In line with the Spanish Society of Cardiology (SEC) policy1 on clinical practice guidelines, we present this article on the new, important, and contentious points of the 2016 European Society of Cardiology (ESC) guidelines on cardiovascular disease prevention in clinical practice.2,3
METHODSThe SEC Guidelines Committee and the coordinators who were assigned to these guidelines selected a group of expert cardiologists to review the ESC guidelines published at the end of May. The aim was to comment on the nature and appropriateness of the guidelines, analyze the methodology, and highlight the new, positive, contentious, or undiscussed points. These evaluations were used to develop a joint document, which was further assessed by cardiologists appointed by the SEC Sections of Cardiovascular Risk, Ischemic Heart Disease, and Clinical Cardiology.
GENERAL COMMENTS AND ANALYSIS OF THE GUIDELINESThese guidelines form the sixth review and involve 10 scientific societies and invited experts. The structure of the guidelines is similar to that of previous versions4 and aims to address the core questions:
- 1.
What is cardiovascular disease prevention?
- 2.
Who will benefit from prevention? When and how to assess risk
- 3a.
How to intervene at the individual level: risk factor intervention
- 3b.
How to intervene at the individual level: disease-specific intervention
- 3c.
How to intervene at the population level
- 4.
Where to intervene at the individual and population level
Each section begins by summarizing the key messages and ends with the remaining knowledge gaps. The guidelines use the well-known levels of evidence (A,B, and C) and classes of recommendation (I, IIa, IIb, and III). The GRADE recommendation system of the previous guidelines has been removed.
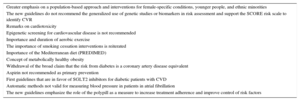
This article includes 2 tables to aid understanding: Table 1 summarizes the newest points and Table 2 summarizes the contentious points of the new guidelines.
New and Important Aspects
| Greater emphasis on a population-based approach and interventions for female-specific conditions, younger people, and ethnic minorities |
| The new guidelines do not recommend the generalized use of genetic studies or biomarkers in risk assessment and support the SCORE risk scale to identify CVR |
| Remarks on cardiotoxicity |
| Epigenetic screening for cardiovascular disease is not recommended |
| Importance and duration of aerobic exercise |
| The importance of smoking cessation interventions is reiterated |
| Importance of the Mediterranean diet (PREDIMED) |
| Concept of metabolically healthy obesity |
| Withdrawal of the broad claim that the risk from diabetes is a coronary artery disease equivalent |
| Aspirin not recommended as primary prevention |
| First guidelines that are in favor of SGLT2 inhibitors for diabetic patients with CVD |
| Automatic methods not valid for measuring blood pressure in patients in atrial fibrillation |
| The new guidelines emphasize the role of the polypill as a measure to increase treatment adherence and improve control of risk factors |
CVD, cardiovascular disease; CVR, cardiovascular risk.
Debatable or Unresolved Aspects
| Limited evidence on younger people, women, the elderly, and ethnic minorities, who are underrepresented in clinical trials |
| Doubt regarding the most appropriate duration and type of cardioprotective strategy to be applied in patients who have received chemotherapy |
| Although female-specific conditions are described, the guidelines lack a more in-depth assessment on the differences between men and women |
| More studies are needed on the safety of smoking cessation methods |
| Economic analysis of the implications of statin treatment in low or moderate CVR patients |
| Doubts over the protective effect of wine polyphenols |
| Indications and uses of PCSK9 inhibitors |
| Coronary artery disease screening in diabetic patients |
| Guidelines do not reflect the results of the SPRINT trial (randomized trial of intensive vs standard BP control). This was published in the same edition (26 November 2015) of the New England Journal of Medicine as the clinical trial on empagliflozin in diabetic patients (IIa recommendation in these guidelines) |
| Multidisciplinary BP control units are not discussed |
| Description of the barriers to implementing the guidelines: little time for seeing each patient, large number of existing guidelines (no comment on whether frequency also increases confusion), and unrealistic targets for control of risk factors |
BP, blood pressure; CVR, cardiovascular risk.
