Survivors of out-of-hospital cardiac arrest constitute an increasing patient population in cardiac intensive care units. Our aim was to characterize these patients and determine their vital and functional prognosis in accordance with the latest evidence.
MethodsA multicenter, prospective register was constructed with information from patients admitted to 5 cardiac intensive care units from January 2010 through January 2012 with a diagnosis of resuscitated out-of-hospital cardiac arrest. The information included clinical status, cardiac arrest characteristics, in-hospital course, and vital and neurologic status at discharge and at 6 months.
ResultsA total of 204 patients were included. In 64% of cases, a first shockable rhythm was identified. The time to return of spontaneous circulation was 29 (18) min. An etiologic diagnosis was made in 86% of patients; 44% were discharged with no neurologic sequelae; 40% died in the hospital. At 6 months, 79% of survivors at discharge were still alive and neurologically intact with minimal sequelae. Short resuscitation time, first recorded rhythm, pH on admission >7.1, absence of shock, and use of hypothermia were the independent variables associated with a good neurologic prognosis.
ConclusionsHalf the patients who recovered from out-of-hospital cardiac arrest had good neurologic prognosis at discharge, and 79% of survivors were alive and neurologically intact after 6 months of follow-up.
Keywords
Approximately 24 000 to 50 000 out-of-hospital cardiac arrests (OHCAs) are estimated to take place every year in Spain,1 of which 90% of the OHCAs occurring in adults could be sudden cardiac deaths.2 In fact, sudden death is the most common form of death among patients with ischemic heart disease, which is the first manifestation of the disease in up to 20% of cases.3
Because sudden cardiac death is closely related to coronary disease, survivors are admitted to cardiac intensive care units (CICUs). Although relatively few patients are admitted for sudden death, the health care impact of these patients is extremely high.4 Cardiologic, in particular neurologic, complications can lead to long hospital stays and a poor vital and functional prognosis.5
The results vary considerably in terms of survival and functional status at hospital discharge.5–9 The difficulty of early neurologic stratification and the poor outcomes until recent times have contributed to worsening patient prognosis by encouraging the phenomenon known as “self-fulfilling prophecy.”7
In our setting, there is a paucity of OHCA data once patients are admitted to the hospital. The current published series are all single-site,4,8 retrospective,8 based on the rate of return of spontaneous circulation,1 or include in-hospital cardiac arrest.9 Moreover, it is unclear how much impact on survival and neurologic prognosis has been obtained from new cardiopulmonary resuscitation (CPR) algorithms,10 widespread use of an automated external defibrillator (AED), postresuscitation care protocols,11 therapeutic hypothermia,12 and greater availability of coronary interventional procedures.13 The purpose of this study is to describe the problem, characterize the patients and their management, and determine the short- and medium-term neurologic prognosis in view of the latest evidence.
METHODSPatientsThe study consisted of a prospective register from 1 January 2010 to 31 January 2012 and included all patients who survived an OHCA and were admitted to CICUs at 5 teaching hospitals in Catalonia (Hospital Universitario de Bellvitge, Hospital Universitario Vall d’Hebron, Hospital Universitario Germans Trias i Pujol, Hospital Universitario de la Santa Creu i Sant Pau, and Hospital Universitario Josep Trueta). Patients with an unidentified cardiologic cause or incomplete information on the cardiac arrest were excluded. All cardiac arrest-related data (location of arrest, first recorded rhythm, resuscitation times and personnel, use of AED and/or nonautomated defibrillator, and neurologic assessment by Glasgow scale) were collected from the emergency medical services. Shockable rhythm was considered to exist when evidenced by electrocardiography or by defibrillation in the case of AED use. Likewise, both family and witnesses were asked about the circumstances of the cardiac arrest and the times elapsed.
During the patient's hospital stay, the following were recorded: cardiologic history, first electrocardiogram and pH, vital signs, percentage of orotracheal intubation/tracheotomy, additional test results, days of intubation and hospital stay, neurologic status, and mortality. Urgent coronary reperfusion times and procedures and affected territories were collected for patients with acute coronary syndrome with persistent ST segment elevation, and the culprit artery of the event for patients who underwent coronary angiography.
