In line with the policy on clinical practice guidelines previously established by the Executive Committee of the Spanish Society of Cardiology (Sociedad Española de Cardiología [SEC]),1 this article aims to discuss the most important and novel issues in the 2015 European Society of Cardiology (ESC) guidelines for the diagnosis and management of pericardial diseases.2 The guidelines update the recommendations contained in the previous 2004 version3 and include new evidence on pericardial diseases that has come to light since then.
METHODSThe SEC Guidelines Committee created a working group to review the evidence and recommendations included in the European guidelines on pericardial diseases.2 All members of the working group were asked to review the guidelines using a questionnaire covering the following features: a) methodology analysis; b) novel contributions and issues particularly relevant to clinical practice; c) analysis of the most positive and most questionable aspects of those contributions; d) gaps in the guidelines; and e) conclusions and implications for clinical practice. Based on the experts’ comments, a consensus document was drafted and approved by all the members of the working group. The document was reviewed by a second panel of experts proposed by both the Clinical Cardiology Section and the SEC Guidelines Committee, and their comments were included in the final document.
GENERAL COMMENTS AND METHODOLOGY ANALYSISThe main difference with the 2004 guidelines is that the recommendations in the current version are expressed through classes of recommendation (I, IIa, IIb, and III) and levels of evidence (A, B, and C). Also, the recommendations in the 2015 guidelines are shown in tables, with their corresponding classes and levels of evidence, whereas the 2004 version contained few tables, and levels of evidence were reported in text. The current guidelines contain a total of 135 recommendations. As shown in Table 1, the proportion of recommendations with level C evidence (based on expert consensus) is very high (99 out of 135 recommendations; 73%). Only 6 recommendations are supported by level A evidence and 29 are based on level B evidence. Most recommendations are supported by level C evidence, which does not invalidate them but leaves a wide margin for critical evaluation and individual medical judgment. More than half the recommendations are class I (51%) and 8% are class IIa. Thus, the level of available evidence on the management of pericardial diseases is low, which should encourage new studies on these diseases.
The guidelines are organized in several sections (epidemiology, etiology, pericardial syndromes, diagnostic work-up and imaging techniques, specific etiologies of pericardial syndromes, age and sex issues, surgery and interventional techniques, and perspectives); the present document will discuss the most relevant, novel, and questionable aspects.
RELEVANT AND NOVEL ASPECTSThe most important and novel aspects of the current guidelines are listed in Table 2.
New and Most Important Features
| 1. A new section on the epidemiology of pericardial diseases |
| 2. A lower level of evidence for diagnostic criteria for acute pericarditis (from I-A to I-B) |
| 3. Clinical predictors of poor prognosis (major and minor) in the initial management algorithm |
| 4. Colchicine as an initial treatment for acute pericarditis (I-A) and lower doses compared with the 2004 guidelines |
| 5. Recurrent pericarditis is distinguished from incessant and chronic forms, and a specific section has been added on recurrent forms |
| 6. Colchicine as first-line therapy for recurrent pericarditis (I-A) |
| 7. Intravenous immunoglobulin, anakinra, or azathioprine as third-line therapies for recurrent pericarditis |
| 8. Myopericarditis is discussed as a separate entity |
| 9. Clarity and simplicity in the section on the management of pericardial effusion |
| 10. A new score as a guide to the timing of pericardiocentesis in cardiac tamponade |
| 11. Three different clinical forms of pericardial constriction are considered separately: transient, effusive-constrictive, and chronic |
| 12. A specific section on diagnostic tests with a proposal for a reasonable and easy to understand approach to diagnostic work-up in pericardial disease |
| 13. Clear and reasonable recommendations for etiologic diagnosis in patients with pericarditis and pericardial effusion |
| 14. Viral serologies are not useful for the diagnosis of viral pericarditis |
| 15. New criteria (differing from those for other forms of pericarditis) for pericardial involvement in post-cardiac injury syndromes |