Cardiovascular disease (CVD) prevention is defined as a coordinated set of actions, at the population or individual level, that aim to eliminate or minimize the impact of CVD. Compared with the 2012 guidelines, this version places greater emphasis on a population-based approach, disease-specific interventions, and interventions in women, younger people, and ethnic minorities.
The guidelines explain that more than half of the reduction in cardiovascular mortality seen over the past 30 years is attributable to better control of cardiovascular risk factors (CVRF), in particular cholesterol (statin use), blood pressure (BP), and smoking. Such measures are especially beneficial if directed at high cardiovascular risk (CVR) individuals, although targets are unmet in a high proportion of patients.5
WHO WILL BENEFIT FROM PREVENTION? WHEN AND HOW TO ASSESS CARDIOVASCULAR RISK. SECTION 2Cardiovascular risk estimation remains based on the Systemic Coronary Risk Estimation (SCORE) tables.6 The cutoff points that classify a country, such as Spain, as “low risk”, are based on data from 2012 on adjusted CVD mortality rates for the age range 45 to 74 years (< 225/100 000 men and < 175/100 000 women).
The guidelines highlight the concept that absolute risk reduction is greater in individuals with a higher baseline risk, while recognizing that most cardiovascular events occur in the intermediate CVR patient group, who are more numerous. Risk reduction strategies must be complemented by public health measures.
Despite limited evidence, the guidelines recommend a systematic strategy of cardiovascular risk assessment for individuals at high risk (class I level C). This includes those with a family history of premature CVD, familial hyperlipidemia, major CVRFs (smoking, hypertension, diabetes mellitus, or dyslipidemia), or comorbidities that increase CVR. An opportunistic approach when patients visit their physician for other reasons is not recommended. Such assessment should be repeated at least every 5 years, and more often when the values are close to those requiring treatment.
In individuals with no known CVRFs, systematic CVR assessment may be considered (class IIb recommendation) in men older than 40 years and women older than 50 or who are postmenopausal.
Since 2003, the guidelines have recommended the use of SCORE tables, which predict 10-year cardiovascular mortality in the asymptomatic population. However, they recognize the limitations of SCORE and present other CVR assessment systems, such as the Pooled Cohort Studies Equations risk calculator, proposed in the 2013 AHA/ACC guidelines on CVR,7 which allow estimation of total cardiovascular events.
The risk categories have changed slightly compared with previous guidelines. There are 4 categories, according to the SCORE result: “very high CVR” (≥ 10%), which generally requires drug treatment; “high CVR” (5%-10%), which requires lifestyle modification and occasionally drug treatment; “moderate risk” (1%-5%), which requires lifestyle advice, and “low CVR” (< 1%).
Family History and GeneticsSystematic genetic studies are not recommended. A family history of premature CVD increases the individual's risk, though it may be difficult to determine if this is due to a genetic component or a common environment. Either way, information on family history is easy to obtain, although the guidelines acknowledge that the application of such information is complex.
Biomarkers and Cardiovascular Imaging TechniquesThe new guidelines discourage the generalized use of biomarkers and imaging and adhere to the SCORE system to identify CVR. Routine use of biomarkers is not recommended due to their lack of added value; no distinction is made between the different types of biomarker. There is a short section on imaging techniques and their role in further quantifying CVR; the information on their predictive capacity for cardiovascular events is inconsistent, and the economic implications of their use require assessment. Specifically, coronary artery calcium scoring with computed tomography has a class IIb recommendation in these guidelines (compared with IIa in previous guidelines). Such recommendations are in line with the latest American guidelines,7 which reserve imaging for intermediate-risk situations, with some limitations.
Clinical Conditions Affecting Cardiovascular RiskModerate chronic kidney disease (CKD) confers a high CVR classification, and severe CKD (glomerular filtration rate < 30mL/min/1.73 m2) confers a very high CVR.
