In 2011, the Spanish Society of Cardiology (SEC) established a specific modus operandi for dealing with European Society of Cardiology guidelines, which entailed publishing the original guidelines in Spanish together with a critical review.1 The critical review is prepared by a group of experts coordinated by the CGPC (Clinical Practice Guidelines Committee).
MethodologyA task force was formed consisting of experts from different fields. Members of the task force were proposed by the SEC Clinical Cardiology, Cardiac Catheterization, and Cardiac Imaging sections and by the SECTCV (Spanish Society of Thoracic and Cardiovascular Surgery). The Task Force was coordinated by 2 representatives of the CGPC. The guidelines were divided into blocks and sent to members of the Task Force, who analyzed the most novel and important aspects in terms of clinical practice. They also gave their opinion on the methodology used, possible areas of conflict, and limitations with regard to other guidelines. In addition, they were asked to describe the implications for actual practice in the Spanish setting. The information received was used to produce a first draft of the document, which the original committee evaluated before referring it to a second group of 11 reviewers also proposed by sections of the SEC and the SECTCV. All authors and reviewers were asked to disclose any conflicts of interest, details of which are provided at the end of the article.
Novel Aspects of the New GuidelinesThe most important and/or novel aspects of the guidelines identified by the task force were:
- 1.
The im portance of consensus decision-making and the establishment of the “heart team” as the cornerstone of diagnosis, prognostic evaluation, and decision-making on treatment.
- 2.
Confirmation of echocardiography as the key tool in diagnosing and quantifying the severity of valvular heart disease, and for prognostic evaluation. The wider use of echocardiography due to new technologies and its use in different situations was also noted.
- 3.
Developments in aortic stenosis (AS), which included a recognition that low-gradient, low-flow aortic stenosis (AS) with preserved ejection fraction constituted a new problem for clinical diagnosis, and modifications to surgical indications for asymptomatic AS.
- 4.
Changes in previous recommendations regarding aortic surgery.
- 5.
Developments in surgical indications for mitral regurgitation (MR).
- 6.
Indications on prosthesis types and antithrombotic therapy for patients with prosthetic valves.
- 7.
The incorporation of percutaneous techniques for selected cases of severe AS and MR.
These guidelines2 are an updated version of the previous 2007 document. They are very relevant for several reasons, including: a) the significant increase in patients older than 75 years with severe valvular heart disease who may benefit from different therapeutic options; b) the development of diagnostic methods and a better understanding of the natural history of the disease; c) discrepancies between clinical practice and guideline recommendations,3 and d) improvements in surgical outcomes and the consolidation of percutaneous treatment.
For the first time, the guidelines were prepared by a joint panel of cardiologists and cardiac surgeons (24 authors and 24 reviewers), which illustrates that one of the key objectives was to minimize differences of opinion. The methodology used was similar to that employed in previous guidelines, with tables summarizing the recommendations in each section (I, IIa, IIb or III) together with the weight of evidence (A, B or C) for each recommendation. The number of tables increased slightly, making it possible to include the methods and parameters used to define the severity of valvular heart disease (stenosis included in 2012), to update recommendations on catheterization for patients with valvular heart disease, and to include data on surgical mortality in Europe and America from 2004 to 2010.
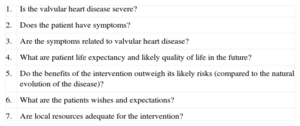
The Importance of Consensus Decision-MakingThe management of patients with valvular heart disease is frequently conditioned by information obtained from complementary tests, and information available to cardiologists is often redundant. The guidelines take a patient-centered approach based on 7 key questions (Table) that should be asked whenever an intervention is considered. The guidelines also promote the idea that decisions should be taken by a multidisciplinary team (the heart team) consisting of cardiologists, imaging experts, interventional cardiac surgeons, and anesthesiologists. The guidelines give less importance to surgical risk scores (EuroSCORE or STS [Society of Thoracic Surgeons]), which are increasingly challenged because of their tendency to overestimate risk, especially in severe cases.
Key Questions When Evaluating a Patient Referred for Valvular Intervention.
| 1. | Is the valvular heart disease severe? |
| 2. | Does the patient have symptoms? |
| 3. | Are the symptoms related to valvular heart disease? |
| 4. | What are patient life expectancy and likely quality of life in the future? |
| 5. | Do the benefits of the intervention outweigh its likely risks (compared to the natural evolution of the disease)? |
| 6. | What are the patients wishes and expectations? |
| 7. | Are local resources adequate for the intervention? |
Adapted from Table 3 of the European Society of Cardiology/European Association for Cardio-Thoracic Surgery guidelines on valvular heart disease.