Treatment was at the discretion of the attending physician, with the ILCOR (International Liaison Committee on Resuscitation) consensus document available at all sites.14 Therapeutic hypothermia was used in all patients who were comatose after cardiac arrest secondary to ventricular fibrillation or recorded rhythm and who met none of the exclusion criteria (nonhypoxic coma, pregnancy, refractory hypotension or hypoxemia, life expectancy <6 months, or uncontrollable active bleeding). The technique was applied according to availability at the hospital and at the discretion of the attending physician. In-hospital mortality was recorded.
Neurologic AssessmentNeurologic status at discharge was assessed using the Glasgow-Pittsburgh categories14: cerebral performance category (CPC) 1 (no sequelae), CPC 2 (mild disability, independent, no institutionalization required), CPC 3 (severe disability, dependent, institutionalization required), CPC 4 (persistent vegetative state), and CPC 5 (death). As in previous studies,15 the first 2 were considered good neurologic outcomes and the last 3, poor neurologic outcomes or death.
Follow-upFollow-up was performed at 6 months via a medical visit or phone interview. Vital status and neurologic status were determined by the Glasgow-Pittsburgh scale.
Data CentralizationAll data were entered cooperatively and synchronously using a web-based platform (Zoho Creator®, Zoho Corporation Pvt, Ltd). Informed consent for data use was obtained, and data confidentiality was guaranteed in compliance with the Spanish Law on Data Protection.
Statistical AnalysisThe results are expressed as the mean (standard deviation) for continuous variables with a normal distribution, medians for continuous variables with a non-Gaussian distribution, and percentages for categorical variables. The characteristics of patients with good and poor prognoses were compared using the χ2 test or Fisher exact test for categorical variables. Quantitative variables were analyzed by the Student t test in the case of normal distribution, or Mann-Whitney U-test in the case of a non-normal distribution. To assess the independent effect of various predictors collected at admission on the incidence of good neurologic prognosis at discharge, a logistic regression model was constructed including the variables that showed P<.15 (0.10-0.20) in the univariate analysis, as well as those previously reported to provide prognostic information.16 The variables were entered in the model as a block. Significance level was set at P<.05. All statistical analyses were performed using SPSS 15.0 for Windows (SPSS Inc.; Chicago, Illinois, United States).
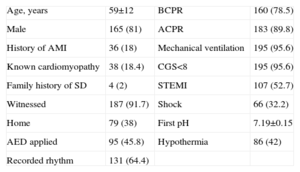
RESULTSBetween 1 January 2010 and 31 January 2012, the 5 participating CICUs recorded 204 patients with resuscitated OHCA. The general characteristics of the sample are summarized in Table 1.
General Characteristics of the Sample and the Cardiac Chain of Survival
| Age, years | 59±12 | BCPR | 160 (78.5) |
| Male | 165 (81) | ACPR | 183 (89.8) |
| History of AMI | 36 (18) | Mechanical ventilation | 195 (95.6) |
| Known cardiomyopathy | 38 (18.4) | CGS<8 | 195 (95.6) |
| Family history of SD | 4 (2) | STEMI | 107 (52.7) |
| Witnessed | 187 (91.7) | Shock | 66 (32.2) |
| Home | 79 (38) | First pH | 7.19±0.15 |
| AED applied | 95 (45.8) | Hypothermia | 86 (42) |
| Recorded rhythm | 131 (64.4) |
ACPR, advanced cardiopulmonary resuscitation; AED, automatic external defibrillator; BCPR, basic cardiopulmonary resuscitation; AMI, acute myocardial infarction; GCS, Glasgow coma scale; SD, sudden death; STEMI, ST-segment elevation acute myocardial infarction.
Data are expressed as no. (%) or mean±standard deviation.
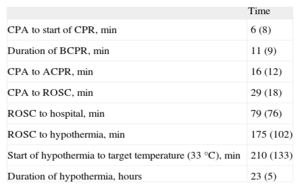
Although most (92%) cardiac arrests were witnessed, only 29% of bystanders began resuscitation maneuvers. Intervention times are described in Table 2. A total of 78.5% of patients received basic CPR. An AED was used as part of basic CPR in 46% of patients, but by a bystander in only 7% of cases.