There is call for increased recognition of chemotherapy-induced cardiotoxicity, and cardioprotective measures are proposed. Patients with heart disease or existing increased CVR are the most likely to develop cardiotoxicity. The guidelines propose early diagnosis using a combination of longitudinal strain techniques on echocardiography and biomarkers such as troponin. Gaps in knowledge include the most suitable type of cardioprotective therapy and the timing of cardiotoxicity screening, given the possibility of late onset complications. In Spain, we must look at how to apply these recommendations. The SEC has already voiced its opinion and considers cardiotoxicity detection to be a quality criterion with added value.8
Relevant GroupsWithin the risk assessment section, there is a new section aimed at addressing the persistent gaps in evidence.
Younger Individuals (Younger Than 50 Years)The main message regarding younger people is to identify patients with low absolute risk but high relative risk; the guidelines recommend the use of a risk age calculator or a lifetime risk calculator.
In younger at-risk individuals, information on CVRFs should be obtained; the specific age at which to begin this is not definitive, although 40 years is suggested. While the guidelines advise on the main CVRFs, they do not specify which methods are the most effective in this population. In fact, the section concludes that the approach to poorly-controlled risk factors should be the same as in older patients.
Elderly IndividualsThere is continued discussion on the significance of age as a dominant factor in CVR assessment. Assessment based on absolute risk reduction is accepted, but the various recommended risk scales do not take into account quality of life or potential years of life gained.
WomenA new section summarizes the evidence on female-specific conditions and their association with CVD. The obstetric subsection describes the importance of preeclampsia and the associated increase in CVR and future occurrence of hypertension and diabetes mellitus. It also explains the need to follow-up women who have premature infants, as there may be increased future CVR, probably related to an increase in hypertension and diabetes mellitus. The section describes gestational diabetes and its association with the future development of diabetes mellitus; periodic measurement of fasting glucose or glycosylated hemoglobin is recommended. The nonobstetric subsection focuses on polycystic ovary syndrome: follow-up is recommended due to the possible onset of diabetes mellitus and premature menopause.
Ethnic MinoritiesThis section of the guidelines focuses on the growing immigration in various parts of the world. The guidelines provide a detailed description on the differences in CVD occurrence in different areas. They go on to recommend the use of SCORE risk assessment in general, but with an additional adjustment for increased or decreased risk in comparison with the individual's current country of residence. For example, for native South Americans, risk is reduced by 30%. These correction factors can only be used in first-generation immigrants and do not apply to the children of immigrants.
HOW TO INTERVENE AT THE INDIVIDUAL LEVEL: RISK FACTOR INTERVENTION. SECTION 3ABehavior ChangeThe evidence is unchanged for cognitive-behavioral strategies and multimodal interventions with a class I level A recommendation for involving patients in their disease management. The recommendation that health care professionals be involved has increased from class IIa to class I, with level A evidence. As with previous guidelines, the question arises of how best to apply such guidelines given the lack of adequate specific training and the current pressures in the health care setting.
Psychosocial FactorsThere is new evidence (class IIa level A) on the treatment of psychosocial risk factors, and it is recommended to refer for treatment if the psychosocial risk factor is a diagnosable disorder (eg, depression) or if risk factors could worsen the classic CVRFs. There is still no evidence on the effect of anxiety on CVD.
Physical ExerciseThere are some small changes in the evidence and new concepts on physical exercise. The guidelines focus less on the known beneficial effects and pathophysiology, with a more practical focus on exercise training.
The guidelines continue to recommend aerobic exercise, whether with specific types of exercise (eg, swimming, running) or with everyday activities. To define exercise levels, intensity is expressed in terms of absolute intensity (MET) or relative intensity (effort level). Relative intensity refers to the percentage of maximum heart rate, the perceived exertion (Borg scale), or frequency of breathing (level of exercise that does not impede speaking).