Echocardiography is recognized as the patient assessment technique par excellence. However, the guidelines emphasize that decisions should not be based on any one parameter or threshold, but rather on an integrated approach to assessing the severity of lesions. In that sense, they follow the recommendations of the American and European societies of echocardiography (Tables 4 and 5 in the guidelines) and suggest that echocardiographic findings should be viewed within the context of the clinical situation. Echocardiography should be comprehensive (ie, it should cover chambers, valves, and aorta), combined (ie, it should use all available techniques – the guidelines incorporate 3-dimensional echocardiography and list specific indications for transesophageal echocardiography), and applicable in different circumstances (complex valve surgery and percutaneous intervention).
Specific recommendations include:
- •
Correlating ventricular dimensions with body surface, especially in patients of small stature.
- •
Use of different severity thresholds for secondary MR (regurgitant orifice area ≥20mm2 and regurgitant volume≥30mL) and primary MR (regurgitant orifice area≥40mm2 and regurgitant volume≥60mL).
- •
Defining a mean gradient>40mmHg as severe AS, as in the American guidelines.
Although stress echocardiography was included in earlier guidelines, the present document emphasizes its utility in evaluating ischemic MR (IIa C recommendation for patients with moderate MR indicated for bypass surgery) and suggests that it may be useful in asymptomatic primary MR (IIb C indication for surgery if pulmonary hypertension>60mmHg is present on exercise). Also included is the occasional use of stress echocardiography in mitral stenosis when there are discrepancies between severity and symptoms and in AS to document the behavior of the mean gradient.
Low Gradient, Low Flow Aortic Stenosis With Preserved Ejection FractionThis entity is particularly noticeable in older patients with a small left ventricle, severe hypertrophy, and hypertension. Its frequency appears to be overestimated, however, and the guidelines point out that some cases stem from technical limitations in calculating the aortic area and from the mismatch that arises when defining severe AS using mean gradient and transvalvular area. To generate mean gradients>40mmHg the areas must be closer to 0,8cm2. It is therefore paradoxical that the cut point was not modified; however, the guidelines point out the importance of carefully confirming the severity of the stenosis using other diagnostic methods before making any clinical decisions.
Surgical Indications in Asymptomatic Aortic StenosisAortic valve replacement is confirmed as the definitive treatment for severe AS. The indications for intervention in asymptomatic patients have been revised:
- •
There is a new IIa (B) indication for very intense stenosis using a maximum transvalvular speed of 5,5 m/s.
- •
The IIb indications have also been modified. Arrhythmias are no longer mentione d, but a new indication is introduce d for asymptomatic patients with low surgical risk and increased mean gradient>20mmHg on exertion, excessive lef t ventricular hypertrophy in the absence of hypertension, or repeated and markedly elevated concentrations of natriuretic peptides (evidence type C).
The criteria regarding the diameter of the ascending aorta at which surgery is indicated were changed. The previous guidelines recommended aortic surgery in Marfan syndrome when the diameter of the ascending aorta was ≥45mm. That diameter remains in effect only if there are risk factors (family history of dissection, aortic diameter increased ≥2mm/year, severe mitral or aortic insufficiency, desire for pregnancy). In other cases, surgery is now indicated at diameters ≥50mm:
- •
For patients with bicuspid valve and risk factors, the indication for surgery remains a diameter of 50mm.
- •
In other circumstances, surgery is indicated at diameters≥55mm.
In order to determine significant progression (dilation>2mm/year), images must be compared with those from earlier studies, while ensuring that measurement takes place at the same place and using the same methodology.
Although these changes are based on recent publications on the natural history of patients with bicuspid valve, it is uncertain whether the risk of aortic dissection is increased when severe valvular dysfunction is present. As previously recommended, replacement of the ascending aorta is indicated at diameters of >45mm when the indication for surgery is valvular heart disease.
Mitral RegurgitationThe first innovation in the guidelines is the use of a simplified etiological classification to distinguish between primary MR (organic, due to valvular heart disease) and secondary MR (functional MR). Although this classification seems more practical because the two entities require a different therapeutic approach, it should be noted that study findings in ischemic MR may not apply to nonischemic secondary MR, and vice versa.