| 16. Specific new sections on age and sex subgroups (children, older persons, pregnant women) |
| 17. Seventeen poorly understood issues requiring further research are reported (“Perspectives and unmet needs”) |
The new 2015 guidelines include a new section on the epidemiology of pericardial diseases. Acute pericarditis accounts for 0.1% of hospital admissions and mainly affects young adults (aged 16-65 years). In-hospital mortality is 1.1% (associated with severe infectious diseases) and the risk of recurrence is about 30% after 18 months. The latter statement is based on 2 studies by Imazio et al4,5 and clearly deserves comment. To assume that almost one third of patients with acute pericarditis will have a recurrence seems an overestimate and is certainly very far from our experience in daily clinical practice. The very high rate of recurrences found in those studies could be explained by 2 factors: population bias (15% of patients in the COPE study4 had pericarditis associated with an autoimmune disease), and the high steroid use, which is difficult to justify (33% of patients with recurrences and 10.9% of patients without recurrences had received steroids before randomization, and 16% also received steroids during follow-up). In Spain, the recurrence rate in patients with “idiopathic” acute pericarditis (accounting for 90% of cases of acute pericarditis in general series) is lower than 10%.6 In patients admitted to tertiary hospitals, once a comprehensive diagnostic protocol has been applied, a higher proportion of associated diseases is found (up to 22% of secondary pericardial diseases) and recurrences are more common.7,8
Pericardial SyndromesPericardial syndromes are classified in 7 groups: acute pericarditis, incessant and chronic pericarditis, recurrent pericarditis, myopericarditis, pericardial effusion, cardiac tamponade, and constrictive pericarditis. There is no mention of congenital pericardium defects, which were discussed in the 2004 guidelines.
Acute PericarditisThe current guidelines include a clearer definition of the diagnostic criteria for acute pericarditis, and require 2 of the following criteria to be present: chest pain, pericardial friction rub, electrocardiogram (ECG) changes, and pericardial effusion. The use of 4 diagnostic tests is recommended in all patients with suspected acute pericarditis: ECG, transthoracic echocardiography (TTE), chest X-ray, and markers of inflammation (ie, C-reactive protein [CRP]) and myocardial damage (creatine kinase, troponin). Interestingly, all 4 tests to be used in all patients with suspected pericarditis have the same class of recommendation and level of evidence (I-C); however, only ECG and echocardiography are useful to establish a diagnosis of acute pericarditis. Compared with the 2004 guidelines, the level of evidence has been lowered from I-B to I-C.
The guidelines do not specify when the 4 diagnostic tests should be performed (it may be inferred, though, that they should be performed on admission) and no recommendation is provided on whether or not they should be repeated or at what interval. These omissions lead to several questions that are not clarified by the current guidelines: Is a single ECG on admission sufficient or should a repeat ECG be obtained to monitor the evolution of ECG changes? If serial ECGs are required, when and how frequently should they be performed? Should TTE and X-ray be performed immediately or within 24hours? Should markers be determined both on admission and in subsequent serial measurements? How frequently and for how long? In the section on clinical management and therapy, a return to activity is recommended once the symptoms have resolved and “diagnostic tests have been normalized”, suggesting that initial diagnostic tests with an abnormal result should be repeated once or several times (not specified). A much more controversial issue is the recommendation for initial doses of anti-inflammatory therapy to be maintained until symptom resolution and CRP normalization. In other words, at least 1 additional CRP measurement must be obtained after a 1-week course of therapy to document CRP normalization before the aspirin dose is reduced. If high CRP values persist (which is not uncommon due to its poor specificity), should anti-inflammatory drug dosing be maintained ad aeternum and CRP measurements be repeated weekly even if the patient is asymptomatic? In our opinion, the need to use CRP for acute pericarditis diagnosis is highly dubious, and the need to use CRP to guide treatment decisions is even more questionable.
