The present article summarizes the main novelties in the recently published cardiovascular disease prevention guidelines of the European Society of Cardiology (ESC),1 comparing them with the previous recommendations2 and examining both their positive aspects and those that may be controversial. In addition, we comment on their applicability to routine clinical practice, taking into account the socioeconomic characteristics of Spain. We do not seek to contradict the recommendations, drafted by experts in the field of cardiovascular prevention, but to analyze and explain their possible implications in our country. At the suggestion of the Guidelines Committee of the Spanish Society of Cardiology (SEC) and the coordinators assigned to this document, a group of expert cardiologists was selected to thoroughly review the new guidelines.
COMMENTS ON THE METHODOLOGYThe guidelines follow a similar structure to that of previous years and attempt to address both the primary and secondary prevention of cardiovascular diseases. Under this ambitious plan, with numerous fields and sections, the authors frequently consider recommendations already detailed in previous specific guidelines, such as those on dyslipidemia,3 antiplatelet therapy,4 and arterial hypertension.5 Although the new guidelines may sometimes be repetitive and do not provide novel data, this approach is necessary to maintain consistency among all of the recommendations. It is also true that the new guidelines, with the novel risk scales SCORE2 and SCORE2-OP, are an innovative attempt to better estimate the cardiovascular risk (CVR) of individuals with cardiovascular risk factors (CVRFs) but without cardiovascular events (CVEs). The term “autoimmune diseases” has been replaced by “inflammatory conditions”. Of these, rheumatoid arthritis is the disease with the strongest link to CVEs, increasing CVRFs by 50% beyond established risk factors. Indeed, the periodic assessment of total CVR in these patients is a new class IIb recommendation. However, the authors do not explicitly state what type of screening should be applied to this population and do not discuss the need to establish a multidisciplinary approach involving cardiology and rheumatology. In addition, new concepts are added in an attempt to better explain the types of populations requiring prevention and their health status or disease state. Thus, the guidelines include the concepts of “apparently healthy people”, for people with CVRFs but without detected events, and of “metabolically healthy obesity”, for people with CVRFs in a transition toward glucometabolic abnormalities.
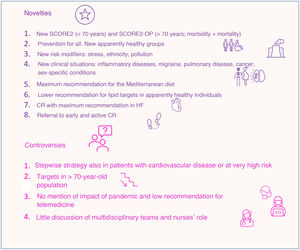
NOVELTIESAs the main novelties of the guidelines, we have selected the following 5 topics.
New risk rating scalesThe most influential modification of these guidelines is probably the recommendation for new risk algorithms, which replace the previous SCORE scale with the SCORE2 and SCORE2-OP. The categories of each individual are first defined to consider prevention, and people are then divided into 4 large groups: apparently healthy people, patients with established CVEs, patients with type 2 diabetes mellitus (DM), and patients with specific CVRFs, such as kidney failure and familial hypercholesterolemia. For the group of patients with CVRFs but considered apparently healthy,6 2 new algorithms are recommended: the SCORE2, for individuals aged between 40 and 69 years, which extends the risk calculation to morbidity and not just mortality, as in previous algorithms, and the SCORE2-OP, for those aged between 70 and 89 years, which takes into account specific factors related to their advanced age and estimates 5- and 10-year risk with adjustment for competing risk. In addition, different scales remain that depend on the risk of the different European populations, which varies from low CVR in countries such as Spain, moderate CVR in Central Europe, high CVR in Eastern Europe, and very high CVR in large parts of Asia and Northern Africa, based on cardiovascular mortality rates.
New potential risk modifiersNovel potential risk modifiers are considered. These factors are particularly important when an individual's risk is close to a decision threshold, for both increasing and decreasing individual CVR: stress and ethnicity (notable given the increasingly evident ethnic diversity in Spain). The risk multipliers range from 0.7 for southern Asian populations to 1.3 for Black African populations. Frailty is also included, with differentiation between advanced age and environmental exposure and with the first clear reference to air pollution. Other CVR markers were mentioned in the previous guidelines: psychosocial factors, family history, and imaging results, although ultrasound measurement of the carotid intima-media thickness, the ankle-brachial index, arterial stiffness, and echocardiography are not recommended to improve the CVR estimation.
