In the present article, we discuss the recently published guidelines for the treatment of dyslipidemia developed by the European Society of Cardiology (ESC) in conjunction with the European Atherosclerosis Society and with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation.1 To comment on these guidelines, the Guidelines Committee formed a task force composed of members of the Spanish Society of Cardiology (SEC).
Thus, following the same order as the guidelines, the current article reviews the most important aspects of the various sections.
PREVENTIONThe most noteworthy part of this section is that, for the first time, the guidelines stress the importance of population-level interventions: the fewer population-based approaches applied, the more individual interventions required, and vice versa. In addition, population-level lifestyle changes are more cost-effective than drug therapies. These aspects are examined in detail in the guidelines for cardiovascular prevention, the subject of a recent analysis and commentary.2
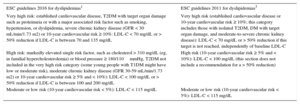
CARDIOVASCULAR RISKThe SCORE risk function has been kept the same for similar groups. The changes made from the 2011 guidelines3 are in line with those proposed by previous guidelines. The latest guidelines contain the following changes (Table 1):
- •
Patients with chronic kidney disease. The very high-risk category only includes patients with severe chronic kidney disease (CKD), namely, a glomerular filtration rate < 30mL/min; those with moderate CKD are placed in the high-risk category.
- •
Diabetic patients without target organ damage and another associated risk factor have been moved from the very high-risk category to the high-risk category. This high-risk category includes individuals with certain markedly elevated vascular risk factors (particularly blood pressure ≥ 180/110mmHg or cholesterol > 310mg/dL).
Treatment Targets in Dyslipidemia: LDL-C. What Has Changed From Previous Guidelines?
| ESC guidelines 2016 for dyslipidemias1 | ESC guidelines 2011 for dyslipidemias3 |
|---|---|
| Very high risk: established cardiovascular disease, T2DM with target organ damage such as proteinuria or with a major associated risk factor such as smoking, hypertension, or dyslipidemia, severe chronic kidney disease (GFR < 30 mL/min/1.73 m2) or 10-year cardiovascular risk ≥ 10%: LDL-C < 70 mg/dL or > 50% reduction if LDL-C is between 70 and 135 mg/dL | Very high risk (established cardiovascular disease or 10-year cardiovascular risk ≥ 10%; this category includes those with isolated T2DM, DM with target organ damage, and moderate-to-severe chronic kidney disease): LDL-C < 70 mg/dL or > 50% reduction if this target is not reached, independently of baseline LDL-C |
| High risk: markedly elevated single risk factor, such as cholesterol > 310 mg/dL (eg, in familial hypercholesterolemia) or blood pressure ≥ 180/110mmHg, T2DM not included in the very high risk category (some young people with T1DM might have low or moderate risk), moderate chronic kidney disease (GFR 30-59 mL/min/1.73 m2) or 10-year cardiovascular risk ≥ 5% and < 10%): LDL-C < 100 mg/dL or > 50% reduction if LDL-C is between 100 and 200 mg/dL | High risk (10-year cardiovascular risk ≥ 5% and < 10%): LDL-C < 100 mg/dL (this section does not include a recommendation for a > 50% reduction) |
| Moderate or low risk (10-year cardiovascular risk < 5%): LDL-C < 115 mg/dL | Moderate or low risk (10-year cardiovascular risk < 5%): LDL-C < 115 mg/dL |
DM, diabetes mellitus; ESC, European Society of Cardiology; GFR, glomerular filtration rate; LDL-C, low-density lipoprotein-cholesterol.
Other notable innovations include a better definition of patients with previous cardiovascular events or documented cardiovascular disease. The guidelines also address the problem of age in the underestimation of the risk of young patients and in the need to recalculate the risk of patients who fall into the “moderate risk” category when they have other risk factors, mentioned in the guidelines, that can increase the risk. However, because the guidelines fail to clearly identify the specific factors prompting a significant risk reclassification, the risk categories should be used to reclassify moderate-risk patients.
LIPID PARAMETERSThis section is practically unchanged from that of the previous guidelines.3 Recent studies of high-density lipoprotein-cholesterol (HDL-C) caution that it is a complex molecule with distinct subfractions and that the presence of dysfunctional HDL-C has a greater effect on atherosclerosis development than HDL-C levels themselves. Triglycerides (TGs) are also recognized as an independent risk factor but they are omitted from the therapeutic target recommendations. Another innovation of the guidelines is the clarification that fasting sampling is no longer recommended for lipid profile analysis.