Regarding clinical management, the current guidelines include a novel proposal for a set of major and minor predictors of “poor prognosis”. Major risk factors include high fever (> 38°C), subacute course, evidence of significant (> 20mm) pericardial effusion, cardiac tamponade, and lack of response to nonsteroidal anti-inflammatory drugs (NSAIDs) within 7 days. Myopericarditis, immunosuppression, traumatic injuries, and the use of oral anticoagulants are considered to be minor risk factors. Most of the predictors are defined rather imprecisely. Moreover, all the predictors have the same role in decision-making on hospital admission: any patient with a major predictor or a single minor predictor should be admitted. However, these predictors of poor prognosis can have very different implications. Two examples: first, both a fever of 38.1°C and cardiac tamponade are considered to be major predictors of poor prognosis, but their significance differs; second, it is hard to accept that a fever of 38.1°C should be considered a major predictor whereas myopericarditis associated with a substantially elevated troponin level is classed as a minor predictor.
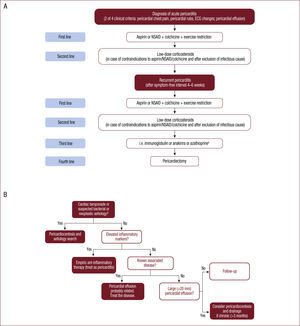
Undoubtedly, the most innovative item is drug therapy, based on the publication of 4 randomized multicenter trials on the use of colchicine in patients with acute4,5 and recurrent pericarditis.9,10 These trials have allowed the recommendation to use colchicine as a first-line drug to be supported by the highest level of recommendation and evidence (I-A). In acute pericarditis, colchicine is recommended as a first-line drug to be added to aspirin/NSAIDs (Figure A). Importantly, to improve tolerability and help improve adherence, the recommended doses for colchicine are lower than those in the 2004 guidelines. The recommended starting dose depends on the patient's weight: 0.5mg once daily (< 70kg) or 0.5mg bid (> 70kg) for 3 months; tapering of colchicine is not mandatory before discontinuation. In athletes, physical activity should continue to be restricted for at least 3 months after symptom resolution and normalization of CRP, ECG, and echocardiography (IIa-C).
A controversial issue in the current guidelines is the recommendation for CRP determination as a guide to assessing response to anti-inflammatory therapy, instead of routine clinical criteria alone. Another important issue to be qualified in the current guidelines is that, although steroids are not recommended as a first-line therapy (III-C), recommendations against steroid use except in very specific cases are not clearly emphasized. In fact, the guidelines include a class IIa-C recommendation for the use of low-dose steroids when aspirin/NSAIDs and colchicine are contraindicated or have failed. In our opinion, it would have been much more appropriate to emphasize the multiple adverse effects associated with steroids and the high risk of recurrence or chronification of pericarditis, an essentially benign disorder if appropriately treated.
Incessant and Chronic PericarditisPericarditis is considered to be “incessant” when symptoms persist for more than 4 to 6 weeks, and “chronic” when it persists for more than 3 months (particularly in patients with persistent pericardial effusions).
Recurrent PericarditisThe 2004 guidelines discussed recurrent and incessant pericarditis within the same section, whereas the 2015 version includes a separate section on incessant pericarditis and has substantially expanded the section on recurrent pericarditis. Diagnosis of recurrences should be based on the same criteria as those used for acute pericarditis, with a minimum symptom-free interval of 4-6 weeks after the initial episode (otherwise, incessant pericarditis is considered to be present). If there is doubt, CRP, computerized tomography (CT) and cardiac magnetic resonance imaging (CMR) may be helpful for diagnosis. The main causes of “inadequate treatment” in the acute phase resulting in incessant, chronic, or recurrent pericarditis are given as: a premature return to physical activity, not using colchicine on top of aspirin/NSAIDs, and, especially, the use of corticosteroids, which is frequently unwarranted.