New clinical sectionsThe new sections include atrial fibrillation, heart failure (HF), chronic obstructive pulmonary disease, inflammatory conditions, infections (HIV, influenza, and periodontitis), migraine, sleep disorders and obstructive sleep apnea, mental disorders, nonalcoholic fatty liver disease, and sex-specific conditions. This aspect is of particular interest, given the impact of all of these clinical situations on the assessment of total CVR.
Mental disorders were previously included as psychosocial risk factors. One novelty is the recommendation that mental disorders with significant functional impairment or with decreased use of health care systems be considered as influencing total CVR (class I). Thus, screening should be performed at each consultation, or at least periodically. However, the application of this recommendation in Spain, with our health care structure and overload, would require adaptation of the measures to the potential demand.
Also highlighted are data indicating that migraine is associated with higher risk of ischemic stroke and ischemic heart disease. In this regard, 2 new recommendations are established: migraine with aura should be considered in the CVR assessment (class IIa) and women with migraine with aura should avoid combined hormonal contraceptives (class IIb).
It must be highlighted that, under the title “Sex-specific conditions”, obstetric conditions (pre-eclampsia, hypertension, and gestational DM) are combined with nonobstetric conditions (polycystic ovary syndrome and premature menopause7) and erectile dysfunction. A new recommendation is included for women (class IIb): periodic screening of hypertension and DM should be considered in women with a history of preterm delivery or fetal death. In contrast, no mention is made of the possibility of systematically including obstetric history in the assessment of women. For men with erectile dysfunction, assessment of total CVR should be considered (class IIa).
As miscellaneous data, other conditions are mentioned. Atrial fibrillation is also associated with elevated risk of death, cardiovascular disease, and renal disease. It is a more powerful CVRF in women than in men. HF itself increases the risk of CVEs. For patients with cancer, the guidelines once again recommend monitoring of cardiac function with imaging techniques and biomarkers and recommend aerobic exercise to prevent cardiotoxicity. Chronic obstructive pulmonary disease is an established comorbidity for cardiovascular disease; however, its role as a RF for atherosclerotic cardiovascular disease is not clearly established. Sleep disorders are associated with higher CVR. It seems that 7hours sleep is optimal for cardiovascular health. Finally, screening of cardiovascular disease is recommended in all patients with chronic kidney disease.
Strengthening of lifestyle habit recommendations and proposed modificationsA healthy diet is the pillar of cardiovascular disease prevention (I A), and a Mediterranean or similar diet is recommended (new recommendation, I A). Recommendations with a high level of evidence (I B) remain: fruits, vegetables, nuts, cereals, and fiber. A new recommendation is added, that of limiting alcohol consumption to a maximum of 100g/wk, with even greater benefit indicated in nondrinkers. Loss of excess weight is critical for controlling CVRFs and reducing mortality. For this, the guidelines note the importance of energy restriction (but in healthy diets, such as the Mediterranean diet) and exercise. Drugs such as glucagon-like peptide-1 agonists (GLP-1a) may be beneficial, as well as bariatric surgery in selected patients (new recommendation, IIa).
Regarding physical activity, the guidelines continue to recommend 150 to 300minutes moderate-intensity aerobic exercise per week or 75 to 100minutes vigorous-intensity exercise per week to reduce morbidity and all-cause and cardiovascular mortality (I A). The authors note the importance of making every effort to combat sedentary behavior and that even repeated sessions of at least 15minutes help inactive patients to achieve cardiovascular benefits and lower mortality (new recommendation, I B). Moderate-intensity exercise is defined by the following: faster breathing that nonetheless permits conversation, a Borg scale score of 12 or 13, or a heart rate between 64% and 76% of the “maximum”. Resistance exercise is still recommended and there is a new role for instructional methods and activity trackers (wearables) in increasing physical activity (another new recommendation, IIa B).