Despite the absence of randomized studies comparing valve replacement surgery with a more conservative approach, the guide considers valve repair to be the surgical procedure of choice for symptomatic primary MR (indication IB). This recommendation is based on records showing lower operative mortality with repair surgery than with valve replacement.
Regarding the indications for surgery, the classic indication is maintained for symptomatic patients with ejection fraction>30% and end-systolic diameter<55mm. However, modifications have been introduced for asymptomatic patients and surgery is now considered an option in patients with normal ejection fraction, a high probability of effective repair, low surgical risk, and any of the following:
- •
Leaflet prolapse and end-systolic diameter>40mm (or >22mm/m2 in small-stature patients) (class IIa).
- •
Atrial size>60mm/m2 in sinus rhythm (class IIb).
- •
Pulmonar y hypertension on exertion (systolic pulmonar y artery>60mmHg) (class IIb).
The indication for surgery in patients with severe secondary MR and ejection fraction>30% who are scheduled for bypass surgery is still considered a class IC recommendation, but a recent meta- analysis4 has provided more consistent evidence regarding treatment. The guidelines therefore lean towards a preference for valve repair with restrictive annuloplasty, a technique that leads to lower operative risk but has a high recurrence rate (30%-50% at 3 years). The assessment and selection of candidates for surgery may, however, be improved by the inclusion in the guidelines of echocardiographic parameters that predict recurrence.
When considering surgery for secondary MR in symptomatic patients with seve re mitral regurgitation and ventricular dysfunction (ejection fraction<30%), and who are candidates for revascularization, the new guidelines emphasize the use of imaging techniques to demonstrate viability. The results of the STICH5 study led the authors to include a strong recommendation for surgery (class IIa C).
Tricuspid RegurgitationThe guidelines also include changes in surgical indications for tricuspid regurgitation:
- •
Severe, isolated tricuspid regurgitation in patients with mild symptoms and progressive deterioration of right ventricular function is now a IIa C indication.
- •
In patients undergoing left valve heart surgery, tricuspid repair is considered a type IIa C indication in those with mild tricuspid regurgitation when the annulus is dilated (>40mm or >21mm/m2).
One significant change is that the age at which a bioprosthesis is recommended over a mechanical prosthesis has been lowered. The IIa recommendation is now to use an aortic bioprosthesis in patients older than 65 years and a mitral bioprosthesis in those over 70 years. Both bioprostheses and mechanical prostheses are considered acceptable in patients aged 60 years to 65 years (aortic prosthesis) or 65 years to 70 years (mitral position), depending on individual patient factors. The increased use of percutaneous prosthesis implantation and the possibility of a bioprosthesis may be factors that explain this development. The new guidelines also emphasize a preference for bioprosthesis over mechanical prosthesis in the tricuspid position.
Also new is the recommendation to perform, as required, an enlargement of the aortic annulus to increase the size of the implanted prosthesis and prevent significant disparity of the prosthesis (defined as effective valve area <0,65cm2/m2).
The section on antithrombotic therapy is structured similarly to the 2007 guide, with some notable changes. A new table (Table 19 in the guidelines) summarizes the recommendations. Major developments include:
- •
A recommendation for concomitant treatment with acetylsalicylic acid and low-dose oral anticoagulant for patients with mechanical prostheses and arteriosclerosis.
- •
In the first 3 months after implantation of a mitral or tricuspid bioprosthetic, oral anticoagulant is recommended; acetylsalicylic acid is recommended in the case of aortic bioprostheses.
- •
Oral anticoagulation is also recommended for the first 3 months after mitral valve repair.
The guidelines explicitly recognize that the new oral anticoagulants (factor IIa or Xa inhibitors) are not indicated for patients with mechanical prostheses and that low molecular weight heparins may be useful for anticoagulation of mechanical prostheses. The guidelines also recognize, however, that the latter is not an accepted indication as it is based on observational series and no controlled trials have been performed. The guidelines also support the use of dual antiplatelet therapy in patients who have undergone transcatheter aortic valve implantation (TAVI) or percutaneous mitroplasty, although there is no evidence to indicate its exact duration.
Incorporating Percutaneous Treatment Options Into Clinic PracticeThe major update on the previous 2007 guidelines is that, for the first time, precise indications for TAVI are provided, based primarily on results from the PARTNER study.6 The new recommendations indicate that patients should only be treated in centers with cardiac surgery facilities and that patient selection should be carried out by a multidisciplinary or heart team. In patients with severe, symptomatic AS which is considered inoperable, TAVI is a IB indication; it is a class IIa B indication in patients at high surgical risk, as long as there is consensus within the heart team and the individual risk and anatomical factors are taken into account.