Key points for the treatment of recurrent pericarditis are well covered in the current guidelines, the main changes being: a) a higher level of evidence favoring colchicine as first-line therapy; b) the recommendation to use CRP measurements as a guide to treatment response (we consider this to be unwarranted); c) changes in immunosuppressive therapy, and d) the lesser importance assigned to intrapericardial corticosteroid administration. Two multicenter randomized trials9,10 have unequivocally shown the value of colchicine (added to aspirin/NSAIDs) to treat recurrent pericarditis and have confirmed the results of early studies performed in Spain almost 30 years ago.11,12 Corticosteroids should only be used as second-line therapy (in patients with inadequate response or contraindication to aspirin/NSAIDs + colchicine), at low doses, and always after careful exclusion of an infectious cause (Figure A). Tapering of corticosteroids must be very slow. Immunosuppressants are a third-line therapy. Cyclosporine is no longer recommended, whereas the recommendation for azathioprine use is maintained and new alternatives have been added such as intravenous immunoglobulin and anakinra; expectations of nonabsorbable corticosteroid administration have been lowered due to insufficient experience.
MyopericarditisThe section on myopericarditis is entirely new. The recommendations are, however, supported by level C evidence. Patients are diagnosed with myopericarditis if the criteria for acute pericarditis are fully met and there are elevations of biomarkers of myocardial injury (troponin I or T, creatine kinase MB fraction), without newly developed focal or diffuse impairment of left ventricular function. Endomyocardial biopsy is not recommended due to the benign prognosis of pericarditis. On the other hand, an issue that could become very controversial is the recommendation of coronary angiography in patients with myopericarditis “according to clinical presentation and risk factor assessment” to rule out acute coronary syndromes (I-C). This is an invasive and expensive test and entails a significant risk in patients with a usually benign disorder. It should be emphasized that, in patients presenting to the emergency room with acute chest pain and persistent ST-segment elevation, an acute coronary syndrome must be ruled out before a diagnosis of “myopericarditis” can be made; if there is doubt, emergency coronary angiography should be performed instead of waiting for elevation of markers of myocardial damage.
Finally, regarding anti-inflammatory therapy, the class of recommendation has been lowered to IIa-C. Aspirin or NSAIDs can be used for anti-inflammatory therapy, with recommended doses being lower than those used for pericarditis, because animal models of myocarditis have shown a lack of efficacy and increased mortality with NSAIDs use.
Pericarditis with Pericardial EffusionA new feature in the 2015 guidelines is that tamponade and pericardial effusion are presented under distinct headings, and echocardiographic effusion sizes are classified into 3 types (mild, < 10mm; moderate, 10-20mm; and large, > 20mm) instead of 4. Recommendations and algorithms on the management and treatment of pericardial effusion are notable (Figure B). One of the 2 main references supporting these recommendations13,14 comes from a nearby country.14 For symptomatic patients with no evidence of inflammation or when an NSAID trial has failed, the guidelines recommend consideration of pericardiocentesis and prolonged catheter drainage, based on a lower relapse rate. Prognosis depends on etiology. Moderate/large effusions are more commonly associated with bacterial and malignant causes. Idiopathic cases have a favorable prognosis in mild or moderate effusions, although a recent series including more than 9000 patients has not corroborated a benign course for asymptomatic mild effusions.15 Patients with large chronic pericardial effusions have a high cardiac tamponade risk; this is also true for subacute effusions unresponsive to anti-inflammatory therapy. Follow-up is well described in the new guidelines. Mild idiopathic effusions have a favorable prognosis with no follow-up being needed; moderate and large effusions can progress and result in a tamponade in one third of cases; thus, regular echocardiographic follow-up is recommended at 6-month intervals for asymptomatic cases and at 3- to 6-month intervals for large effusions (Figure B).