Together with heart-healthy habits, the guidelines make new recommendations regarding psychological treatment (IIa B) and pharmacological therapy (IIa B) (selective serotonin reuptake inhibitors [SSRIs]) to treat anxiety and depression and to reduce CVEs and cardiovascular mortality in coronary heart disease patients. As an exception, the authors mention that patients with HF are not recommended to receive antidepressants due to increased all-cause mortality (III).
Strengthening of disease and risk factor recommendations and proposed modificationsThe guidelines follow the same recommendations as the 2019 guidelines on dyslipidemia,3 which are based on low-density lipoprotein-cholesterol (LDL-C) targets and the lipid-lowering therapy algorithm. The drug therapy of choice is still built around statins. They are complemented with ezetimibe and PCSK9 inhibitors to achieve therapeutic targets, and bempedoic acid is mentioned as an option, in combination with ezetimibe, for patients with statin intolerance; inclisiran is an alternative, with results on CVE outcomes expected. These guidelines highlight the role played by non–high-density lipoprotein-cholesterol, which is included in the new SCORE2 and SCORE2-OP scales.
No modifications have been made to the previous recommendations of the latest hypertension guidelines of the ESC,5 from 2018: special emphasis is placed on the advantages of rapidly and effectively reducing blood pressure, which hinges on lifestyle changes, starting with an initial combined treatment when drug therapy is required, which clearly improves the prognosis of hypertensive patients. The only novelty included in these guidelines is the clinical translation of beneficial effects throughout life of reducing blood pressure, applying the LIFE-CVD model based on the new risk tables SCORE2 and SCORE2-OP. These scales have been developed by the ESC and their inclusion for the assessment of CVR is one of the main contributions of these guidelines.
The novel sections include the new impact of pollution and environmental factors as CVRFs and their cost in lives. Recommendations have been added to avoid environmental exposure in areas with elevated pollution, including screening in regions of high pollution. In addition, noise is included as an environmental pollutant (>55dB at night) and the authors stress that governmental policies should aim to eliminate sources of pollution, such as traffic, power plants, heating, and industry.
Regarding the prevention of atrial fibrillation, the guidelines mention a paradigm shift in the approach to this condition, which can be found in the specific guidelines.8 Thus, the holistic management of patients via the “ABC” is still included in the current prevention guidelines and the importance is highlighted of the letter C, which refers to CVR and comorbidity optimization. The guidelines stress that the optimum control of all of these factors, already specified in other parts of the guidelines (eg, hypertension, obesity, alcohol consumption), can prevent the onset of atrial fibrillation.
The secondary prevention of stroke and transient ischemic attack should comprise antiplatelet agents for nonembolic events and anticoagulants for embolic events. In this regard, the blood pressure targets are about 130mmHg. Regarding peripheral vascular disease, the authors stress the usefulness of an ankle-brachial index ≤ 0.9 as a marker of vascular disease and CVRF. The recommendations are identical overall for patients but stress smoking cessation, physical exercise, particularly in patients with intermittent claudication, strict control of blood glucose levels in diabetic patients, and angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers in hypertensive individuals. All patients with peripheral arterial disease and intermittent claudication should also receive an antiplatelet agent and, in the case of DM, rivaroxaban 2.5mg/12h can be added, together with aspirin, as long as the bleeding risk is low (IIb B recommendation).
POSITIVE ASPECTSThe guidelines recommend different approaches to the risk estimation of apparently healthy people older than 70 years and younger people. In patients older than 70 years, given that there is a gradient of the association of CVRFs with CVEs that attenuates with age and a competing risk related to increased noncardiovascular mortality, the document recommends (class I) the use of the SCORE2-OP scale, which estimates 5- and 10-year fatal and nonfatal events adjusted by the risk of competing events. In this population, the thresholds for defining risk are higher, meaning that the group with very high CVR comprises individuals with a 10-year event estimation ≥ 15%, whereas the thresholds are ≥ 10% and ≥ 7.5% in individuals aged 50 to 69 years and those younger than 50 years, respectively. In addition, age is itself a CVRF.