Alongside this major advance in the management of AS, in which TAVI appears to have become quite firmly established as a treatment option, there is also some support for percutaneous treatment using the MitraClip® in selected MR patients7. Although there is no explicit recommendation for this procedure in organic MR, it is considered a class IIb indication in high risk or inoperable patients with secondary MR.
Critical Evaluation of Contentious IssuesAs with previous versions, the main problem with the current guidelines is the lack of objective evidence to support the recommendations. Of the 68 recommendations included in the tables, none is backed by level A evidence and only 9 are supported by level B evidence. Fifty-nine (87%) of the recommendations are therefore the result of expert consensus, common sense, or historical trends in the field. This lack of references should definitely act as a spur for clinical research in valvular heart disease. For editorial reasons, no type III recommendations were included although these did appear in other guidelines.
One of the problems hindering implementation of the guidelines is that some of the terms used are not precisely defined. For example, excessive hypertrophy is mentioned but no values are provided for thickness or mass; significant prosthetic dysfunction is not defined and no criteria are provided on how the severity of AS should be determined in some complex cases (Table 9 of the guidelines).
Another difficulty is that recommendations are included without any clear justif ication in the text. For ex ample, coronar y revascularization is recommended (IIa C) for lesions between 50% and 70% and no justification is provided. The same is true for the recommendation (IIb C) to re-operate for prostheses without structural deterioration in patients undergoing surgery on another valve or coronary bypass. There are also some discrepancies when numerical parameters are provided and then not used in management algorithms. Examples include the definition of critical aortic stenosis (<0,8cm2) and the value for brain natriuretic peptide of >105 ng/mL in MR.
These limitations are particularly striking in the paragraph on antithrombotic treatment. In this case, observations are made in the text which are not included in any of the tables. Examples include the recommendation to use international normalized ratio (INR) self- management systems in patients undergoing anticoagulant therapy; the use of median INRs rather than INR range; anticoagulation recommendations according to type of prosthesis, location, and risk factors; and the lack of precision regarding when to interrupt anticoagulant treatment, or the role of low molecular weight heparins in these circumstances.
Although echocardiography is defined as the gold standard for evaluating valvular heart disease, a discussion of its limitations and problems of reproducibility was not included. This would have been useful, especially given the emphasis on quantitative approaches to decision making. The possibilities of new echocardiographic techniques (such as 3-dimensional echocardiography) and other forms of cardiac imaging are addressed only very briefly; it may have been helpful to provide specific recommendations for potential clinical problems. Magnetic resonance imaging (MRI) is only mentioned for tricuspid conditions and functional analysis of the right ventricle. Likewise, although computed tomography is mentioned as a means of ruling out coronary artery disease, there is little discussion of its usefulness as an alternative to coronary angiography, especially in nonelderly patients with valvular heart disease (mitral valve prolapse, bicuspid valve, etc.) and low calcification.8 Three-dimensional transesophageal echocardiography could help to quantify AS or provide additional information when assessing annular diameter before indicating TAVI, as well as during monitoring of the procedure. Both MRI and computed tomography can be useful in evaluating the ascending aorta, and the detection and quantification of myocardial fibrosis by MRI can provide prognostic information.
The latest recommendations suggest that surgery in patients with valvular heart disease should now be carried out earlier and/or when objective parameters indicate less severe ventricular involvement. This attitude is based on a better knowledge of prognostic factors and improvements in surgical outcomes. However, the need for strict quality control should be stated explicitly, as this is essential when performing surgery in asymptomatic patients. Extreme care is also required with TAVI, a novel technique whose medium-term results are not yet well-known.9 It is important to note that these guidelines do not distinguish between different types of bioprosthetic valves; this should be taken into account with certain age groups as there are differences in durability depending on the material used, the manufacturing process, and the methods used for conservation.
