To investigate the relationship between the prevalence of cocaine use disorders and acute myocardial infarction in patients aged ≥ 18 years and to estimate the influence of cocaine use disorders on mortality, excess length of stay, and overexpenditure among hospitalized patients with acute myocardial infarction.
MethodsRetrospective study of the minimum basic data set of 87 Spanish hospitals from 2008 to 2010.
ResultsAmong 5 575 325 admissions reviewed, there were 24 126 patients with cocaine use disorders and 79 076 cases of acute myocardial infarction. The incidence of acute myocardial infarction among patients with cocaine use disorders increased with age and reached a peak at 55 years to 64 years (P < .0001). Multivariate analysis showed that cocaine use disorders were more prevalent among patients with acute myocardial infarction independently of age, sex, other addictive disorders, and 30 other comorbidities (odds ratio = 3.0). Among patients with acute myocardial infarction, those with cocaine use disorders did not show an increase of in-hospital death, but did show excess length of hospital stay (1.5 days) and overexpenditure (382 euros).
ConclusionsCocaine use disorders are associated with acute myocardial infarction and increase the length of hospital stay and overexpenditure among acute myocardial infarction patients. Cessation of cocaine use among these patients should be one of the primary therapeutic goals after hospital discharge.
Keywords
Cocaine use has increased in the last 10 years, and this substance is now the second most frequently consumed drug in Europe after cannabis.1,2 After the United Kingdom, Spain is the country with the highest prevalence of cocaine use among persons aged 15 years to 64 years, with 8.3% having consumed the drug at some time. Consumption is particularly high among young men (15-34 years): 5.5% during the last year and 1.9% during the last month,2 which has been attributed to its wide availability, ease of administration, increasingly lower cost, and the mistaken belief that recreational cocaine use is not dangerous.
Cocaine is the most widely used illicit drug among patients attending hospital emergency departments and drug rehabilitation centers.2–4
While cocaine use has been increasing, there has been an extraordinary rise in the number of its cardiovascular complications, such as unstable angina pectoris, acute myocardial infarction (AMI), aortic dissection, infectious endocarditis, and other entities.5,6 A topic that has been analyzed in the last few years is the impact of cocaine use disorders (cocaine abuse and dependence) on cardiovascular diseases in persons > 50 years, since, in many developed countries, there has been an increase in older cohorts with this addiction.7,8
To analyze the association between the prevalence of cocaine use disorders and AMI, we studied this phenomenon in patients aged ≥ 18 years admitted to a sample of 87 Spanish hospitals from 2008 to 2010 and attempted to control for other confounding and interaction variables, such as age, sex, other addictions, and a considerable number of comorbidities. Another aim of this study was to evaluate the possible influence of these disorders on mortality, excess length of hospital stay, and overexpenditure among patients hospitalized for AMI.
METHODSSample and ParticipantsMultistage sampling was performed, initially based on calculating the sample size of the study nationally and for autonomous communities, adjusted to their population weights. Problems related to alcohol, smoking and other drugs were analyzed with an alpha error of 5%, a 2-tailed test, a statistical power of 90%, a control:case ratio of at least 4:1, and a more unfavorable proportion of cases in which cases were exposed and controls were not exposed, based on the available scientific evidence. The hospital selection was adjusted to the distribution of hospital groups in each autonomous community, which resulted in 87 hospitals being selected from all the autonomous communities in Spain.
Based on the written or digitalized information in the medical record, each patient's diagnoses, the external causes and the procedures applied were codified, following the ICD-9 (ninth revision of the International Classification of Diseases and Causes of Death). Specialized personnel, with solid training and experience in data recording, codified the data and introduced the information in the databases. These databases contained information on demographic characteristics, admission and discharge dates, type of admission and discharge, diagnostic codes for the main and secondary diagnoses, and external causes and procedures, classified using ICD-9 codes. These databases also included diagnosis-related groups and each hospital was classified into a group, depending on its size and complexity.9 The analysis was restricted to patients ≥ 18 years of age at the time of hospital discharge.