TREATMENT TARGETSThis was one of the most eagerly awaited sections due to the highly intense debate surrounding the publication of the American guidelines at the end of 2013.4 The truth is that any establishment of a specific target level of low-density lipoprotein-cholesterol (LDL-C) would be arbitrary because the risk is continuous and expressed by a regression line. The authors of the new European guidelines take the time to justify this target, which continues to be 70mg/dL (for very high-risk individuals, including those in secondary prevention), although they accept that it is generally better to reduce the LDL-C as much as possible. Specifically, establishment of a particular target value helps physician-patient communication, adherence, and treatment individualization and personalization. There is another factor: if there is no goal, monitoring is not required, which demotivates both patients and physicians. The SEC had already backed5 the guideline of the ESC, which is unchanged. Importantly, the North American guidelines6 have recently been updated to once again discuss LDL-C targets.
LIFESTYLE MODIFICATIONS TO IMPROVE THE LIPID PROFILELifestyle habits, and especially dietary factors, are playing more and more important roles not only in improving the lipid profile, but also in preventing or improving other cardiovascular risk factors, such as blood pressure and blood glucose. In addition, the available evidence shows that specific dietary patterns can help to prevent cardiovascular disease. The Mediterranean diet, already held in high regard, received a further boost from the results of the PREDIMED study7 of the primary prevention of cardiovascular disease in patients at high cardiovascular risk, the most significant Spanish scientific contribution to these guidelines. A Mediterranean diet supplemented with products such as extra-virgin olive oil or nuts (walnuts, almonds, hazelnuts) should be encouraged via cultural, commercial, and health care policies. Although the general recommendation is to consume fish twice a week, particularly oily fish, the failures of the latest randomized studies with omega-3 discourage supplementation with these products.
The recommendations are to substitute polyunsaturated and monounsaturated fatty acids for some of the saturated fat but it is better to replace saturated fat with monounsaturated fat, particularly that derived from virgin olive oil. Monounsaturated fatty acids also improve insulin sensitivity, decrease TG levels, and, in contrast to polyunsaturated fat, do not decrease, and can even increase, HDL-C. Based on the available scientific data, the most important factor that should be stressed is not the amount of fat consumed, as long as it is less than 35% of total calories as recommended in the guidelines, but the quality.
For the dietary prevention of cardiovascular disease, effort should be made to decrease the intake of trans fatty acids. Their main source is partially hydrogenated polyunsaturated fatty acids of industrial origin. These fats negatively affect the lipid profile, can contribute to the onset of diabetes mellitus, and increase cardiovascular risk.
Because alcohol consumption increases TG levels, its intake should be discouraged in individuals with any type of hypertriglyceridemia, no matter how mild. The guidelines also stress that a moderate reduction in weight in overweight individuals combined with regular physical activity is a very effective method to prevent type 2 diabetes and improve metabolic abnormalities, including the lipid profile and insulin resistance.
More and more space is dedicated in the guidelines to dietary supplements and functional foods, an important consideration given their exponential growth in the market, the growing interest of people in their consumption, and the advertising pressure. The guidelines clarify that there is evidence that certain products can reduce cholesterol levels, especially phytosterols (2g/d reduces LDL-C by 7%-10%) and some traditional Asian products such as red yeast rice (which has a similar action to statins). However, the evidence, except for lipid reduction, is scarce regarding their ability to reduce cardiovascular events and there are few longitudinal safety studies. Because all signs indicate that their consumption will continue to increase, rigorous trials are vital.
DRUGS FOR THE TREATMENT OF HYPERCHOLESTEROLEMIAFor the pharmacological treatment of dyslipidemias, statins continue to be the cornerstone of lipid-lowering therapy. Their effectiveness has been shown once again in the latest trial (HOPE 3, NCT00468923). This study showed reduced morbidity and mortality with high-potency statin therapy (rosuvastatin 10mg) in patients at intermediate cardiovascular risk.
Various meta-analyses indicate that the clinical benefit of statins is largely independent of the type of statin but is closely related to the LDL-C reduction achieved. Thus, the type of statin used should reflect the LDL-C target of each patient. The guidelines reproduce the diagram published in previous guidelines showing the different percentage reductions in LDL-C levels that can be achieved with the different statins.
