Patients who have undergone angioplasty with stenting can be reintegrated into normal life at an early stage, thanks to the absence of sequelae associated with the procedure itself. Consequently, these patients can be involved earlier in the second stage of cardiac rehabilitation. Although rehabilitation for coronary patients follows the general guidelines used for all patients, which were developed with the secondary prevention of coronary artery atherosclerosis in mind, the specific form of rehabilitation adopted for each individual with ischemic heart disease will depend on the patient's circumstances, including the revascularization technique used. Regular physical exercise (i.e. physical training), in itself, has substantial cardiovascular benefits for both primary and secondary cardiovascular prevention. In patients who have had a myocardial infarction, training decreases mortality, increases functional capacity and improves ventricular function and remodeling. It is also thought to boost the collateral circulation. In addition, training improves endothelial function and stimulates the circulation of stem cells. It has been shown that physical training after percutaneous revascularization decreases the number of cardiac events. Moreover, in patients with stable angina, it results in fewer events than percutaneous revascularization.
Keywords
Following established practice, the Spanish Society of Cardiology endorses and translates the clinical practice guidelines (CPG) published by the European Society of Cardiology (ESC) and convenes a panel of Spanish specialists with expertise in each topic. This expert panel reviews and summarizes the CPGs from a Spanish perspective, and its reflections are published as an editorial commentary in Revista Española de Cardiología.
The present commentary highlights the main changes and implications for clinical practice in the 2018 ESC/European Society of Hypertension (ESH) guidelines on the management of arterial hypertension (HT).1 This commentary is not intended to provide an exhaustive review, and readers seeking more comprehensive information should consult the original CPG document.
A table near the start of the 2018 ESC/ESH CPG summarizes innovations and changes introduced since the 2013 edition,2 thus providing an overview of the guidelines. This table uses the ESC color code for classes of recommendation and includes sections on “New sections/recommendations” and “New concepts”.
Key Features and New Content
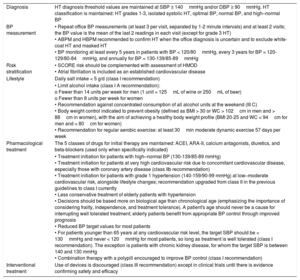
| Diagnosis | HT diagnosis threshold values are maintained at SBP ≥ 140mmHg and/or DBP ≥ 90mmHg. HT classification is maintained: HT grades 1-3, isolated systolic HT, optimal BP, normal BP, and high–normal BP |
| BP measurement | • Repeat office BP measurements (at least 3 per visit, separated by 1-2 minute intervals) and at least 2 visits; the BP value is the mean of the last 2 readings in each visit (except for grade 3 HT) • ABPM and HBPM recommended to confirm HT when the office diagnosis is uncertain and to exclude white-coat HT and masked HT • BP monitoring at least every 5 years in patients with BP < 120/80mmHg, every 3 years for BP = 120-129/80-84mmHg, and annually for BP = 130-139/85-89mmHg |
| Risk stratification | • SCORE risk should be complemented with assessment of HMOD • Atrial fibrillation is included as an established cardiovascular disease |
| Lifestyle | Daily salt intake < 5 g/d (class I recommendation) |
| • Limit alcohol intake (class I A recommendation): o Fewer than 14 units per week for men (1 unit = 125mL of wine or 250mL of beer) o Fewer than 8 units per week for women • Recommendation against concentrated consumption of all alcohol units at the weekend (III C) • Body weight control indicated to prevent obesity (defined as BMI > 30 or WC > 102cm in men and > 88cm in women), with the aim of achieving a healthy body weight profile (BMI 20-25 and WC < 94cm for men and < 80cm for women) • Recommendation for regular aerobic exercise: at least 30min moderate dynamic exercise 57 days per week | |
| Pharmacological treatment | The 5 classes of drugs for initial therapy are maintained: ACEI, ARA-II, calcium antagonists, diuretics, and beta-blockers (used only when specifically indicated) |
| • Treatment initiation for patients with high–normal BP (130-139/85-89 mmHg) • Treatment initiation for patients at very high cardiovascular risk due to concomitant cardiovascular disease, especially those with coronary artery disease (class IIb recommendation) • Treatment initiation for patients with grade 1 hypertension (140-159/90-99 mmHg) at low–moderate cardiovascular risk, alongside lifestyle changes; recommendation upgraded from class II in the previous guidelines to class I currently • Less conservative treatment of elderly patients with hypertension • Decisions should be based more on biological age than chronological age (emphasizing the importance of considering frailty, independence, and treatment tolerance). A patient's age should never be a cause for interrupting well tolerated treatment; elderly patients benefit from appropriate BP control through improved prognosis • Reduced BP target values for most patients • For patients younger than 65 years at any cardiovascular risk level, the target SBP should be < 130mmHg and never < 120mmHg for most patients, so long as treatment is well tolerated (class I recommendation). The exception is patients with chronic kidney disease, for whom the target SBP is between 140 and 130 mmHg • Combination therapy with a polypill encouraged to improve BP control (class I recommendation) | |
| Interventional treatment | Use of devices is discouraged (class III recommendation) except in clinical trials until there is evidence confirming safety and efficacy |
ABPM, ambulatory blood pressure monitoring; ACEI, angiotensin converting enzyme inhibitors; ARA-II, angiotensin II receptor antagonists; BMI, body mass index; BP, blood pressure; DBP, diastolic blood pressure; HBPM; home blood pressure monitoring; HMOD, hypertension-mediated organ damage; HT, hypertension; SBP, systolic blood pressure; WC, waist circumference.