VariablesCases of AMI, first episode, were defined as those in which the code appeared in the main diagnosis (codes 410.01-410.91). Cases were excluded if the code appeared in one of the secondary diagnoses, but not the main diagnosis. The ICD-9 codes were used to define cocaine use disorders as cocaine dependence (304.20-304.23) and cocaine abuse (305.60-305.63). Disorders due to cannabis, opioid, amphetamine, sedative or hypnotic, alcohol use and smoking were defined in a similar manner.
Age was quantified in years. The following comorbidities were identified: obesity, uncomplicated hypertension, complicated hypertension, arrhythmias, pulmonary circulation disorders, valvular disease, deficiency anemia, posthemorrhagic anemia, electrolyte disorders, weight loss, hypothyroidism, coagulopathy, previous AMI, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, rheumatic disease, peptic ulcer, diabetes mellitus without chronic complications, diabetes mellitus with chronic complications, hemiplegia or paraplegia, kidney disease, moderate or severe liver disease, cancer, leukemia or lymphoma, metastatic cancer, AIDS, and depression. We used the ICD-9 codes proposed by Quan et al10 for these comorbidities. The Charlson comorbidity index was also calculated for each patient.11
Data AnalysisThe main aim was to calculate the association between the incidence of AMI and cocaine use disorders in patients admitted to hospital. The secondary aims were to determine mortality, length of hospital stay, and hospital costs in patients with and without cocaine use disorders who had experienced an AMI. We calculated costs by using the specific hospital costs for each diagnosis-related group stratified by hospital group and using the estimates published by the Ministry of health for 2008 to 2010.9
A univariate analysis was performed to examine the association between AMI and addictive disorders, age, sex, and comorbidities. Then, multivariate models were constructed, using unconditional logistic regression analysis to determine the association between cocaine disorders and other addictions with AMI and in-hospital death due to AMI, and controlling for the remaining variables. A multivariate analysis of covariance was performed to determine the effect of cocaine use disorders on length of hospital stay in days and on costs in patients with AMI. The data were adjusted by age, sex, addictions, hospital group, and the above-mentioned comorbidities. The analysis was performed with the STATA statistical program, version MP 12.1.
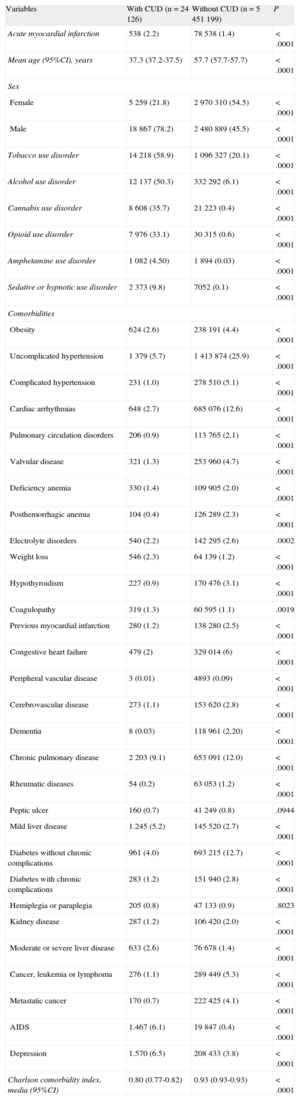
RESULTSPatient CharacteristicsThe characteristics of patients with and without cocaine use disorders are shown in Table 1. We identified 5 475 325 patients, of which 24 126 (0.44%) had cocaine use disorders and 79 076 (1.4%) were admitted for AMI. A total of 538 (2.2%) patients with cocaine use disorders were admitted for AMI, while 78 538 (1.4%) without these disorders were admitted.