Intervention Times
| Time | |
| CPA to start of CPR, min | 6 (8) |
| Duration of BCPR, min | 11 (9) |
| CPA to ACPR, min | 16 (12) |
| CPA to ROSC, min | 29 (18) |
| ROSC to hospital, min | 79 (76) |
| ROSC to hypothermia, min | 175 (102) |
| Start of hypothermia to target temperature (33°C), min | 210 (133) |
| Duration of hypothermia, hours | 23 (5) |
ACPR, advanced cardiopulmonary resuscitation; BCPR, basic cardiopulmonary resuscitation; CPA, cardiopulmonary arrest; CPR, cardiopulmonary resuscitation; ROSC, return of spontaneous circulation.
Data are expressed as mean (standard deviation).
Advanced CPR was performed in 89.8% of patients. In 64%, a first shockable rhythm was identified. Advanced CPR was performed by emergency medical services in 93% of patients and in a health setting in all others.
On arrival to the CICU, 95.6% of patients remained in spontaneous or pharmacologic coma, and 32% presented clinical evidence of shock. Therapeutic hypothermia was applied to 86/195 (44%) patients who were comatose on arrival to the CICU.
Etiology of Cardiac Arrest and Hospital OutcomeAdditional tests were carried out to identify the etiologic diagnosis: routine echocardiography in all patients, coronary angiography in 133 (64%), flecainide testing in 5 (all negative), electrophysiologic study in 4 (1 patient was identified and underwent ablation in an accessory pathway; in another, ventricular tachycardia was induced; 2 were negative), and lastly only 1 patient underwent cardiac magnetic resonance, which was inconclusive.
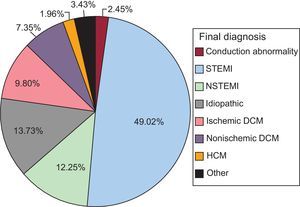
The most common reason for OHCA was some form of ischemic heart disease (71.1%): dilated ischemic cardiomyopathy, non-ST-segment elevation acute myocardial infarction, and most predominantly, in 49% of all patients, ST-segment elevation acute myocardial infarction (STEMI). The cause was considered to be nonischemic dilated cardiomyopathy in 7.4% of cases and hypertrophic cardiomyopathy in 2%. One case of Wolf-Parkinson-White syndrome was diagnosed, 1 acute aortic syndrome, and 1 vasospasm (0.5% each). In 28 (13.7%) patients, no OHCA etiology was identified. The final diagnoses are shown in Figure 1.
In patients without STEMI, 30.2% had a known cardiomyopathy and only 1 had a poorly functioning implantable cardioverter-defibrillator. The incidence of a family history of sudden death was very low (4%).
Reperfusion treatment was given to 89% of patients with STEMI (primary percutaneous coronary intervention in 79.6% and thrombolysis in 9.3%), with a symptoms-to-balloon time of 178 (5) min. The most common STEMI site was anterior (56.4%), and the anterior descending artery was the most commonly identified culprit artery (57.5%).
Patients had markers of complexity, such as a mean intubation time of 6 days, a tracheotomy rate of 17%, or a mean hospital stay of 24 days.
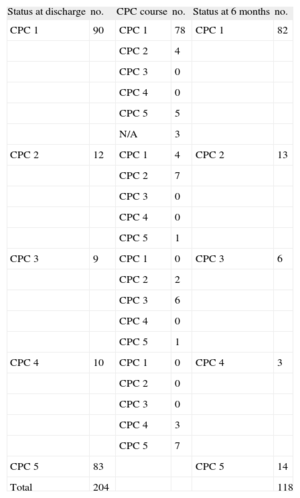
Survival and Neurologic OutcomeOf the 204 patients included in the register, 90 (44.1%) were discharged neurologically intact (CPC 1), 12 (5.8%) had mild neurologic deficits (CPC 2), 9 (4.4%) had serious neurologic sequelae that led to dependence (CPC 3), and 10 (5%) continued in a persistent vegetative state (CPC 4); in-hospital mortality was 40.7% (83 patients). The most common causes of death were neurologic complications (50.6%), followed by cardiogenic shock (18%) and infections (17%).