The following paragraphs outline the features regarded by the expert review panelists as the most important changes and new content in the latest guidelines.
2Definition, classification, and epidemiological aspects of hypertensionThe definition of HT remains unchanged from the previous European guidelines: systolic blood pressure (SBP) ≥ 140mmHg and/or diastolic blood pressure (DBP) ≥ 90mmHg. This marks a clear divergence from the latest US guidelines,3 which now define hypertension as blood pressure (BP) readings > 130/80mmHg, a change that has stimulated intense debate over the past year.4 The European guidelines use the same values in younger, middle-aged, and older adults, whereas BP centiles are used in children and adolescents because interventional trial data are unavailable for these 2 groups. There are no changes in the thresholds used to define optimal, normal, and high–normal BP and the different grades of hypertension.
A notable change in this section is the recommendation to assess cardiovascular (CV) risk in patients with no known CV disease using the SCORE scale,5 which provides an estimate of the 10 year risk of a fatal first atherosclerotic event.
The new guidelines also place great emphasis on the need for CV risk estimation to include assessment of what earlier guidelines called target organ damage, and which the 2018 CPG document identifies as hypertension-mediated organ damage (HMOD). HMOD describes alterations to all major organs potentially damaged by HT (heart, brain, retina, kidneys, and blood vessels), some of which are not considered in the SCORE scale. In addition, HMOD is common and frequently goes undetected, and multiple HMODs often occur in the same patient. For these reasons, it is important to exclude the presence of HMOD in patients classified at low risk on the SCORE scale and to identify HMOD in patients with a high or very high SCORE risk. It should also be remembered that an adapted version of the SCORE scale is available for patients older than 65 years; the SCORE OP (older persons) scale is based on patient data from several European countries and has been evaluated in a Spanish population.6,7 Another change is the proposed use of the term “CV risk age” as a useful way to communicate risk and support treatment decision-making. This is illustrated by the example of a younger patient (40 years old) with risk factors but low absolute risk whose CV risk is equivalent to that of a person aged 60 years with optimal risk factors; the younger patient's CV risk age is thus 60 years.
3BLOOD PRESSURE MEASUREMENTAs in previous editions, the guidelines pay close attention to the method used to measure BP, devoting an extensive section to this question. A diagnosis of HT should be confirmed by repeat office BP measurements (at least 2), with at least 3 readings per visit, separated by 1 to 2minutes. On each visit, the recorded BP should be the mean of the last 2 readings (discarding the first). An exception is made for patients with severe HT (grade 3), for whom repeat determinations are not required. The guidelines also encourage the wider use of ambulatory blood pressure monitoring (ABPM) and home blood pressure monitoring (HBPM) to confirm a diagnosis of HT, maintaining the same thresholds as the previous CPG document. The guideline authors note that these out-of-office BP measurements are more reproducible and have a higher prognostic value than office BP measurement; however, some authorities would go further and recommend routine confirmation of an HT diagnosis with ABPM, especially in patients with grade 1 HT values, in line with the NICE guidelines.8 The use of HBPM is encouraged in light of evidence of its positive impact on treatment adherence and BP control; however, this recommendation is accompanied by a warning against inappropriate use, which can lead to clinical problems. Precise instructions are given, similar to those in the Spanish consensus document published a few years ago.9
Following the publication of the SPRINT study,10 the new guidelines incorporate automated (unattended) BP measurement in the physician's office. As the authors remark, unattended BP measurement has been linked to BP values lower than those obtained by conventional office BP measurement. It should be noted, however, that unattended measurement was not used by all participating centers in the SPRINT study, and a recently published analysis shows that the BP readings were independent of the measurement method used.11 Like its predecessor, the new CPG document lacks a list of BP measuring devices validated for use in Europe.