In addition to recapping the mechanism of action, the guidelines also review the main adverse effects of these drugs, such as muscular or hepatic problems. The current guidelines confirm that statins might increase the incidence of diabetes, as already noted in the previous guidelines.3 The risk is greater for older patients and those with other diabetes risk factors. However, not all statins are equal and more potent statins at higher doses are associated with a greater risk of diabetes development. Notably, the Spanish Agency for Medicine and Health Products states in the data sheet for pitavastatin that it does not increase the incidence of diabetes.
An adverse effect that had not previously been documented is that of possible renal complications, although the authors recognize that this matter is still under debate. An increased frequency of proteinuria has been reported with all statins, although this association has been analyzed in greatest detail for rosuvastatin. A recent Cochrane analysis of renal function failed to identify any beneficial effects of statins on creatinine clearance, but no harmful effects were seen either. The final paragraph of this section is dedicated to reviewing the possible interactions with certain statins, mainly interactions related to hepatic metabolism via cytochrome P450 pathways. As in previous guidelines, the section on statins concludes with combinations of statins and fibrates, combinations that can increase the risk of myopathy. Because the risk is higher with gemfibrozil, this combination should be avoided, and it seems lower with fenofibrate, bezafibrate, and ciprofibrate.
There are no changes from previous guidelines regarding bile acid sequestrants. No morbidity and mortality benefits have been seen with these agents, and their main limitation is poor tolerance due to a high frequency of gastrointestinal adverse effects. Because there are no modifications from previous years, the section dedicated to these drugs in these guidelines is identical to that of previous guidelines.
The guidelines summarize the positive findings of the IMPROVE-IT trial.8 This study determined that a > 70mg/dL reduction in LDL-C is beneficial, with no additional adverse effects, even when the active agent is not a statin. The low incidence of coronary heart disease with low levels of LDL-C in individuals with genetic defects in the protein inhibited by ezetimibe (NPC1L1), together with the results of the IMPROVE-IT trial, support combination ezetimibe + statin therapy when these patients fail to achieve LDL-C targets. This is a novel landmark in the 2016 guidelines because it was only cautiously noted in previous guidelines.
PCSK9 inhibitors are presented as a completely novel therapeutic strategy. They were not even mentioned in the future perspective sections of previous guidelines. This new approach involves the subcutaneous administration of a specific monoclonal antibody against the PCSK9 protein, which in turn inactivates the LDL receptor. PCSK9 inhibitors are administered every 14 or 28 days, and the US Food and Drug Association and European Medicines Agency have already approved the marketing of 2 forms: evolocumab and alirocumab. The guidelines note the extraordinary efficacy of the LDL-C reduction, which ranges between 50% and 70% and is independent of whether the drugs are combined with statins or other lipid-lowering agents, and their low incidence of adverse events and suggest that they might reduce triglyceridemia. Potential drug candidates are listed, such as patients with ischemic heart disease and at high cardiovascular risk or with heterozygous familial hypercholesterolemia who fail to achieve therapeutic targets with the maximum tolerated doses of statins or who do not tolerate them at all. Although the findings might be circumstantial, a grouping of various phase III studies clearly shows a reduction in cardiovascular morbidity and mortality, strengthening the idea that marked reductions in LDL-C, beyond 70mg/dL, have an additional cardiovascular benefit. Such a benefit has already indicated by the IMPROVE-IT study,8 although that bonus reduction was achieved with nonstatin drugs.
The results of studies of the morbidity and mortality of these agents will soon be known. These findings will surely obligate rewriting of the ESC/EAS clinical guidelines, assuming the results are as important as expected. However, the previous experiences with lipid-lowering agents compel us to be cautious when making such comments.
On the other hand, the guidelines report the removal of pharmaceutical preparations containing nicotinic acid. Not only did they fail to reduce cardiovascular morbidity and mortality, they also significantly increased adverse events.