Cardiac TamponadeThe main improvement in the new guidelines are their greater clarity; common causes of tamponade (pericarditis, tuberculosis, iatrogenic complications, traumatic injuries, and neoplasms) and less common causes, as well as and diagnostic tools, are clearly summarized. Unless echocardiography is unavailable, CMR and CT are unnecessary. Only 2 recommendations (both based on level C evidence) are made: a) in patients with clinical suspicion of tamponade, echocardiography is recommended to evaluate the size, location, and hemodynamic impact, and b) pericardiocentesis or surgical drainage is recommended to treat tamponade. Echocardiography- or fluoroscopy-guided pericardiocentesis is the usual method of choice for drainage. Surgery is reserved for the following 4 scenarios: type-A aortic dissection, free wall rupture after a myocardial infarction, recent and severe chest trauma, and iatrogenic hemopericardium when bleeding cannot be controlled through percutaneous access. The main new feature is a scoring system proposed by the ESC working group on myocardial and pericardial diseases as a guide to the timing of the intervention; this system will require validation (recommendation IIb-C). The system evaluates etiologic, clinical, and imaging features and, if the score is ≥ 6, pericardiocentesis should not be postponed (Figure B).
Constrictive PericarditisThe main new feature is the classification of constrictive syndromes into 3 types. In previous guidelines, definitions, pathophysiology, and the management of such syndromes were not precisely described. By contrast, surgical aspects are rather superficially discussed in the new guidelines.
The guidelines clearly state that constrictive pericarditis can occur after any pericardial disease, but rarely develops after recurrent pericarditis. Cardiac catheterization is suggested as a diagnostic tool when doubts persist after clinical and other noninvasive imaging tests. Surgery is a mainstay of treatment of constrictive pericarditis, but medical therapy is considered very important for 3 specific therapeutic aims: a) specific etiologic therapy; b) anti-inflammatory therapy for transient constrictive pericarditis, especially when markers of inflammation are persistently high or inflammation is still seen in CMR or CT, and c) management of right-sided cardiac failure symptoms, which can be useful to postpone surgery or may even be the only useful therapy in patients with high surgical risk. The indications and limitations of pericardiectomy are highlighted in the new guidelines. Pericardiectomy is recommended for highly symptomatic patients (New York Heart Association [NYHA] functional class III-IV) and should be cautiously considered in patients with mild symptoms or those with an advanced stage of the disease (cachexia, atrial fibrillation, low cardiac output, hypoalbuminemia, liver dysfunction), those showing myocardial dysfunction or significant kidney failure, and those with a disease secondary to radiotherapy. However, the degree of pericardial calcification has no impact on survival. Child-Pugh score should be assessed, because a score > 7 (B or C) is associated with high mortality.
Diagnostic Work-up and Imaging. Multimodality ImagingA specific section on the main contributions of various imaging methods has been added, and a reasonable and easy to understand approach to diagnostic work-up is suggested. Two tables have been included to summarize and compare the findings, strengths, and limitations of echocardiography, CT, and CMR. The timing of CT or CMR use is not specified, and both are considered to be second-line tests for use when additional data are needed. In Spain, access to these imaging tests—especially CMR—may still be limited in some institutions; however, they are increasingly becoming universally used techniques.
Echocardiography is a first-line imaging test and should be used in all patients with clinical suspicion of pericardial disease (recommendation I-C). For selected cases not fulfilling any other severity criterion and with no evidence of cardiomegaly on chest X-ray, institutions without ultrasound equipment might consider omitting this examination. Moreover, in some patients, such as those with suspected pericardial effusion, the use of a pocket ultrasound device may be adequate to rule out significant disease. The appropriate use of this novel technology is not defined in the current guidelines.
One important new feature is the clear and reasonable recommendations for etiologic study in patients with pericarditis and pericardial effusion, similar to those suggested by Spanish groups some years ago.7,8 The proposed etiologic study takes into account both the clinical relevance of etiologic diagnosis (causes for which there is specific therapy, especially tuberculous pericarditis, pericarditis associated with systemic diseases, and neoplastic pericarditis) and the regional epidemiological profile. In Europe, relevant and reliable epidemiological data have been reported by Spanish,7,8 Italian, and French groups; thus, these recommendations are clearly valid in Spain. Some risk factors have been associated with a higher proportion of selected etiologies in epidemiological studies. However, we believe that not every risk factor is likely to have the same impact, and the mere presence of 1 risk factor does not always warrant the performance of aggressive tests. For example, a patient with typical clinical manifestations suggesting acute pericarditis and presenting with a large pericardial effusion who shows a rapid response to anti-inflammatory therapy is likely to have a benign cause, and pericardiocentesis can be avoided in many cases. In our opinion, a clear limitation of this section is the lack of a clear indication on when to suspect a specific cause and order aggressive diagnostic tests, and the appropriate sequence of these tests.