Finally, the guidelines highlight the importance of early detection of HT. Blood pressure monitoring is recommended at least every 5 years for people with values < 120/80mmHg, every 3 years for those with BP values in the range of 120-129/80-84mmHg, and annually for those whose BP values fall in the range of 130-135/85-89mmHg.
4Clinical evaluation and assessment of hypertension-mediated organ damage in patients with hypertensionIn this largely unaltered section, the standout change is the inclusion of atrial fibrillation (AF) as a CV disease that should be assessed during patient clinical evaluations. Although AF is routinely assessed in clinical practice, this is the first time that the ESC guidelines specifically identify AF as a cardiac disorder that should be taken into consideration. HT is the most prevalent risk factor among AF patients, and the evidence links HT directly to the origin and maintenance of this arrhythmia.12 It is therefore a very positive move that the HT guidelines now recommend the inclusion of AF in risk stratification.
As in previous editions, the guidelines recommend that all patients undergo a 12-lead electrocardiogram examination to test for left ventricular hypertrophy voltage criteria (including Cornell criteria) and indicators of other heart conditions. A table is included showing the definitions of echocardiographic definitions of left ventricular hypertrophy and left atrial dilatation; these parameters were mentioned in previous guideline documents but were not described in such detail. Likewise, the 2018 guidelines specify the need to record heart rhythm and diagnose cases of asymptomatic AF.
Finally, it is worth reproducing the recommendations included in this section on the types of patients with hypertension who require referral for more specific, hospital-based care:
- •
Patients with suspected secondary hypertension
- •
Younger patients (<40 years) with grade 2 or more severe hypertension in whom secondary hypertension should be excluded
- •
Patients with treatment-resistant hypertension
- •
Patients in whom detection of HMOD would substantially influence treatment decisions
- •
Patients with sudden onset hypertension in whom BP has previously been normal
- •
Patients with other clinical circumstances that the referring physician feels require more specialist evaluation
The new guidelines comment briefly on the genetic determinants of HT. The evidence points to a strong hereditary component in HT, and between 35% and 50% of patients have a first degree relative also affected by the condition. However, HT has a multifactorial etiology, and accumulated genetic analyses explain only about 3.5% of HT cases. Routine genetic testing is therefore not recommended for HT patients (class III, level C); nevertheless, for specific patients with a suspected rare monogenic cause of secondary HT, genetic testing is recommended in class IIa, evidence level B.
6TREATMENT OF HYPERTENSIONThis section covers all aspects of HT therapy: its medical basis, when to initiate antihypertensive treatment, treatment goals and target BP values, lifestyle changes, drug treatment strategies, and the current role of interventional treatments in the management of HT patients.
There are 2 key aspects. The first and most important is the treatment goal. The target “blood pressure value” has been changed from the more uniform and simplified target in the 2013 guidelines and for most patients is now set at 130/80mmHg or even lower. For patients older than 65 years, the guidelines stipulate a target SBP between 120 and 129mmHg. Moreover, treatment initiation is now recommended for patients between the ages of 65 and 80 years with grade 1 HT, whereas the previous CPG document indicated only that treatment should be “considered” in these patients. Unlike the previous edition, the new CPG document includes a recommendation to consider treating patients with high–normal BP (130–139/85–89mmHg) when this is accompanied by a high CV risk, especially in patients with coronary artery disease. These changes have been introduced to reflect the results of meta-analyses of randomized, controlled clinical trials published in recent years.13
The second key aspect is the rational maintenance of 2 main subsections dealing with treatment strategies: lifestyle changes and BP-lowering drug therapy.
For most patients, the new guidelines tend to recommend the simultaneous introduction of lifestyle changes and pharmacological treatment.