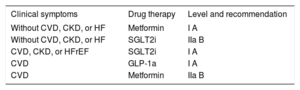
Patients with DM are automatically considered to have at least moderate CVR and may have high or very high risk depending on the associated CVRFs, target organ damage, duration of DM, and presence of chronic kidney disease or cardiovascular disease. Tirst-line drugs with proven cardiovascular benefits are recommended, such as sodium-glucose cotransporter 2 inhibitors (SGLT2i) and GLP-1a, separating them from drugs solely indicated to achieve metabolic control. Notably, this approach is somewhat closer to the therapeutic positioning of patients with type 2 DM of the SEC,9 in which SGLT2i and GLP-1a are first-line drugs and distinct from antidiabetic drugs. Changes are made to the pharmacological section for type 1 DM, with a dapagliflozin recommendation, but with consideration of the risk of ketoacidosis, and advice is consolidated regarding type 2 DM management (Table 1).
Advice on the pharmacological management of patients with type 2 diabetes mellitus.
| Clinical symptoms | Drug therapy | Level and recommendation |
|---|---|---|
| Without CVD, CKD, or HF | Metformin | I A |
| Without CVD, CKD, or HF | SGLT2i | IIa B |
| CVD, CKD, or HFrEF | SGLT2i | I A |
| CVD | GLP-1a | I A |
| CVD | Metformin | IIa B |
CKD, chronic kidney disease; CVD, cardiovascular disease; HF, heart failure; HFrEF, heart failure with reduced ejection fraction.
All of these recommendations are based on various clinical trials of type 2 DM with cardiovascular and renal targets and are captured in 2 meta-analyses including all of these trials.10,11
These guidelines very practically and simply summarize in a single table the main recommendations on the clinical management of hypertension, including its classification and diagnosis, the assessment of hypertension-mediated organ damage (previously called target organ damage), the thresholds for treatment initiation, blood pressure targets in the clinic, the management of both interventions regarding lifestyle changes, and the approach to total CVR in hypertensive patients.
Also present is the recommendation for smoking cessation, with brief advice and treatment with the available drugs, varenicline (safe when initiated in the hospital), bupropion, and nicotine replacement therapy. The use of electronic cigarettes is discouraged.
Cardiac rehabilitation programs receive a clear class I A indication and are now awarded a I A indication in all patients with HF to reduce hospitalization and mortality risk. The document also recommends that patients be actively, automatically, and promptly referred to rehabilitation programs, as well as the involvement of nursing staff and other professionals (IIa).
For the general population, we must note the inclusion of a new recommendation (I C) for the implementation of pollution reduction policies aimed at decreasing cardiovascular morbidity and mortality. This traditional focus is based on the prevention paradox, in which small shifts in the risk of disease in an entire population lead to greater reductions in disease burden than a large shift in high CVR individuals. There are 2 key ideas that were not found in the previous document. The aims of population-level interventions are to improve the health literacy of populations and to alter the social environment to modify CVRFs. Although population-wide lifestyle modifications are expensive, slow, and difficult to implement and maintain over time, they achieve long-lasting returns in terms of quality and quantity of life improvements. The authors also stress the need for governmental policies to reduce the intake of calories, salt, sugar, and saturated fat through both education and taxes and in all settings: in schools, workplaces, and the community. They also agree on the importance of informing consumers though nutrition labeling and information.
CONTROVERSIAL ASPECTSAlthough the inclusion of new potential modifiers with known involvement in risk is a positive development, they are difficult to assess and the guidelines provide little information regarding topics such as the individual cumulative exposure to pollutants and the measurement of their impact on CVR. Equally, although the evidence is clear on the relationship of body mass index, waist circumference, and waist-to-hip ratio with cardiovascular disease, no significant reclassification is provided in the risk tables. In addition, while there are promising data on the value of biomarkers such as lipoproteins in the assessment of CVR, more evidence is still required and the guidelines do not examine this aspect.