Algorithms for the management of acute and recurrent pericarditis (A) and pericardial effusion (B) according to Figure 2 of the 2015 guidelines on pericardial diseases2. NSAID, nonsteroidal anti-inflammatory drugs.
Seven specific etiologies are discussed: viral, bacterial, kidney failure, autoimmune or inflammatory diseases, post-cardiac injury syndromes, post-traumatic and neoplastic, and miscellanea. Each subsection includes summary tables with recommendations on diagnosis and therapy, with levels of evidence (11 new tables).
Diagnosis of viral pericarditis requires histological, cytological, immunohistochemical, and molecular assessments in either pericardial fluid or pericardial/epicardial biopsy specimens. By contrast, viral serology has no role in diagnosis (with the exception of human immunodeficiency and hepatitis C viruses) (class III). Specific therapies included in the previous guidelines have been eliminated, because they are still under investigation. A recommendation against steroid use is included (III-C). Regarding tuberculous pericarditis, the recommended treatment duration has been reduced to 6 months. For bacterial pericarditis, intrapericardial antibiotic therapy is no longer recommended. The term autoreactive pericarditis, which was meant to include pericardial disorders due to inflammatory and autoimmune diseases in the previous guidelines, is no longer used. The section on post-cardiac injury syndromes has been thoroughly revised. This section groups together several forms of pericardial inflammation (such as post-infarction, post-pericardiotomy, and post-traumatic pericarditis) with a presumed shared autoimmune pathogenesis after an initial myocardial injury. The new guidelines propose a new set of diagnostic criteria for these syndromes, which differ from the diagnostic criteria for pericarditis.16 Regarding prevention, a systematic review has shown that only colchicine is associated with a reduced risk of post-pericardiotomy syndromes. However, due to an increased risk of gastrointestinal adverse events, colchicine is not recommended as perioperative therapy, unless there are signs of systemic inflammation.
Age and Sex Issues in Pericardial DiseasesA specific section is included on the pediatric age group. Up to 5% of children presenting to emergency rooms with chest pain have pericarditis. Clinical and prognostic features, as well as recurrences and diagnostic criteria, are similar to those in adults. The online supplementary material includes a treatment schedule for pediatric patients. The recurrence rate appears to be halved by colchicine (recommendation IIa-C), and avoidance of steroid use is more strongly emphasized than in adults. Anakinra (an interleukin-1 receptor antagonist) is also included as a therapeutic option, especially for steroid-dependent children (class of recommendation IIb-C). A class III-C recommendation has been assigned to aspirin and steroids.
No new features have been included on pregnancy, breast feeding, and women of reproductive age. However, a proposed treatment scheme in the online supplementary material deserves mention. High-dose aspirin (500-750mg/8h) is still recommended as a first-line drug during the first 20 weeks of pregnancy, and NSAIDs may be considered during the first and second trimesters. After week 20, NSAIDs may cause constriction of the ductus arteriosus and renal disorders. They should always be withdrawn at week 32.
Regarding elderly patients, only a brief comment is included to highlight the need to assess comorbidities and poor treatment adherence. Indomethacin use is not recommended. Colchicine doses should be halved and care should be taken to assess renal function and drug–drug interactions.
Interventional Techniques and SurgeryA specific section has been added to describe fluoroscopy- or echocardiography-guided pericardiocentesis as well as pericardioscopy, but no new features have been added compared with the earlier guidelines. Relative contraindications for pericardiocentesis included in previous guidelines are no longer mentioned. Brief discussions on intrapericardial therapy and pericardial access for electrophysiology do not include important new features. A specific section on the pericardial window and pericardiectomy is included in the current guidelines, instead of discussing these methods in various sections as in the previous version, and surgical technique is now described.