Of the 121 survivors, follow-up information was obtained from 118 (97.5%), with a mean follow-up of 270 days. At 6 months, 82 (69.5%) were still in CPC 1; 13 (11%) in CPC 2; 6 (5%) in CPC 3, and 3 (2.5%) in CPC 4; 14 (11.9%) patients died during follow-up. Of these 14, the cause of death was known in 8 (3, neurologic deterioration; 2, heart failure; 2, recurrence of cardiac arrest; 1, infectious complication). A total of 19 automated defibrillators were implanted. The CPC distribution at discharge and at 6 months and the clinical course are described in Table 3.
Neurologic Outcomes
| Status at discharge | no. | CPC course | no. | Status at 6 months | no. |
| CPC 1 | 90 | CPC 1 | 78 | CPC 1 | 82 |
| CPC 2 | 4 | ||||
| CPC 3 | 0 | ||||
| CPC 4 | 0 | ||||
| CPC 5 | 5 | ||||
| N/A | 3 | ||||
| CPC 2 | 12 | CPC 1 | 4 | CPC 2 | 13 |
| CPC 2 | 7 | ||||
| CPC 3 | 0 | ||||
| CPC 4 | 0 | ||||
| CPC 5 | 1 | ||||
| CPC 3 | 9 | CPC 1 | 0 | CPC 3 | 6 |
| CPC 2 | 2 | ||||
| CPC 3 | 6 | ||||
| CPC 4 | 0 | ||||
| CPC 5 | 1 | ||||
| CPC 4 | 10 | CPC 1 | 0 | CPC 4 | 3 |
| CPC 2 | 0 | ||||
| CPC 3 | 0 | ||||
| CPC 4 | 3 | ||||
| CPC 5 | 7 | ||||
| CPC 5 | 83 | CPC 5 | 14 | ||
| Total | 204 | 118 |
CPC, cerebral performance category; N/A, follow-up information not available.
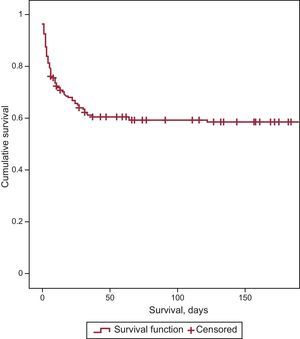
Among the 102 patients in CPC 1 or 2 at discharge, 93 (91%) remained in CPC 1 or CPC 2 at 6 months, whereas only 2 (10%) of the 19 patients in CPC 3 or CPC 4 at discharge improved to CPC 2. Mortality was 5.8% in CPC 1 and CPC 2 patients, and 42% in the CPC 3 and CPC 4 group. Most patient deaths occurred during the first month, and vital prognosis was typically good afterwards. In summary, after follow-up, 95/204 (46.5%) were alive and neurologically intact or had few sequelae and 97/204 (47.5%) had died.
No significant differences were found in CPC category between the different hospitals at discharge or during follow-up. Cumulative survival is shown in Figure 2.
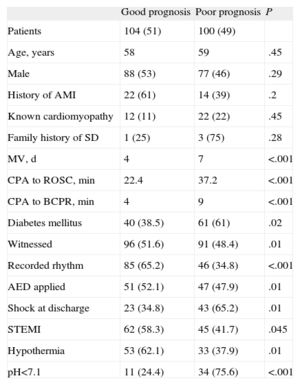
Predictors of Good PrognosisTo identify predictive factors of good vital and functional prognosis at discharge, the population was divided into 2 groups: good prognosis (CPC 1 and CPC 2) and poor prognosis (CPC 3 to CPC 5). A univariate analysis was performed, with the results listed in Table 4.