One of the most controversial topics is the strategy for achieving objectives; the authors propose a stepwise approach, with more relaxed targets at first and then, based on CVR or comorbidities, a more stringent target in the second step. The authors state that this stepwise strategy reduces secondary effects without compromising target achievement, leaving the possible combination of both steps in patients with very high CVR. As well as being controversial, the appropriate times and clinical pathways are not defined. Thus, these recommendations could lead to follow-up loss and a failure to achieve adequate targets in some patients.
The guidelines do not explore some aspects in depth. For example, different treatment groups are defined for dyslipidemias, such as women, for whom the same strategy for men is defended because no differences have been found with drug therapy. However, the authors do not address the need for lipid control related to possible obstetric conditions or inflammatory diseases, which are also more frequent in women and can modify CVR (figure 1).
No reference is made to cardiopulmonary exercise testing and its thresholds, a true gold standard in exercise prescription. In addition, the document does not specify the intensity levels or the effect of prolonged overtraining and their relationship with, for example, increased risk of atrial fibrillation.
As in other guidelines, very recent publications could not be considered in the recommendations, such as the results of the SSaSS study,12 presented at the ESC Congress 2021, which found clear cardiovascular benefit with sodium-reduced salt containing 25% potassium chloride, although there were some methodological limitations.
The guidelines consider (IIb A indication) the possible prescription of clopidogrel 75mg/d instead of aspirin, a recommendation recently strengthened by the outcomes of the HOST-EXAM trial, which compared long-term antiplatelet monotherapy (after initial dual antiplatelet therapy) with aspirin vs clopidogrel in more than 5000 patients.13 Although clopidogrel reduced ischemic and bleeding events vs aspirin, there were no differences in mortality. Another of the “questionable” recommendations (IIb C) is aspirin for patients without a history of myocardial infarction or revascularization but with evidence of coronary heart disease in imaging tests (mainly coronary angiotomography). Indeed, no mention is made of the value of the calcium score (whether absolute or as a percentage) as a guide. In addition, if applicable, it should be primarily considered in patients without high bleeding risk. This indication is not supported by any citation and readers are referred to the specific guidelines on chronic coronary syndromes, despite the existence of studies with controversial results.14 In individuals without atherothrombotic disease, particularly patients with DM and high/very high CVR, aspirin is recommended with level IIb A (in the absence of clear contraindications). The vast majority of studies referenced to support this change reach the same conclusion: aspirin reduces atherothrombotic events but increases bleeding risk. Accordingly, this latest recommendation should be followed with caution.15
Regarding the elderly population, in contrast to the 2019 ESC/EAS guidelines on dyslipidemia,3 the age limit is established at 70 years instead of 75. This limit must be put into context, because biological age is not per se the sole determinant of patients’ baseline status. Individuals older than 70 years with a 10-year risk of CVEs between 7.5% and 15% are already considered to have high CVR; for treatment selection, the factors considered must include frailty, polypharmacy, and patient preferences. These factors have a subjective component that is poorly defined in the guidelines and might depend more on the treating physicians’ and patients’ own criteria. Given that up to 70% of individuals older than 70 years have had at least 1 CVE and two-thirds also have noncardiovascular comorbidities, comorbidities and multimorbidity should be considered when targets are being established.16 The guidelines highlight some of the more frequent comorbidities in these patients, both cardiovascular and noncardiovascular (eg, depression and cancer). The authors mention that men have more cardiovascular disease-related comorbidities while women have more noncardiovascular comorbidities (particularly depression).17 The approach to these patients, underrepresented in clinical trials, is complex and the guidelines cannot give absolute directives on their management. Thus, the aspects requiring consideration include pharmacokinetics, life expectancy, and disease-disease, drug-disease, and drug-drug interactions. Other relevant aspects may be the socioeconomic level, geriatric syndromes, and life expectancy, which is why multidisciplinary teams are key to the improved management of these patients.18 The classification and management of CVR in people older than 85 years who also have frailty are controversial, due to the lack of data.