Characteristics of Patients With and Without Cocaine Use Disorders
| Variables | With CUD (n = 24 126) | Without CUD (n = 5 451 199) | P |
| Acute myocardial infarction | 538 (2.2) | 78 538 (1.4) | < .0001 |
| Mean age (95%CI), years | 37.3 (37.2-37.5) | 57.7 (57.7-57.7) | < .0001 |
| Sex | |||
| Female | 5 259 (21.8) | 2 970 310 (54.5) | < .0001 |
| Male | 18 867 (78.2) | 2 480 889 (45.5) | < .0001 |
| Tobacco use disorder | 14 218 (58.9) | 1 096 327 (20.1) | < .0001 |
| Alcohol use disorder | 12 137 (50.3) | 332 292 (6.1) | < .0001 |
| Cannabis use disorder | 8 608 (35.7) | 21 223 (0.4) | < .0001 |
| Opioid use disorder | 7 976 (33.1) | 30 315 (0.6) | < .0001 |
| Amphetamine use disorder | 1 082 (4.50) | 1 894 (0.03) | < .0001 |
| Sedative or hypnotic use disorder | 2 373 (9.8) | 7052 (0.1) | < .0001 |
| Comorbidities | |||
| Obesity | 624 (2.6) | 238 191 (4.4) | < .0001 |
| Uncomplicated hypertension | 1 379 (5.7) | 1 413 874 (25.9) | < .0001 |
| Complicated hypertension | 231 (1.0) | 278 510 (5.1) | < .0001 |
| Cardiac arrhythmias | 648 (2.7) | 685 076 (12.6) | < .0001 |
| Pulmonary circulation disorders | 206 (0.9) | 113 765 (2.1) | < .0001 |
| Valvular disease | 321 (1.3) | 253 960 (4.7) | < .0001 |
| Deficiency anemia | 330 (1.4) | 109 905 (2.0) | < .0001 |
| Posthemorrhagic anemia | 104 (0.4) | 126 289 (2.3) | < .0001 |
| Electrolyte disorders | 540 (2.2) | 142 295 (2.6) | .0002 |
| Weight loss | 546 (2.3) | 64 139 (1.2) | < .0001 |
| Hypothyroidism | 227 (0.9) | 170 476 (3.1) | < .0001 |
| Coagulopathy | 319 (1.3) | 60 595 (1.1) | .0019 |
| Previous myocardial infarction | 280 (1.2) | 138 280 (2.5) | < .0001 |
| Congestive heart failure | 479 (2) | 329 014 (6) | < .0001 |
| Peripheral vascular disease | 3 (0.01) | 4893 (0.09) | < .0001 |
| Cerebrovascular disease | 273 (1.1) | 153 620 (2.8) | < .0001 |
| Dementia | 8 (0.03) | 118 961 (2.20) | < .0001 |
| Chronic pulmonary disease | 2 203 (9.1) | 653 091 (12.0) | < .0001 |
| Rheumatic diseases | 54 (0.2) | 63 053 (1.2) | < .0001 |
| Peptic ulcer | 160 (0.7) | 41 249 (0.8) | .0944 |
| Mild liver disease | 1.245 (5.2) | 145 520 (2.7) | < .0001 |
| Diabetes without chronic complications | 961 (4.0) | 693 215 (12.7) | < .0001 |
| Diabetes with chronic complications | 283 (1.2) | 151 940 (2.8) | < .0001 |
| Hemiplegia or paraplegia | 205 (0.8) | 47 133 (0.9) | .8023 |
| Kidney disease | 287 (1.2) | 106 420 (2.0) | < .0001 |
| Moderate or severe liver disease | 633 (2.6) | 76 678 (1.4) | < .0001 |
| Cancer, leukemia or lymphoma | 276 (1.1) | 289 449 (5.3) | < .0001 |
| Metastatic cancer | 170 (0.7) | 222 425 (4.1) | < .0001 |
| AIDS | 1.467 (6.1) | 19 847 (0.4) | < .0001 |
| Depression | 1.570 (6.5) | 208 433 (3.8) | < .0001 |
| Charlson comorbidity index, media (95%CI) | 0.80 (0.77-0.82) | 0.93 (0.93-0.93) | < .0001 |
95%CI, 95% confidence interval; CUD, cocaine use disorder.