Prognostic Predictors. Univariate Analysis
| Good prognosis | Poor prognosis | P | |
| Patients | 104 (51) | 100 (49) | |
| Age, years | 58 | 59 | .45 |
| Male | 88 (53) | 77 (46) | .29 |
| History of AMI | 22 (61) | 14 (39) | .2 |
| Known cardiomyopathy | 12 (11) | 22 (22) | .45 |
| Family history of SD | 1 (25) | 3 (75) | .28 |
| MV, d | 4 | 7 | <.001 |
| CPA to ROSC, min | 22.4 | 37.2 | <.001 |
| CPA to BCPR, min | 4 | 9 | <.001 |
| Diabetes mellitus | 40 (38.5) | 61 (61) | .02 |
| Witnessed | 96 (51.6) | 91 (48.4) | .01 |
| Recorded rhythm | 85 (65.2) | 46 (34.8) | <.001 |
| AED applied | 51 (52.1) | 47 (47.9) | .01 |
| Shock at discharge | 23 (34.8) | 43 (65.2) | .01 |
| STEMI | 62 (58.3) | 45 (41.7) | .045 |
| Hypothermia | 53 (62.1) | 33 (37.9) | .01 |
| pH<7.1 | 11 (24.4) | 34 (75.6) | <.001 |
AED, automatic external defibrillator; AMI, myocardial infarction; BCPR, basic cardiopulmonary resuscitation; CPA, cardiopulmonary arrest; MV, mechanical ventilation; ROSC, return of spontaneous circulation; SD, sudden death; STEMI, ST-segment elevation acute myocardial infarction.
Data are presented as no. (%).
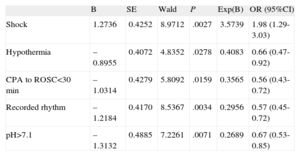
Based on the available variables at admission with P <.15 in the univariate analysis, a multivariate model was constructed, showing that first recorded rhythm, time to return of spontaneous circulation<30 min, pH on admission n>7, absence of shock, and use of therapeutic hypothermia were the independent factors associated with a good neurologic prognosis (Table 5).
Prognostic Predictors. Multivariate Analysis (n=126)
| B | SE | Wald | P | Exp(B) | OR (95%CI) | |
| Shock | 1.2736 | 0.4252 | 8.9712 | .0027 | 3.5739 | 1.98 (1.29-3.03) |
| Hypothermia | –0.8955 | 0.4072 | 4.8352 | .0278 | 0.4083 | 0.66 (0.47-0.92) |
| CPA to ROSC<30 min | –1.0314 | 0.4279 | 5.8092 | .0159 | 0.3565 | 0.56 (0.43-0.72) |
| Recorded rhythm | –1.2184 | 0.4170 | 8.5367 | .0034 | 0.2956 | 0.57 (0.45-0.72) |
| pH>7.1 | –1.3132 | 0.4885 | 7.2261 | .0071 | 0.2689 | 0.67 (0.53-0.85) |
95%CI: 95% confidence interval; CPA, cardiopulmonary arrest; OR, odds ratio; ROSC, return of spontaneous circulation; SE, standard error.
This article reports for the first time in Spain on the clinical characteristics and prognosis of a multicenter prospective cohort of survivors of OHCA admitted to CICU. Despite the severity of these patients at hospital admission, 50% of patients who recovered from OHCA had a good neurologic prognosis at discharge. At 6 months, 79% of survivors were still alive and neurologically intact with minimal sequelae. These promising results contrast with those obtained by other groups in a similar population.
In the largest series published to date in Spain, with characteristics similar to those of the present study, 26% to 35% of survivors were free of significant neurologic sequelae at discharge.4,8,9 Certain factors could at least partially explain the good outcomes: improvement in the cardiac chain of survival, and use of moderate hypothermia, coronary reperfusion treatment, and postcardiac arrest care protocols in the CICU.
First, communities with early defibrillation programs have been shown to have higher survival rates.17 Compared to the series cited, our population had shorter response times and more widespread use of AED by basic emergency teams, which have been associated with better prognoses.18 Emergency system response time and AED use were not independent predictors of good prognosis, but did affect total arrest time and resuscitation duration and quality, summarized as initial pH,19 which has been shown to be an independent predictor of good prognosis.
Two aspects related to the cardiac chain of survival offer opportunities for improvement. Firstly, the low rate at which witnesses began maneuvers and low rate of AED use by a bystander, which could improve with CPR training, access to public defibrillation, or systems based on phone aid.20 Secondly, the long transport time to hospital after return of spontaneous circulation, time in which measures could be taken to control the postcardiac arrest syndrome21 and shorten the delay in reaching the hospital.