Lifestyle recommendations have been updated in light of recent publications and are now stricter, both for reducing salt and alcohol intake and for targeting waist circumference through weight loss and regular physical activity. The guidelines also bring together important recent advances in pharmacological treatment identified in recent clinical trials and meta-analyses; these studies have addressed the prevention of morbidity and mortality in patients with high–normal BP, the treatment of patients with grade 1 HT and low risk, as well as the treatment of elderly patients with HT and patients with hypertension and diabetes. Although somewhat lacking in scientific consistency, the available data indicate a reduction in the thresholds for initiating treatment with BP-lowering drugs, as well as lower target values for both SBP (130-120mmHg) and DBP (80-70mmHg) for most patients who tolerate treatment. The exceptions to these strict goals are hypertensive patients older than 65 years or those with chronic kidney disease; for these patients, a target SBP of 130-139mmHg is more beneficial than lower values.
The most important change with respect to the previous edition is the new recommendation to use combination therapy as the first-line pharmacological treatment. This strategy seeks to achieve target BP values earlier and to improve control, and is applicable to most patients. Possible exceptions are elderly patients with grade 1 HT and younger patients with grade 1 HT, SBP < 150mmHg, and low risk; for these patients, an SBP < 130mmHg may be achievable with monotherapy. To improve treatment adherence, the guidelines also recommend that drugs for combination therapy be included in a single pill, containing 2 or 3 antihypertensive drugs. This may turn out to be the most difficult recommendation to implement in daily practice, particularly in a country like Spain, where the use of fixed dose drug combinations receives insufficient support from the health care authorities.14 This could be one of the greatest challenges we face over the coming years.
7Hypertension in specific circumstancesThe new guidelines present several clinical scenarios not considered in the previous guidelines, such as ethnicity, the coexistence of HT with valve disease or aortic disease, and HT related to anticancer drug therapy. Other content has been removed, including the specific subsections on metabolic syndrome, obstructive sleep apnea, renovascular disease, and primary hyperaldosteronism.
Recommendations for the pharmacological treatment of resistant hypertension center on the results of the PATHWAY-2 study.15 Invasive strategies such as renal denervation are discouraged because the available evidence raises questions about their clinical role. The guidelines highlight the importance of volume overload as a cause of resistant HT and recommend salt restriction and intensified diuretic therapy as appropriate treatments. Mineralocorticoid receptor antagonists effectively control many cases of resistant HT and are recommended as the fourth-line treatment.
The guidelines cover several specific aspects of HT in daily clinical practice. For white-coat HT, the guidelines recommend assessment of individual CV risk profiles, including a screen for HMOD; white-coat HT patients with a higher CV risk or organ damage should be considered for antihypertensive drug therapy, alongside lifestyle recommendations. Poorly controlled masked HT is very common, and the guidelines underline the need for out-of-office BP measurement; however, masked HT is usually caused by poorly controlled nocturnal BP, and can therefore only be detected with ABPM. Since the publication of these latest ESC/ESH guidelines, the results of the Spanish CARDIORISC registry have been released.16 The CARDIORISC findings confirm that white-coat HT is nonbenign and that masked HT is associated with a higher mortality risk than persistently elevated BP.
This section also makes recommendations for the treatment of HT in specific age groups. Despite the lack of evidence from clinical outcome trials, antihypertensive treatment is recommended in younger adults (< 50 years) with grade 1 HT because of the linear relationship between elevated BP and long-term CV events and death. Isolated systolic HT in young patients is closely associated with smoking, and the guidelines advise against routine assessment of central BP because it is normal in this patient group and the methodology for measuring it is usually unavailable.
For the treatment of HT in older patients (≥ 65 years < 80 years), the new guidelines reject the excessively conservative recommendations of previous guidelines in favor of an approach similar to that used in adult patients younger than 65 years. This change was prompted by recent evidence supporting the treatment of HT in elderly patients, including those who are frail.17 The new CPG document rightly introduces the concept of frailty, which is a more important factor in decision-making than chronological age. Periodic functional and cognitive assessments are recommended, and the value of these evaluations increases with patient age (although this is not clearly expressed in the text). Unlike the previous CPGs, the latest document recommends antihypertensive therapy for grade 1 HT in patients between the ages of 65 and 80 years who tolerate the treatment well; the goal is to achieve an SBP in the range of 130-139mmHg, and the guidelines even advise this treatment for patients older than 80 years who tolerate it well.