Unless otherwise indicated, the data are expressed as no. (%).
Patients with cocaine use disorders were younger (mean age, 37.3 years), were mainly male (78.2%) and showed a high prevalence of addiction to all drugs, mainly tobacco (58.9%) and alcohol (50.3%), but also cannabis (35.7%), opioids (33.1%), amphetamines (4.5%), and sedatives or hypnotics (9.8%).
The mean Charlson comorbidity index score was lower in patients with cocaine use disorders, which could be explained by their mean age; in addition, in most of these patients, their rates of specific comorbidities were significantly lower–or without statistically significant differences–than those of patients without these disorders. However, patients with cocaine use disorders had a higher prevalence of weight loss, coagulopathies, mild, moderate or severe liver disease, AIDS, and depression.
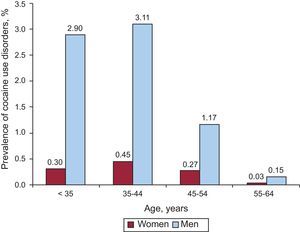
A more detailed analysis of the distribution of the prevalence of cocaine use disorders by age and sex is presented in Figure 1, which shows that, in both men and women, the group with the highest prevalence of these disorders was that aged 35 years to 44 years, followed by the group < 35 years, that aged 45 years to 54 years and, finally, that aged 55 years to 64 years.
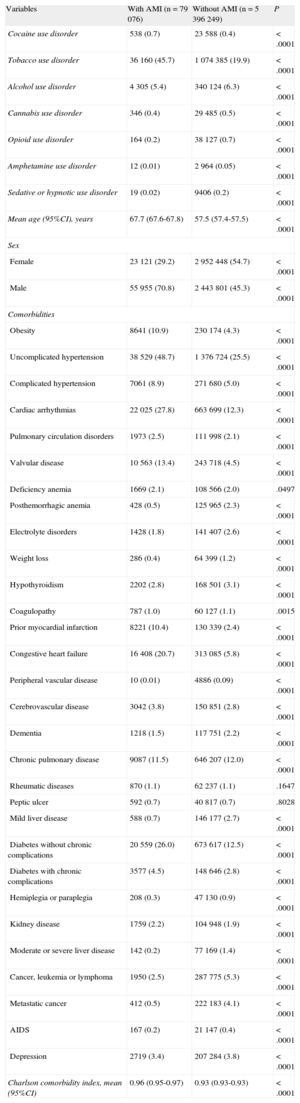
Association Between Cocaine and Acute Myocardial InfarctionThe characteristics of patients with and without AMI are shown in Table 2. Those admitted for AMI were older (mean age, 67.7 years), were mainly male (70.8%), and showed the two most prevalent addictions: tobacco (45.7%) and cocaine (0.7%).