Exercise duration recommendations (class I level A) are unchanged from previous guidelines, although the units have changed from hours per week to minutes per week. Recommendations are for 150minutes per week of moderate-intensity (activities such as golf, tennis doubles, cycling, gardening, and brisk walking) or 75minutes of high-intensity exercise (activities such as race-walking, running, tennis singles, higher-speed cycling, heavy gardening, and swimming).
For additional benefits, a longer duration is suggested, of 300minutes per week of moderate intensity or 150minutes per week of high-intensity or a combination of the two (class I level A). Sessions are recommended to last at least 10minutes, particularly for those unable to exercise for prolonged periods (class IIa level B). Exercise should be taken every day, and at least 3 to 5 times per week.
The guidelines place new importance on muscular strength physical activity and neuromotor activity (eg, agility, balance, coordination). However, they contain no evidence on the recommended quantity or the long-term prognostic effects on CVD. Interval training and high-intensity training are not yet recommended, until further studies are conducted.
There are new recommendations on medical evaluation prior to the start of physical activity. For the healthy low-CVR population, only a basic clinical evaluation is required (class I level C). Exercise testing should be considered for sedentary individuals with risk factors who want to start a vigorous physical activity or sport (class IIa level C).
A class I level B recommendation suggests regular assessment and counselling by medical professionals to encourage patient engagement.
Smoking InterventionThe most cost-effective measure for CVD prevention is stopping smoking. Cardiovascular risk increases even with low levels of smoking, passive smoking, and other forms of tobacco consumption (pipe, water pipe, “light” cigarettes, etc), therefore such situations should not be a reason for the patient or physician to ignore or avoid smoking cessation advice. After myocardial infarction, early and ongoing intervention is important to avoid relapse.
Despite a small decrease in smoking in Europe, mainly in adult men, smoking rates have increased in women and socially disadvantaged individuals, including adolescents.
The evidence has been updated on the efficacy and safety of drugs such as bupropion and varenicline, and these drugs are recommended alone or in combination (class I level A). Varenicline appears to be more effective than bupropion or nicotine replacement therapy.
Electronic cigarettes are a new addition to the guidelines: evidence on their effectiveness in smoking cessation is limited, and moderate at best, although they may be considered as a risk reduction strategy in some individuals while more robust results are awaited.
The guidelines contain is a specific section on population strategies. Adolescence is the most vulnerable period for starting smoking, and applying high levels of tax to all tobacco products is the most effective method to reduce the numbers of new young smokers. Tobacco smoke must be restricted due to the solid evidence on its damaging effects, as should electronic cigarettes due to the uncertainty over their effects and safety. Neutral packaging is effective, and advertising, promotions, and sponsorship restrictions are recommended. The goal of such common European measures would be to achieve a smoke-free Europe by 2030.
Nutrition and ObesityThe recommendations on diet type prevail. The Spanish PREDIMED trial9 has helped strengthen the evidence that the Mediterranean diet is the most heart-healthy, and the DASH diet is advocated for hypertensive patients. There is still no evidence on the use of vitamin supplements. In addition, the lower limit of healthy body mass index (BMI) is set at 20kg/m2; the upper limit remains at 25.
A daily fiber intake of more than 7g and 10g is shown to be associated with a 9% and 16% lower risk of stroke and coronary artery disease, respectively. There is evidence (from meta-analyses) that a regular intake of fruit and vegetables (5 pieces per day) and walnuts or mixed nuts (30g/d) reduces CVR, although there are no data from randomized control trials. There is also evidence from prospective studies on CVR reduction with a weekly intake of fish, attributed to the omega-3 fatty acid content, although 3 randomized trials have shown negative results.
One of the most remarkable aspects of the guidelines is the doubt cast regarding alcohol consumption, contrary to the potential benefits in CVR reduction from red wine polyphenols. An analysis of 59 epidemiological studies showed that the lowest level of CVR is observed in those who abstain from alcohol, and that any quantity of alcohol consumption is associated with increased BP and BMI.10.