Perspectives and Unmet NeedsThe guidelines provide a very stimulating description of several unresolved issues in pericardial disease. Seventeen issues for future research are mentioned. The most relevant issues include: a) a better understanding of pathophysiology and risk factors for recurrent and constrictive pericarditis; b) should physical activity restriction still be recommended for patients with acute and recurrent pericarditis?; c) is intrapericardial fibrinolysis really useful and safe in exudative pericarditis? and d) what actually is pericarditis and what is myocarditis?
QUESTIONABLE ASPECTS AND GAPS IN THE GUIDELINESQuestionable issues and gaps have been mentioned in previous sections and are summarized in Table 3.
Questionable Aspects and Gaps in the Guidelines
| 1. Excessively high incidence reported for recurrent pericarditis in the epidemiology section |
| 2. Need to measure C-reactive protein at the time of diagnosis and its use as a guide to the duration of anti-inflammatory therapy |
| 3. The prognostic value of various major and minor risk factors in acute pericarditis is not precisely described |
| 4. Insufficient emphasis is placed on the recommendation to avoid corticosteroid use in acute and recurrent pericarditis, due to their adverse effects and the increased rate of recurrences and chronicity |
| 5. The recommendation for coronary angiography in myopericarditis is rather imprecise |
| 6. When to suspect a specific etiology and use various aggressive test is not clearly stated |
| 7. Although a table showing available tests to be used for specific clinical suspicion is provided, a sequence of use is not suggested. |
| 8. Limited information and relevance of surgical and interventional techniques |
The new 2015 guidelines on pericardial diseases address an important gap in the literature, because the previous version was published 11 years ago. Although the document includes a large number of class C recommendations (expert opinions and consensus) due to the lack of randomized trials on pericardial diseases, it provides a clearer diagnostic and therapeutic approach to different kinds of pericardial syndromes and to the use of currently available techniques. New and more extensive evidence focuses on the use of colchicine as a first-line therapy for acute and recurrent pericarditis. Diagnostic, prognostic, and therapeutic algorithms are mainly based on expert opinion. Nevertheless, they are useful in the management of various syndromes, despite the limitations and doubts that have been discussed in the corresponding sections. On the whole, the 2015 guidelines will be an invaluable help to improve the management of pericardial diseases. The limitations and controversial issues listed in Table 3 do not detract from its value. On the contrary, they should encourage further research on the disease in the near future.
CONFLICT OF INTERESTNone declared.
SEC Working Group for the 2015 ESC Guidelines for the Diagnosis and Management of Pericardial Diseases: Josep Guindo (coordinator), Manuel Anguita (coordinator), Joaquín Alonso, Joaquín Aznar, Jaume Francisco Pascual, María Dolores Martínez Ruiz, Beatriz Ordóñez, Juan Quiles, and Gabriel Vázquez.
Expert Reviewers for the 2015 ESC Guidelines for the Diagnosis and Management of Pericardial Diseases: Gonzalo Barón Esquivias, Vivencio Barrios Alonso, Juan Cosín Sales, Covadonga Fernández-Golfín Lobán, José María Gámez Martínez, Xavier García-Moll Marimón, Luis Jiménez Borreguero, Eva Laraudagoitia Gorostiza, Federico Lombera Romero, Ana Peset Cubero, Tomás Ripoll Vera, and José Angel Rodríguez Fernández.
SEC Guidelines Committee: Manuel Anguita (chairman), Ángel Cequier, Fernando Alfonso, Lina Badimón, José A. Barrabés, Ignacio Fernández Lozano, José Juan Gómez de Diego, Luis Rodríguez Padial, José Alberto San Román, Pedro-Luis Sánchez, Juan Sanchis, and Alessandro Sionis.
SEC Working Group for the 2015 ESC Guidelines for the Diagnosis and Management of Pericardial Diseases, Expert Reviewers for the 2015 ESC Guidelines for the Diagnosis and Management of Pericardial Diseases, and SEC Guidelines Committee.