Characteristics of Patients With and Without Acute Myocardial Infarction
| Variables | With AMI (n = 79 076) | Without AMI (n = 5 396 249) | P |
| Cocaine use disorder | 538 (0.7) | 23 588 (0.4) | < .0001 |
| Tobacco use disorder | 36 160 (45.7) | 1 074 385 (19.9) | < .0001 |
| Alcohol use disorder | 4 305 (5.4) | 340 124 (6.3) | < .0001 |
| Cannabis use disorder | 346 (0.4) | 29 485 (0.5) | < .0001 |
| Opioid use disorder | 164 (0.2) | 38 127 (0.7) | < .0001 |
| Amphetamine use disorder | 12 (0.01) | 2 964 (0.05) | < .0001 |
| Sedative or hypnotic use disorder | 19 (0.02) | 9406 (0.2) | < .0001 |
| Mean age (95%CI), years | 67.7 (67.6-67.8) | 57.5 (57.4-57.5) | < .0001 |
| Sex | |||
| Female | 23 121 (29.2) | 2 952 448 (54.7) | < .0001 |
| Male | 55 955 (70.8) | 2 443 801 (45.3) | < .0001 |
| Comorbidities | |||
| Obesity | 8641 (10.9) | 230 174 (4.3) | < .0001 |
| Uncomplicated hypertension | 38 529 (48.7) | 1 376 724 (25.5) | < .0001 |
| Complicated hypertension | 7061 (8.9) | 271 680 (5.0) | < .0001 |
| Cardiac arrhythmias | 22 025 (27.8) | 663 699 (12.3) | < .0001 |
| Pulmonary circulation disorders | 1973 (2.5) | 111 998 (2.1) | < .0001 |
| Valvular disease | 10 563 (13.4) | 243 718 (4.5) | < .0001 |
| Deficiency anemia | 1669 (2.1) | 108 566 (2.0) | .0497 |
| Posthemorrhagic anemia | 428 (0.5) | 125 965 (2.3) | < .0001 |
| Electrolyte disorders | 1428 (1.8) | 141 407 (2.6) | < .0001 |
| Weight loss | 286 (0.4) | 64 399 (1.2) | < .0001 |
| Hypothyroidism | 2202 (2.8) | 168 501 (3.1) | < .0001 |
| Coagulopathy | 787 (1.0) | 60 127 (1.1) | .0015 |
| Prior myocardial infarction | 8221 (10.4) | 130 339 (2.4) | < .0001 |
| Congestive heart failure | 16 408 (20.7) | 313 085 (5.8) | < .0001 |
| Peripheral vascular disease | 10 (0.01) | 4886 (0.09) | < .0001 |
| Cerebrovascular disease | 3042 (3.8) | 150 851 (2.8) | < .0001 |
| Dementia | 1218 (1.5) | 117 751 (2.2) | < .0001 |
| Chronic pulmonary disease | 9087 (11.5) | 646 207 (12.0) | < .0001 |
| Rheumatic diseases | 870 (1.1) | 62 237 (1.1) | .1647 |
| Peptic ulcer | 592 (0.7) | 40 817 (0.7) | .8028 |
| Mild liver disease | 588 (0.7) | 146 177 (2.7) | < .0001 |
| Diabetes without chronic complications | 20 559 (26.0) | 673 617 (12.5) | < .0001 |
| Diabetes with chronic complications | 3577 (4.5) | 148 646 (2.8) | < .0001 |
| Hemiplegia or paraplegia | 208 (0.3) | 47 130 (0.9) | < .0001 |
| Kidney disease | 1759 (2.2) | 104 948 (1.9) | < .0001 |
| Moderate or severe liver disease | 142 (0.2) | 77 169 (1.4) | < .0001 |
| Cancer, leukemia or lymphoma | 1950 (2.5) | 287 775 (5.3) | < .0001 |
| Metastatic cancer | 412 (0.5) | 222 183 (4.1) | < .0001 |
| AIDS | 167 (0.2) | 21 147 (0.4) | < .0001 |
| Depression | 2719 (3.4) | 207 284 (3.8) | < .0001 |
| Charlson comorbidity index, mean (95%CI) | 0.96 (0.95-0.97) | 0.93 (0.93-0.93) | < .0001 |
95%CI, 95% confidence interval; AMI, acute myocardial infarction.
Unless otherwise indicated, the data are expressed as no. (%).
The mean Charlson score was higher among patients with AMI, mainly due to the comorbidities associated with risk of AMI: obesity, hypertension, cardiac arrhythmias, pulmonary circulation disorders, valvular disease, prior AMI, congestive heart failure, cerebrovascular disease, diabetes mellitus without chronic complications, and diabetes mellitus with chronic complications.
