 3.66
Equipment/proceduresThe AHFA must have the equipment needed to deliver its services portfolio, including endomyocardial biopsy and ventricular assist devices. The service or cardiology unit linked to the AHFU should have a cardiac catheterization, interventional cardiology, and electrophysiology laboratory. The hospital housing the AHFU must have a cardiovascular surgery service.
Care ProcessThe most relevant requirement of this domain is the development of an HF care management process, agreed by the members of the multidisciplinary team, which must meet the diagnostic criteria and therapeutic management recommendations of the ESC guidelines,55 and the development of a specific protocol for the indication and follow-up of patients needing devices or advanced HF solutions (Heart Team), which includes a protocol to evaluate, select, and follow-up heart transplant recipients and device implantation patients, and a protocol for the immediate care of patients with cardiogenic shock.
Information SystemThe standards of this domain are similar to those of the SHFU. Participation in the Spanish Heart Transplantation Registry and the Spanish Circulatory Assist Device Registry.
Outcome IndicatorsThe outcome indicators are similar to those of the other HFUs.
CONCLUSIONSHeart failure is a complex process. For affected patients to receive appropriate care, change is required in the organization of HF care. The organization of HF care must be based on a coordinated system of HFUs with different levels of complexity (community-based, specialized, and advanced), which meet the quality standards based on the available evidence as presented in this article.
CONFLICTS OF INTERESTNone declared.