The new clinical guidelines review the potential combinations of these drugs: statins with cholesterol absorption inhibitors (ezetimibe) (IIa B recommendation), statins with bile acid sequestrants (resins) (IIb C recommendation), resins with cholesterol absorption inhibitors, and statins with phytosterols; however, no clinical trials have found fewer cardiovascular events with these last 2 combinations. The main innovations are the increased levels of evidence awarded to combination statin + ezetimibe therapy after the results of the IMPROVE-IT trial,8 the IIb C recommendation for combination PCSK9 inhibitors when LDL-C targets are not reached with maximum tolerated doses of statins, with or without ezetimibe combination, which might be increased in the next edition of these guidelines after the imminent publication of the morbidity and mortality studies of these combinations, and the abandonment of the recommendation to add nicotinic acid to combination therapy.
DRUGS FOR THE TREATMENT OF HYPERTRIGLYCERIDEMIAThis edition of the guidelines stresses on the role played by TGs as a cardiovascular risk factor, with a greater association with the nonfasting TG level than the fasting TG level.9 Recent data from genetic studies using a Mendelian randomization design support the relationship of both the nonfasting TG level and residual cholesterol with higher risks of cardiovascular events and all-cause mortality.10 Residual cholesterol, calculated as TG – (HDL-C + LDL-C), is considered one of the main risk factors for atherosclerosis and cardiovascular events11 and an indirect marker of TGs.12
The guidelines include a comprehensive table showing possible causes of hypertriglyceridemia (HTG), as well as its definition and classification: HTG is considered to be mild or moderate when the TG values are between 150 and 880mg/dL and severe when they are > 880mg/dL.13 Severe HTG is associated with a monogenic mutation and an increased risk of pancreatitis.
The fasting TG target of 150mg/dL is maintained and the therapeutic strategy is similar to that of the previous guidelines.3 Prior to any intervention, the guidelines recommend analysis of possible causes of the TG elevation and an evaluation of overall cardiovascular risk. The main objective is to reduce LDL-C due to cardiovascular risk, given that the evidence of the benefits of a TG reduction is scarce compared with LDL-C reduction. Nonetheless, the current recommendation is for a lifestyle intervention in individuals with TGs > 150mg/dL, and drugs should only be used in patients at high cardiovascular risk and with TGs > 200mg/dL (class IIa, level B).14
Statins are the drug of choice, although the recommendation strength has decreased (class IIa, level B); if a reduction below 200mg/dL cannot be achieved, fenofibrate should be added (class IIa, level C). Omega-3 fatty acids and PCSK9 inhibitors can also be considered, although neither approach has a clear indication. The guidelines do not yet consider niacin or bile acid sequestrants within the therapeutic strategy.
High doses of more potent statins (atorvastatin, rosuvastatin, and pitavastatin) should be the therapy of choice. Although clinical trials of fibrates have identified some beneficial effects, particularly in individuals with elevated TGs and low HDL-C levels, there is no clear evidence for a decrease in all-cause death or death from cardiovascular causes.15 There is evidence that omega-3 fatty acids can reduce TG levels but not cardiovascular events or mortality.16 Two trials currently underway—REDUCE-IT (NCT01492361) with 8000 participants and STRENGTH (NCT02104817) with 13 000 participants—are trying to evaluate the efficacy of these fatty acids in reducing cardiovascular events. Omega-3 fatty acids are generally safe, although they can increase bleeding in individuals taking aspirin/clopidogrel, and a recent study found an association between high omega-3 intake and prostate cancer.17 Finally, the risk of myopathy should be monitored and the use of gemfibrozil avoided in patients under treatment with combination statins and fibrates. If TG levels are poorly controlled with statins or fibrates, omega-3 can be added; this combination is safe and well-tolerated.
DRUGS AFFECTING HDL-C LEVELSThere are few therapeutic options for people with low HDL-C levels. Lifestyle modifications can increase HDL-C levels by 10% but most patients require pharmacological interventions to achieve targets. Nonetheless, after disheartening results with torcetrapib, evacetrapib, and dalcetrapib, the guidelines stress that there is no clear evidence that a HDL increase boosts cardiovascular risk prevention. The only study still underway is the REVEAL trial (NCT01252953) of anacetrapib (in phase III), which hopes to show the efficacy and safety of a HDL-C increase.
Finally, researchers continue to search for drugs that effectively increase HDL-C and apolipoprotein A1 (apoA1) levels and reduce atherosclerosis progression. The main focus is on apoA1 mimetic peptides, which might have additional widespread biological activities, including anti-inflammatory and immunomodulatory effects. However, genetic studies indicate that low HDL-C levels do not cause cardiovascular diseases, weakening the expectations of these therapeutic options.