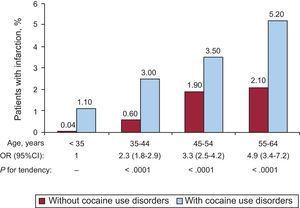
A more detailed analysis of the distribution of cases of AMI by groups of age and sex is presented in Figure 2, which shows that the prevalence of AMI increased with age and reached a peak in the group aged 55 years to 64 years; however, the odds ratio was significantly higher among patients with cocaine use disorders, with a significant positive tendency: the prevalence of AMI doubled among the group aged 35 years to 44 years, tripled among that aged 45 years to 54 years and quadrupled among the group aged 55 years to 64 years when compared with the reference group aged < 35 years (P for tendency < 0.0001). These analyses were limited to the population aged 18 years to 64 years, because only 3 patients aged ≥ 65 years had a cocaine use disorder and AMI.
Frequency of myocardial infarction in patients with and without cocaine use disorders by age groups. The odds ratio of each age group is shown in comparison with that in the group aged 18 years to 34 years and the P-value for tendency (chi-squared). 95%CI, 95% confidence interval; OR, odds ratio.
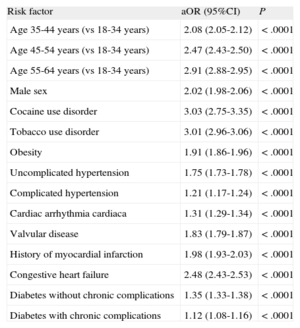
The results of the multivariate analysis are shown in Table 3, which reveals that the prevalence of AMI was 3-fold higher in patients with cocaine use disorders than in those without these disorders when the analysis was adjusted by age, sex, the remaining addictions, and the 30 comorbidities listed previously. The positive tendency between age and AMI was maintained in the multivariate analysis, but the differences between odds ratios were less marked than in the univariate analysis.
Logistic Regression Model for Hospital Admissions for Acute Myocardial Infarction in Patients aged ≥ 18 Years, 2008-2010
| Risk factor | aOR (95%CI) | P |
| Age 35-44 years (vs 18-34 years) | 2.08 (2.05-2.12) | < .0001 |
| Age 45-54 years (vs 18-34 years) | 2.47 (2.43-2.50) | < .0001 |
| Age 55-64 years (vs 18-34 years) | 2.91 (2.88-2.95) | < .0001 |
| Male sex | 2.02 (1.98-2.06) | < .0001 |
| Cocaine use disorder | 3.03 (2.75-3.35) | < .0001 |
| Tobacco use disorder | 3.01 (2.96-3.06) | < .0001 |
| Obesity | 1.91 (1.86-1.96) | < .0001 |
| Uncomplicated hypertension | 1.75 (1.73-1.78) | < .0001 |
| Complicated hypertension | 1.21 (1.17-1.24) | < .0001 |
| Cardiac arrhythmia cardiaca | 1.31 (1.29-1.34) | < .0001 |
| Valvular disease | 1.83 (1.79-1.87) | < .0001 |
| History of myocardial infarction | 1.98 (1.93-2.03) | < .0001 |
| Congestive heart failure | 2.48 (2.43-2.53) | < .0001 |
| Diabetes without chronic complications | 1.35 (1.33-1.38) | < .0001 |
| Diabetes with chronic complications | 1.12 (1.08-1.16) | < .0001 |
95%CI, 95% confidence interval; aOR, adjusted odds ratio.
The multivariate analysis showed no association between having a cocaine use disorder and mortality among patients with AMI.
The multivariate analysis of covariance, which included age, sex, hospital group, and all the above-mentioned addictions and comorbidities, showed that, among patients with an AMI, those with cocaine use disorders had a mean excess length of hospital stay of 1.5 days (95% confidence interval, 1.4-1.6 days). Overexpendure due to hospital stay among patients with an AMI and cocaine use disorder was 382 (95% confidence interval, 298-464) euros.