This 2012 version of the European guidelines still contains significant differences with respect to the latest version of the American guidelines,10 particularly as concerns mitral valve disease. The European guidelines continue to give less weight to echocardiography in the stratification of MR and place greater limits on its indication in mitral stenosis. The American guidelines differentiate between mitral stenosis approaches on the basis of functional class (II vs III-IV), reserve surgery for functional class III-IV, and consider valvuloplasty as an option even with areas>1,5cm2. The European guidelines, on the other hand, consider intervention (valvuloplasty or surgery) to be indicated when functional class≥II and area<1,5cm2. There are also noteworthy differences between the two sets of guidelines regarding the indication for surgery in asymptomatic patients with MR, as the American guidelines only require that the repair be feasible (IIa). The performance of a stress test in all asymptomatic patients with AS or the inclusion of specific indications for aortic annulus enlargement or use of the Ross procedure are included in the STS guidelines, but not in the European ones.11 Some institutions such as National Institute for Health and Clinical Excellence consider the evidence for the effectiveness of TAVI in high-risk patients who are candidates for surgery to be inadequate, in contrast to the view expressed by the European guidelines.12
Implications for Clinical Practice in SpainThe publication of a clinical practice guideline provides an opportunity for self-assessment by comparing daily practice with consensus recommendations. Opportunities for improvement can always be found. However, this is a complex issue and space is limited, so we have restricted our analysis to 4 distinct situations:
- •
Clinical Management of Valvular Heart Disease. Following the guidelines closely would require improvements in quality standards for clinical management and for echocardiographic assessment, with quantitative parameters. It would also be necessary to use available multimodal imaging resources with defined protocols to eliminate unnecessary or redundant imaging studies. The guidelines’ recommendation for yearly review in certain subgroups of patients with heart disease represents a major burden of care. Although cardiologists should take overall responsibility for patient management, close collaboration with primary care physicians is also needed.
- •
Collaboration Between Specialists in Decision Making. The guidelines emphasize the need for collaboration between professionals and the importance of heart teams when decisions are being made. This collaboration already exists in tertiary hospitals, but the guidelines challenge us to transform collaborative work into a systematic and formal approach to the assessment of complex cases. The existence of referral hospitals to which patients from any center can be referred would ensure that the heart team strategy is available to the entire population.
- •
Surgical Treatment of Valvular Heart Disease. The availability of surgical teams specializing in mitral valve repair, as recommended in the guidelines, seems a reasonable approach to optimizing outcomes in mitral surgery and provides a reference point for future research. The surgical outcomes presented in the document set the goal to aim for, although achieving it will not be easy in Spain, especially in patients with severe disease. This is illustrated by surgical series published in Revista Española de Cardiología in recent years, in which the mortality and EuroSCORE were virtually on a par.13,14
- •
Implementation of Novel Therapeutic Procedures. Surprisingly, these guidelines do not explicitly mention the cost-effectiveness of new treatments (TAVI would be the paradigm), despite the fact that they represent a significant spending increase in a subgroup of patients with advanced disease. The Spanish cardiology community cannot ignore its responsibility in the current economic climate and should establish rigorous mechanisms to ensure that new technologies are implemented only in situations in which they are truly efficient. This requires a dual educational effort, on the one hand among professionals (who are already under pressure from industry and peer competition) but also among the general population, who need to understand that new technologies should only be used in situations in which their benefit has truly been demonstrated.
These European guidelines contain updated recommendations for the management of patients with valvular heart disease which are extremely useful for the practice of general clinical cardiology. In clinical terms, the recommendation to adopt an integrative approach via a multidisciplinary team of cardiologists, cardiac surgeons, and other specialists is the main novelty. Early indications for surgery, the documentation of excellent outcomes, and the emergence of percutaneous methods are the most notable advances as regards treatment. It is now up to all of the professionals involved to disseminate and implement the new guidelines, a move which will surely impact positively on the quality of medical care in valvular heart disease.
Conflicts of InterestGonzalo Barón: consulting, presentations, and manuscript preparation (Bayer, Boehringer, BMS, Rovi, Sanofi). Ángel Luis Fernández González: attendance at meetings (Edwards LifeSciences). Antonio Fernández-Ortiz: consulting, presentations (Eli Lilly, Daiichi- Sankyo, Bayer, Ferrer, Merck, AstraZeneca, Roche, Chiesi, GSK, Abbott), educational presentations (Merck, GSK), attendance at meetings (Eli Lilly, Daiichi-Sankyo, AstraZeneca, Bayer). Marta Sitges: presentations (Edwards LifeSciences). José Luis Zamorano: consulting, presentations (Boehringer, Daiichi-Sankyo, Astra, Bayer, Philips), royalties (testbooks: Springer and McGraw-Hill). All members of the Committee: manuscript preparation (Sociedad Española de Cardiología).