Body WeightThe guidelines highlight that in individuals younger than 60 years, all-cause mortality is lowest when BMI is between 20 and 25. A healthy weight in elderly people is higher than the healthy weight of younger patients and other adults.
The guidelines reflect on the growing interest around the concept of the metabolically healthy obese phenotype. They explain that there is a subgroup of obese individuals that are resistant to metabolic complications such as hypertension and insulin resistance; however, individuals with metabolically healthy obesity have a higher risk of all-cause mortality than those with a healthy weight.11 The long-term results suggest that metabolically healthy obesity is a transition phase toward glucometabolic abnormalities rather than a specific clinical state.
Diet, exercise, and lifestyle changes remain the cornerstone for weight control, despite a lack of long-term success. Orlistat and bariatric surgery are still recommended as alternatives.
Lipid ControlIn 2016, new guidelines will be published on dyslipidemia; these will be analyzed in a separate article. The most contentious new point in those guidelines is likely to be the advised 50% reduction in low-density lipoprotein cholesterol (LDL-C), going beyond the targets of < 70mg/dL in very high-risk patients or < 100mg/dL in high-risk patients: this could mean LDL-C concentrations of as low as 35 to 50mg/dL. For the rest of the population, LDL-C levels of < 115mg/dL are advised.
Although these levels have been shown to be safe in both the IMPROVE-IT trial and studies on PCSK9 inhibitors, physicians should be prudent until more information is available. For statins or ezetimibe, each 1 mmol reduction in LDL-C lowers the relative risk of a CV event by approximately 20% to 22%. Also, as shown in the meta-analysis by Boekhold et al.,12 there may be an even greater risk reduction with values below 50mg/dL. It is still unknown whether PCSK9 inhibitors will have similar effects.
Type 1 and 2 Diabetes MellitusA multifactorial approach is essential. The widespread claim that all diabetic patients have a CVR similar to that of coronary patients has been withdrawn, as the initial phases of type 2 diabetes mellitus cannot be considered a coronary disease risk equivalent.
The guidelines reaffirm the need for early glycemic control; the general aim is for glycosylated hemoglobin (HbA1c) of < 7%. Strict control is not advised for frail or elderly patients, or those with established CVD but otherwise (and provided there are no hypoglycemic episodes) a target of HbA1c < 6.5% may be considered. Regarding drug therapy, the guidelines echo the study results of noninferior cardiovascular safety of various dipeptidyl peptidase 4 (DPP4) inhibitors and glucagon-like peptide 1 (GLP1) receptor agonists. However, saxagliptin increased the rate of hospitalization for heart failure, and the lack of additional cardiovascular benefits from such agents is stressed. Metformin is considered the first-line therapy. An important update is the recommendation (IIa) of sodium-glucose cotransporter 2 (SGLT2) inhibitors for patients with type 2 diabetes mellitus and associated CVD. These are the first guidelines to recommend SGLT2 inhibitors for diabetic patients with CVD, suggesting a class effect, though this could be debated.
Recommendations on blood pressure control are similar to previous recommendations, with a general target of < 140/85mmHg. A recent meta-analysis identified a group of young patients in whom a target of < 130/80 reduced morbidity but not mortality.
In line with the American societies, the guidelines on lipid control suggest a cutoff of 40 years after which taking statins is beneficial. Although this is a new recommendation since the 2012 guidelines, the evidence that it is based on is unchanged, making the current class I recommendation surprising.
Primary prevention with aspirin is not recommended. Microalbumin measurement is advised to identify which patients should be started on renin-angiotensin inhibitors. The guidelines do not discuss the role of coronary artery disease screening in individuals with type 2 diabetes mellitus.
There is a specific section on type 1 diabetes mellitus, describing the different pathophysiology to type 2 diabetes mellitus. However, the targets and general focus are very similar. The only difference is a target BP of < 130/80mmHg.
HypertensionThere are no substantial changes in the field of hypertension. In the general recommendations, some evidence levels have been reviewed and changed and there are slight modifications to some aspects.