DISCUSSIONOur results indicate that cocaine use disorders significantly impact the incidence of AMI, independently of age, sex, smoking, other addictions, and the 30 comorbidities studied. When the adjusted odds ratio for AMI were considered in the multivariate model, the excess incidence of AMI in patients with cocaine use disorders was 203% in comparison with patients without these disorders (odds ratio = 3.0). Among patients with an AMI, those with cocaine use disorders had more prolonged hospital stays and higher hospital costs.
There is abundant evidence in the scientific literature indicating that cocaine use disorders are an independent risk factor for AMI and other cardiovascular diseases.5,6 Cocaine use triggers coronary failure through several mechanisms,12 stimulates the sympathetic nervous system by inhibiting catecholamine reuptake in the nerve endings and increasing their sensitivity to noradrenaline,13 promotes endothelial release of endothelin-1–a potent vasoconstrictor14, and inhibits production of nitric acid, the main vasodilator produced by endothelial cells.15 Likewise, cocaine use promotes coronary thrombosis through platelet activation,16,17 thus favoring platelet aggregation17,18 and increasing the activity of plasminogen activator inhibitors19 and concentrations of fibrinogen and von Willebrand factor.20
The isolated impact of cocaine use is especially marked in the youngest users, among whom the cumulative effects of cocaine do not compete with those of other addictions and the comorbidities that increase with age. Our results showed a positive association of age with the incidence of AMI, which is higher among patients with cocaine use disorders. The group aged 55 years to 64 years had the highest odds ratio, which can easily be explained by the greater number of comorbidities with age and the cumulative effect of prolonged use of cocaine and other substances. Some estimates indicate that, in the United States, the number of patients ≥ 50 years who seek treatment for their addictions will increase from 1.7 million in the year 2000 to 4.4 million in 2020.7 Similar estimates have been made in Europe, where the number of older patients seeking treatment for their addictions will double from 2001 to 2020.21 These tendencies are the result of the demographic phenomenon of the aging population in developed countries, and particularly reflect aging of the “baby-boom” generation, consisting of persons born between 1946 and 1964.7
The high prevalence of smoking, alcohol use, and other addictions in patients with cocaine use disorders is worrisome. Multiple addictions are widespread among patients with drug disorders. Simultaneous tobacco and cocaine exposure increases the risk of AMI, because smoking produces vasoconstriction of the coronary arteries through alpha-adrenergic stimulation similar to that provoked by cocaine.22 The combination of tobacco and cocaine increases heart rate, the energy used for contraction, and systemic arterial pressure, all of which increases myocardial oxygen needs and, at the same time, reduces oxygen supply due to vasoconstriction.23 Simultaneous cocaine and alcohol use produces cocaethylene, which also blocks neurotransmitter reuptake in the nerve endings and enhances the toxic systemic effects of cocaine.24,25
LimitationsOur study has several limitations. The data used were drawn exclusively from the Minimum Basic Data Set (MBSD) and were not completed by additional data from the patients. Throughout the study, we used the definitions of addictive disorders, AMI and comorbidities as assigned the physicians in each center, which were then codified and introduced in the databases by the codifiers. Another limitation is the potential under-registration of information due to the possibility that the medical record did not contain all the data required for the codifiers to assign codes or due to variation in the codifiers’ interpretations.
The prevalence of cocaine use disorders in the hospitalized population was markedly higher in men than in women, and the group with the highest rate (3.5%) consisted of men aged 35 years to 44 years. The real prevalence is probably underestimated in hospitalized patients, given the results of several studies comparing the reported addiction rate with other objective indicators such as the prevalence of cocaine metabolites in urine. In a study by Bosch et al,26 19% of the patients did not admit to having used cocaine, even though cocaine metabolites were detected in their urine. In other studies, the proportion of patients denying cocaine use varied: 28% of the patients in a study by Hollander et al27 and 48.2% of those in a study by Lee et al.28 All these factors indicate that the present study probably underestimated the number of cases of AMI concomitant to cocaine use and that the impact of cocaine is probably considerably greater.