Miscellaneous aspects include various recommendations in different areas with many knowledge gaps. It remains unclear if periodontitis prevention or treatment improves clinical prognosis. Equally, the possible benefit of intermittent fasting requires more long-term studies, which is why no specific recommendations are made in this regard. In addition, there are no relevant data on the differential cardiovascular impact of alcohol consumption between men and women.
Surprisingly, the indication is just II B for cardiac telerehabilitation and home-based programs, particularly given that the guidelines do not mention the need for adaptation to the impact of the COVID-19 pandemic on the deteriorated control of CVRFs and on preventive methods in general or the unavoidable delaying of face-to-face care in multidisciplinary programs.
IMPLICATIONS FOR CLINICAL PRACTICE IN SPAIN AND THE LOCAL SOCIOECONOMIC CONDITIONSCVE prevention requires an integrated approach with contributions from various disciplines and specializations that work together and are focused on each patient and family. Progress is required to clearly determine the specific purview of each health care professional.
The previous guidelines considered wideranging evidence from multidisciplinary treatment and prevention programs to reduce CVR. These programs are coordinated by nursing staff, improve conventional medical care, and are adaptable to distinct health care contexts. Nurses are considered key to cardiovascular prevention. The authors also recognize the extensive evidence showing that multidisciplinary cardiovascular prevention programs coordinated by nursing staff are more effective than conventional medical care without multidisciplinary support and signal that these programs can be adapted to different health care contexts. The current guidelines award a IIa B indication to the consideration of methods to increase referrals to cardiac rehabilitation and prevention, electronic prompts or automatic referrals, and referral and liaison visits, as well as structured follow-up by nurses or health care professionals to rapidly initiate these programs after discharge. Adherence to cardiac rehabilitation programs is improved by the active involvement of nurses. Nurse-coordinated programs can increase efficacy, which is why, together with the commitment of families, they can improve the CVRF profile of coronary heart disease patients or individuals at risk of developing cardiovascular disease and of patients with HF, particularly those with reduced ejection fraction, within the multidisciplinary team strategy.19,20 However, the guidelines do not refer to the dose adjustment of drugs by nurses acting within a multidisciplinary team.
CONCLUSIONSThe new prevention guidelines contain some novelties that will change the clinical practice regarding CVR assessment in apparently healthy people. The SCORE2 evaluates morbidity and mortality and not just mortality and, in addition, the SCORE-OP is an improved and novel approach to CVR in patients older than 70 years. Regarding CVRF control and diseases requiring special preventive attention due to their higher CVR, numerous recommendations are made; some stress those that are already included in other guidelines and others represent slight changes. There is also space for more controversial recommendations, the stepwise approach, and some gaps in the evidence. Finally, cardiac rehabilitation receives the maximum recommendation and evidence, not only in ischemic heart disease, but also in HF, all considering the current health care stage.
FUNDINGNone.
CONFLICTS OF INTERESTThe conflict of interest declaration documents of all authors can be seen in the supplementary data.
SEC Working Group for the 2021 ESC guidelines on cardiovascular disease prevention in clinical practice: Vicente Arrarte (coordinator), Raquel Campuzano (coordinator), José Antonio Alarcón Duque, Guillermo Aldama, Vivencio Barrios, Clara Bonanad, Almudena Castro Conde, Rosa Fernández Olmo, José M Gámez, Gabriela Guzmán-Martínez, Carmen Neiro Rey, and David Vivas.
SEC Guidelines Committee: Pablo Avanzas, Gemma Berga Congost, Araceli Boraita, Héctor Bueno, David Calvo, Raquel Campuzano, Victoria Delgado, Laura Dos, Ignacio Ferreira-Gonzalez, Juan José Gomez Doblas, Domingo Pascual Figal, Antonia Sambola, Ana Viana Tejedor, José Luis Ferreiro (copresident), and Fernando Alfonso (copresident).