Regarding office BP measurement, BP values should be verified with “at least 2 BP measurements per visit and on at least 2 visits” (the 2012 guidelines stated “several times, on several separate occasions”). If BP is only mildly elevated, this should be followed up over several months. Blood pressure should preferably be measured at the arm. A new point specifies that automatic methods are invalid for patients in atrial fibrillation. The diagnostic roles of ambulatory blood pressure measurement (ABPM) and home blood pressure measurement (HBPM) are described as complementary, not competitive, and the value of night-time BP measurements in predicting events is noted. Devices should be calibrated periodically, ideally every 6 months. Carotid Doppler, ankle-brachial index, and pulse wave velocity measurement are not recommended as additional investigations.
The decision to treat must be based on both BP levels and total CVR measured using SCORE (as in 2012). We are reminded that assessment of target organ damage, including subclinical damage, is highly useful, particularly with intermediate SCORE values (1%-4%).
Treatment recommendations are similar to previous guidelines. In the decision to start early pharmacological treatment, the guidelines stress the importance of risk stratification, although in grade 3 hypertension, early pharmacological treatment is essential independently of risk level. For patients older than 60 with a systolic BP ≥ 160mmHg, the target BP should be 140 to 150mmHg.
Antiplatelet TherapyAntiplatelet Therapy in Patients Without Cardiovascular DiseaseIn this section, the main message is clear and unchanged from previous guidelines: “Antiplatelet therapy is not recommended in individuals free from CVD due to the increased risk of major bleeding”. Four large trials are ongoing, 2 in diabetic patients (ASCEND, NCT02358343 and ACCEPT-D, Current Controlled Trials ISRCTN48110081), 1 in elderly patients (ASPREE, NCT01038583), and 1 in intermediate-risk patients (ARRIVE, NCT00501059). These will provide important information over the next 5 years.
Antiplatelet Therapy for Patients With Cardiovascular or Cerebrovascular DiseaseBased on the results of the PEGASUS-TIMI 54 trial and the DAPT study, a class IIb level A recommendation has been assigned to prolonged dual antiplatelet therapy beyond 12 months. The balance between ischemic risk and hemorrhagic risk must always be considered.2 Of interest, the guidelines do not specify the recommended dose of ticagrelor for this indication.
Early stopping (between 3 and 6 months) of P2Y12 inhibitors may be considered after drug-eluting stent implantation in patients with high risk of hemorrhagic stroke (IIb A).
For patients with stable coronary artery disease, the previous recommendation has been qualified: prasugrel is not recommended for patients with stable coronary artery disease. Ticagrelor is not recommended for patients with stable coronary artery disease except those with a history of acute coronary syndrome and low bleeding risk.
Last, the guidelines comment on the role of vorapaxar2 in secondary prevention in patients with established CVD: its systematic use as secondary prevention is not recommended, in line with the results of the TRA 2P-TIMI 50 trial.
Adherence to MedicationThis section is practically unchanged, other than the statement on role of the polypill, which may be considered (IIb B) as a means to increase treatment adherence and improve control of CVRFs.13
In the section on the cost-effectiveness of prevention, the guidelines highlight the limitations of current studies, which are mostly based on simulations rather than clinical trials or real life.
HOW TO INTERVENE AT THE INDIVIDUAL LEVEL: DISEASE-SPECIFIC INTERVENTION. SECTION 3BThe web addenda of the new guidelines explain the specific recommendations for patients with atrial fibrillation, coronary artery disease, heart failure, and peripheral arterial disease.
HOW TO INTERVENE AT THE POPULATION LEVEL. SECTION 3CThis new section reflects the aim that the guidelines should provide stakeholders with evidence-based suggestions to create a social environment that promotes healthy lifestyle choices as the default. Such modification of the social environment is wide-ranging, from local interventions to national and international policies. The guidelines highlight the responsibility of health professionals to take an active role in advocating such evidence-based interventions at the population level.