The guidelines lack clear recommendations for the HDL-C values indicating pharmacological therapy initiation, as well as an algorithm specifying values and treatment steps for HTG and low HDL-C, in particular.
MANAGEMENT OF DYSLIPIDEMIAS IN DIFFERENT CLINICAL SETTINGSThe previous guidelines3 had already stressed that the plasma concentrations of lipids are strongly determined by genetic factors. The current guidelines note that the prevalence of such genetic conditions is higher than previously recognized. In their most extreme forms, they manifest as familial dyslipidemias. Due to their frequency and their elevated cardiovascular risk, notable examples include familial combined hyperlipidemia (FCH), with a prevalence of at least 1 in 100, and familial hypercholesterolemia (FH), with a prevalence of 1 in 250 to 300. Both conditions are calculated to be the cause of up to 40% of cases of premature coronary heart disease. FCH is characterized by high levels of LDL-C and/or TGs and is frequently associated with type 2 diabetes, hypertension, and central obesity. Thus, physician understanding of these conditions is vital to permit early diagnosis and treatment.18
Although the previous guidelines3 highlighted the importance of FH, there is still a vacuum in its detection and treatment. The current guidelines present a better definition of the therapeutic targets for LDL-C, use of combined therapy (statins and ezetimibe), and availability of new drugs. Because heterozygous FH is a frequent genetic cause of premature cardiovascular disease that affects half of a given family, physicians need to be fully aware of the importance of its early diagnosis and treatment.
The guidelines detail the clinical criteria for the diagnosis of genetic dyslipidemias: elevated LDL-C levels in subjects and their family members, premature coronary heart disease, and xanthomas. However, it should be stressed that these clinical criteria can only be used to diagnosis the index case (the first individual diagnosed in a family) and should not be applied to other relatives or young subjects in particular. The most effective way to identify new cases is cascade screening of the relatives of the case index.
Atherosclerotic disease in FH is well known but there is little information on its effects on other vascular territories. Recently, a Spanish study of the SAFEHEART registry of FH showed that patients with FH also have increased prevalence of stoke and peripheral arterial disease.19,20
PCSK9 inhibitors, recently approved in Spain, can be an alternative for certain patients with FH. These drugs are very effective and reduce LDL-C levels by an additional 60% in patients under treatment with statins. Because studies of cardiovascular morbidity and mortality are required, the use of these inhibitors should be limited to patients with FH and highly elevated cardiovascular risk, those with LDL-C levels far from the objectives despite maximum lipid-lowering therapy, and those unable to tolerate statins.
Finally, in a notable development, the guidelines explicitly discuss elderly patients and more closely align their treatment with that of the rest of the population. The main differences from previous recommendations are an increased weight of the evidence in favor of statin use in the same way as in younger patients in secondary prevention (I A), a lowered recommendation for lipid-lowering agent titration in elderly people (from I C to IIa C), and an evaluation of the use of statins in primary prevention if patients have classic associated cardiovascular risk factors (from IIb B to IIa B).
MONITORING OF LIPIDS AND ENZYMES IN PATIENTS ON LIPID-LOWERING DRUG THERAPYIn this section, the guidelines precisely detail the recommendations for the systematic analysis of lipids to evaluate patient treatment effectiveness and of enzymes to monitor safety. The main recommendations are shown in Table 2. Notably, the guidelines have modified the cutoff values for creatine kinase elevation contraindicating treatment initiation or suggesting its modification.