Databases such as the MBSD also have considerable advantages.29 Registered data is usually complete in most hospital discharges and, because these databases include practically all cases, they allow fairly accurate estimates on incidence, prevalence, comorbidities, and mortality from diseases attended in the hospital setting.30 These data can be retrospectively analyzed, unlike other designs that require prospective data collection. Data from long periods and a large number of patients, as in the present study, can be collected relatively rapidly and easily. Because the data are systematically gathered, the cost reduction is considerable. Studies based on these databases may show fewer selection biases, such as those biases that lead patients or their legal representatives to refuse to sign informed consent and participate in the study.
The results of this study are supported by several factors. We used the 410.x1 codes of the ICD-9 for AMI, first episode as the main diagnosis (excluding those that appeared as a secondary diagnosis), following the inclusion and exclusion criteria of the United States’ AHRQ (Agency for Healthcare Research and Quality) in its health care quality indicator “in-hospital mortality from acute myocardial infarction”31 to obtain maximal validity of AMI diagnosis. A study carried out and published in Spain that used the MBSD and the AHRQ criteria found that mortality from AMI was highly similar to that of patients who were followed up in observational studies such as PRIMHO, PRIMHO II, RISCI, and ARIM.32 The latter study also found that other characteristics, such as distribution by sex, mean age, and the frequency of cardiovascular risk factors, were similar, indicating that the use of the MBSD led to adequate representation of the epidemiological profile of AMI.32 The results of another study on the validity of the comorbidities of AMI in Spain, calculated from MBSD data, which also used the AHRQ inclusion and exclusion criteria, suggest that the information obtained from the MBSD is reliable and valid.33 The latter study, which analyzed in-hospital mortality from AMI from 2003 to 2009, observed that mortality was decreasing, a finding that also coincides with the tendency noted in other observational studies carried out in Spain.34,35
The overexpenditure incurred by patients with cocaine use disorders was due to 2 factors. First, the higher number of diagnostic and therapeutic procedures and the greater number of complications in these patients, which led to their inclusion in more expensive diagnosis-related groups. Second, the excess cost was attributable to longer hospital stay.
Because of the sample size and the diversity of hospitals, our data can be generalized and are not limited to patients admitted to one or a few hospital centers. Calculation of overexpenditure was facilitated by the availability of costs for each diagnosis-related group stratified by hospital groups and by each year. To our knowledge, this is the first study that calculates the excess hospital stay and overexpenditure attributable to cocaine use disorders in patients with AMI.
One of the main therapeutic objectives after hospital discharge is cessation of cocaine use. The incidence of chest pain, AMI, and death decrease in patients who cease using cocaine.36,37 The remaining cardiac risk factors should be modified, especially cigarette smoking,12 as well as any other addictions. Activities with demonstrated effectiveness that could prevent AMI recurrence in these patients include a brief intervention on the risks of these substances and referral to specialized rehabilitation services. Given the current economic restrictions, decreasing the number of admissions and readmissions due to cocaine would help to reduce hospital costs and increase the availability of hospital beds. Each case of AMI and of other diseases avoided or of prevented admission would also reduce the burden of the multiple problems experienced by these patients in a particularly difficult and stressful era.
CONCLUSIONSAmong patients with AMI, cocaine use disorders are associated with the incidence of AMI, excess hospital stay, and overexpenditure. Cessation of consumption of cocaine and other addictive substances should be one of the main objectives in these patients after hospital discharge.
FUNDINGThis study was funded by the Delegación del Gobierno para el Plan Nacional Sobre Drogas, Ministerio de Sanidad, Servicios Sociales e Igualdad (Grant No. 009I017, Project G41825811).
CONFLICTS OF INTERESTNone declared.