The recommendations center on promoting a healthy lifestyle and are divided into 5 main groups: diet, physical activity, smoking, alcohol abuse protection, and healthy environment (environmental pollution). Although the recommendation levels follow the same format as the rest of the ESC guidelines, their basis differs (the highest recommendation level corresponds to “consistent findings from several high-quality studies”, and not necessarily robust randomized clinical trials).
The dietary measures proposed include promoting production of and access to healthy products, legislative regulation of potentially harmful contents and advertising aimed at vulnerable populations, economic incentives using pricing policies, and the creation of healthy environments (school, work).
New importance is given to physical exercise. The guidelines assert that physical activity should be promoted at a population level with specific policies starting in childhood. The main messages are that regular exercise is recommended for men and women throughout life for at least 150minutes per week if moderate-intensity and 75minutes if vigorous-intensity. In childhood, a minimum of 30minutes and preferably 60minutes per day of exercise should be encouraged in schools, and availability of spaces and equipment for this should be increased (class I recommendation). Breaks between academic classes should be considered, integrating exercise into the everyday timetable, for example with supervised walking routes to get to school (class IIa recommendation). Similar measures are recommended in the workplace for the adult population.
The recommendations work on the idea that small changes in population CVRFs lead to a greater reduction in the disease burden than large changes in high risk individuals only.14
WHERE TO INTERVENE AT THE INDIVIDUAL AND POPULATION LEVEL. SECTION 4The message is clear: in all places, situations, and environments in society and in all health care settings, from primary care to hospitals.
A class I recommendation places emphasis on the role of the general practitioner as a motivator and coordinator, along with the important role of nurses and other health professionals. Prevention should be seen as a continuous lifelong process and all patients should be considered for specialized prevention programs. Of note are the barriers to implementing these guidelines, which include the time for seeing patients, the large number of existing guidelines (there is no comment on whether their frequency also increases confusion), unrealistic targets for control of risk factors, and lack of knowledge regarding risk assessment.
The guidelines state that all patients with an acute cardiac event or unstable heart failure should undergo a cardiac rehabilitation program, with a class I level A recommendation. Likewise, all stable patients are recommended to undergo a preventative program to improve prognosis (I B). This may involve making use of existing programs and new methods and technologies, always in the context of a multidisciplinary team, and starting prevention as soon as possible after an event (IIa).
The guidelines recognize the need for more investigation on the components of optimal intervention and cost-effectiveness analysis of these. A new addition is the description of home-based rehabilitation and telerehabilitation programs.
CONFLICTS OF INTERESTNone declared.
SEC Working Group for the 2016 ESC Guidelines on Cardiovascular Disease Prevention in Clinical Practice: Vicente Arrarte, Alejandro Berenguel, Carlos González Juanatey, Jesús María de la Hera, Iñaki Lekuona, Domingo Marzal, Rafael Peñafiel Burkhardt, and Félix Valencia Serrano.
Expert Reviewers for the 2016 ESC Guidelines on Cardiovascular Disease Prevention in Clinical Practice: Joaquín Alonso Martín, Vivencio Barrios Alonso, Raquel Campuzano Ruiz, Almudena Castro Conde, Juan Cosin Sales, Regina Dalmau González-Gallarza, Carlos Escobar Cervantes, José Julio Jiménez Nacher, Pilar Mazón Ramos, Sergio Raposeiras Roubin, and Fernando Worner Diz.
SEC Guidelines Committee: Alberto San Román, Fernando Alfonso, Fernando Arribas, Arturo Evangelista, Ignacio Ferreira González, Manuel Jiménez Navarro, Francisco Marín, Leopoldo Pérez de Isla, Luis Rodríguez Padial, Pedro Luis Sánchez Fernández, Alessandro Sionis Green, and Rafael Vázquez García.
SEC Working Group for the 2016 ESC Guidelines on Cardiovascular Disease Prevention in Clinical Practice, Expert Reviewers for the 2016 ESC Guidelines on Cardiovascular Disease Prevention in Clinical Practice, and the SEC Guidelines Committee.