Another factor that could have contributed to the good outcomes is the frequent use of hypothermia. In our series, 44% of patients in coma received moderate hypothermia, a treatment shown to improve vital and functional prognosis of OHCA survivors.22 Although population selection was somewhat more restrictive (all patients with recorded rhythms) in the only published Spanish series on hypothermia after resuscitated cardiac arrest, the reported rate of neurologic sequelae-free survival of 44% is similar to the one we described.23
Thirdly, the elevated incidence of STEMI in our series and the optimal treatment of the condition may have contributed to the outcomes obtained. In a series described by Escorial-Hernández,8 only 40% of patients received reperfusion treatment. In contrast, in our study, 9 of the 10 patients with STEMI received reperfusion treatment, which has been associated with improved prognosis in sudden death survivors.13 Nevertheless, our study probably lacked the power to demonstrate that reperfusion treatment was an independent variable for good prognosis.
In terms of the etiology of cardiac arrest, ischemic heart disease played an important role in our series. Similar to previous studies, coronary disease explained 7 of 10 cardiac arrests.24 In 13.7% of cases, no etiologic diagnosis was available at discharge. It has been pointed out that systematized study protocols for these patients could enhance diagnostic performance.25
In our study, although there was no uniform protocol across the 5 sites, in addition to a shared approach to routine management all centers had access to a general document on the treatment of these patients. Sunde et al.26 reported that care protocolization and systematization improved the rate of neurologically intact survivors at discharge from 26% to 56%, data that are similar to the rates described in our study. Regarding neurologic prognosis, one of the factors that led to the nonuse of therapeutic measures and the phenomenon of self-fulfilling prophecy in these patients was the possibility that it might increase the number of patients with severe neurologic deficit or persistent vegetative state.7 In the present study, only 19 patients were discharged with CPC 3 or CPC 4, with very adverse prognosis; 8 of them died within 6 months. However, 85% of survivors were in good neurologic status at discharge and 92% at 6 months. Similar to previous studies, these results show that the clinical outcome of neurologically intact patients is excellent.27
In this regard, the use of new algorithms for the cardiac chain of survival and the use of a hypothermia protocol have led to changes in prognosis markers.28 Therefore, studies are needed to provide information on this new scenario. In our register, markers of better prognosis (first recorded rhythm, lower return of spontaneous circulation time, better hemodynamic status expressed as pH>7.1, lower incidence of cardiogenic shock, and use of therapeutic hypothermia) indicate improvements in the cardiac chain of survival from out-of-hospital care to in-hospital care. However, an important point for improvement is the infrequent use of basic resuscitation maneuvers by bystanders who witness OHCA.
LimitationsDespite the advantage afforded as a prospective register of all patients who have recovered from OHCA, in our opinion the most important limitation of our study was the difficulty in obtaining specific information related to arrest times and resuscitation maneuver start and duration times. These variables were not measured directly, but rather obtained from out-of-hospital emergency service reports and questioning of relatives and witnesses. Secondly, patient management was not based on a common protocol at all 5 sites, but rather on common guidelines. Moreover, remote follow-up of most patients and the use of the CPC classification did not allow a precise analysis of neurologic status, even though the methodology is recommended by various consensus documents.14 Lastly, because this is a CICU register, patients who died before they reached the hospital and those admitted in other health care areas (intensive care, resuscitation, etc.) were not included and, therefore, the conclusions cannot be extrapolated to the general population.
CONCLUSIONSIn our series, coronary disease explained 70% of cardiac arrests. Half the patients who survived OHCA and were admitted to CICUs had good vital and neurologic prognosis at discharge and at 6 months, even though they were in serious condition on arrival. Most deaths during follow-up were early and occurred in patients with the most neurologic impairment. Improvements in the initial care of cardiac arrest patients and routine, protocolized management of postcardiac arrest syndrome may have contributed to the good outcomes. Health education programs are necessary to enhance the use of basic CPR maneuvers by bystanders who witness an OHCA.
CONFLICTS OF INTERESTNone declared.
We thank Dr. Ángel Loma-Osorio and Dr. Coloma Tirón for their support and critical review of the article.