Recommendations for the Systematic Analysis of Lipids and Enzymes
| I. Lipid profile |
| 1. How often should the lipid profile be tested? |
| Before initiation of lipid-lowering therapy, at least 2 measurements should be made, with an interval of 1-12 weeks, except when treatment must be started immediately, such as in patients with ACS or at very high risk |
| 2. How often should patients’ lipids be tested after they begin a lipid-lowering therapy? |
| • 8 (± 4) weeks after treatment initiation |
| • 8 (± 4) weeks after treatment modification until therapeutic targets are achieved |
| 3. How often should patients’ lipids be tested once they have achieved a therapeutic target? |
| • Annually, unless there are adherence problems or other specific reasons for more frequent reviews |
| II. Liver and muscle enzymes |
| 1. How often should liver enzymes be tested: ALT in patients under treatment with lipid-lowering drugs? |
| • Before treatment |
| • 8-12 weeks after treatment initiation or after lipid-lowering agent dose increase |
| • If the result of this testing is normal, subsequent routine monitoring of ALT is not recommended |
| 2. If liver enzymes are elevated due to lipid-lowering therapy: |
| If ALT < 3 × ULN: |
| • Continue therapy |
| • Retest liver enzymes in 4-6 weeks |
| If the value is ≥ 3 × ULN: |
| • Stop lipid-lowering therapy or reduce the dose and retest liver enzymes within 4-6 weeks |
| • Cautious reintroduction of therapy when the ALT levels have returned to normal |
| • If ALT remains elevated: rule out other causes of enzyme elevation |
| 3. How often should CK be measured in patients under treatment with lipid-lowering drugs? |
| Before treatment initiation: |
| • If the baseline CK value is 4 × ULN, drug therapy should not be started |
| During the treatment: |
| • Routine monitoring of CK is not necessary |
| • Only if the patient develops myalgia |
| Pay close attention to the onset of myopathy and CK elevations in at-risk patients: elderly patients, patients taking multiple medications or concomitant therapy that could interfere with the effect of the lipid-lowering therapy, patients with liver or renal disease, or athletes |
| 4. If CK is elevated due to lipid-lowering therapy: |
| Re-evaluate indication for statin therapy |
| 4.1. If ≥ 4 × ULN: |
| • If CK < 10 × ULN: |
| Stop treatment for 6 weeks |
| – Check renal function and CK every 2 weeks |
| – Rule out the possibility of transient CK elevation for other reasons such as exertion |
| – Consider the possibility of myopathy if CK remains elevated |
| – Consider combination lipid-lowering therapy: lower-potency statin + ezetimibe or another lipid-lowering drug |
| • If CK < 10 × ULN, without symptoms: |
| – Continue with lipid-lowering therapy |
| – Monitor CK |
| • If CK < 10 × ULN, with symptoms: |
| – Stop statin therapy |
| – Monitor normalization of CK |
| – Reintroduce statins at low doses when CK is normalized |
| • Consider the possibility of transient CK elevation for other reasons such as exertion |
| • Consider the possibility of myopathy if CK remains elevated |
| • Consider combination lipid-lowering therapy: lower-potency statin + ezetimibe or another lipid-lowering drug |
| 4.2. If < 4 × ULN |
| • If there are no muscle symptoms: |
| – Continue statin therapy (ask patient to report symptoms) |
| – Monitor CK |
| • If there are muscle symptoms: |
| – Check symptoms and CK regularly |
| • If the symptoms persist: |
| – Stop statin therapy for 2-4 weeks |
| – Re-evaluate symptoms after 6 weeks |
| – Re-evaluate indication for statin therapy |
| – Reintroduce the same statin or another lower-potency statin |
| – Introduce low-dose statin therapy on alternate days or 1-2 times per week |
ACS, acute coronary syndrome; ALT, alanine aminotransferase; CK, creatine kinase; ULN, upper limit of normal.
In this section, a special emphasis is given to the need for patients to not only make lifestyle changes, but also to maintain these changes over time and to adhere to medication. Thus, the guidelines stress the value of physician-patient communication. Physicians should inform patients of the importance of reaching therapeutic LDL-C targets due to their benefits. Communication skills need to be developed to persuade patients of the importance of their treatment. In addition, patients should be equipped with the tools required to maintain a healthy lifestyle and correct adherence to their treatment. Finally, the guidelines advise the creation of communication systems facilitating treatment adherence.
CONFLICTS OF INTERESTSL. Pérez de Isla, fees for consultancy and advisory work, presentations, preparation of teaching material, and funding to attend scientific conferences from MSD, AstraZeneca, Bayer, MSD, Amgen, Sanofi, Esteve, Ferrer, and Aegerion. E. Galve, fees for consultancy work and presentations from Sanofi, Ferrer, and AstraZeneca and funding to attend scientific conferences from Amgen. A. Castro Conde, fees for consultancy and advisory work, preparation of presentations and teaching material, and funding to attend scientific conferences from Amgen, Sanofi, and MSD. L.A. Álvarez-Sala, fees for presentations from Amgen and MSD.
SEC Working Group for the 2016 ESC Guidelines for the Management of Dyslipidemias 2016, Expert Reviewers for the ESC Guidelines for the Management of Dyslipidemias 2016, and SEC Guidelines Committee.