The recommendations on HT in pregnancy have been extensively revised. Important changes include the specific recommendation to monitor uric acid in pregnant hypertensive women, the advisability of Doppler ultrasound of the uterine arteries to identify women at risk of complications, and the recommendation to use angiogenic markers to predict pre-eclampsia. Based on the results of a clinical trial published in 2017,18 the guidelines recommend a daily aspirin dose of 100–150mg in weeks 12 to 36 of pregnancy for women with a high or moderate pre-eclampsia risk. A low evidence level is maintained for recommendations on target BP values and the timing of treatment initiation. In contrast with the mild hypertensive effect of estrogens in contraceptive pills, hormone replacement therapy in postmenopausal women does not increase HT. Other noteworthy content in this section includes the link between ethnicity and comorbidities such as diabetes mellitus, chronic kidney disease, chronic obstructive pulmonary disease, and anticancer drugs that can increase BP, such as proteasome or angiogenesis inhibitors. There are no major changes to the recommendations for the treatment of pregnant women with heart disease.
Regarding HT and cerebrovascular disease, the new guidelines reject the previous recommendation for immediate and intense BP reduction in all patients with acute intracerebral hemorrhage and high BP. (This change follows the rejection of routine antihypertensive therapy for acute ischemic stroke in the previous guidelines.) In its place, the new guidelines recommend a more conservative approach, although an exception is made for patients with BP ≥ 220mmHg, who might benefit from BP reduction < 180mmHg. In acute ischemic stroke, BP reduction is only recommended for patients scheduled for thrombolysis, in whom BP should be lowered and maintained at < 180/105mmHg for at least the first 24hours after the procedure. In the period starting several days after ischemic stroke (or immediately after a transient ischemic attack), BP-lowering drug therapy is strongly recommended for hypertensive patients; the goal should be to reduce SBP < 130mmHg, as indicated by the results of the Secondary Prevention of Small Subcortical Strokes Trial.19 The guidelines also contain a new set of recommendations for patients taking anticoagulants. These include reducing BP to < 130/80mmHg and proceeding with extreme caution at BP ≥ 180/100mmHg; both these recommendations have a low level of evidence (the second of them is derived from the exclusion criteria for morbidity and mortality trials with anticoagulant drugs).
The new CPG document devotes a long subdivided section to the management of HT in patients with vascular disease. The guideline authors remark on the knowledge gap regarding the treatment of HT in patients with tight carotid stenosis, especially when bilateral. Physicians are advised to adopt a cautious approach to the speed and degree of BP lowering. A cautious approach is also recommended for the treatment of lower extremity arterial disease in the presence of critical ischemia. For arterial stiffness, indirect evidence suggests that renin-angiotensin system (RAS) blockers may be more potent than antihypertensive drugs; however, there is no evidence to indicate that they are more beneficial. Moreover, centers commonly lack the technology to measure arterial stiffness. Taken together, these considerations justify the exclusion of this parameter from decision-making. The recommendations for BP management in patients with aortic diseases are taken from the recent ESC guidelines on this topic.20 These recommendations include reducing BP to < 130/80mmHg in patients with aortic dilatation or bicuspid aortic valve disease, although the supporting evidence is weak in both settings. The guideline authors challenge the mistaken view that BP-lowering treatment is deleterious in patients with aortic stenosis and hypertension. Similar misconceptions occur in relation to the use of beta-blockers to treat chronic obstructive pulmonary disease or symptomatic peripheral arterial disease, conditions in which this treatment benefits most patients.
The section on sexual dysfunction has been revised and expanded. The guidelines mention the prognostic value of erectile dysfunction and its negative influence on treatment adherence and describe the effects of available treatments. Nonetheless, the information presented is old and rather inconsistent, reflecting the conflicting published data, which do not identify the simple fact of lowered BP as possible major cause of erectile dysfunction.
The final part of this section updates the approach to the perioperative management of HT, presenting recommendations that are sometimes unclear and have a low level of evidence. Recent data suggest that the perioperative use of beta-blockers is linked to an increased risk of complications; nonetheless, the guidelines recommend against either abrupt or programmed gradual discontinuation. Transient preoperative discontinuation of RAS blockers is recommended, as these drugs appear to be associated with an elevated incidence of complications.
8Managing concomitant cardiovascular disease riskThe recommendations for statin therapy are adjusted to the latest guidelines in this area.21 For patients with a very high CV risk, the goal of statin therapy should be to achieve a low-density lipoprotein cholesterol (LDL-C) level of < 70mg/dL or a reduction of at least 50% from a baseline level between 70 and 135mg/dL. For patients at high risk, the LDL-C goal is < 100mg/dL or a ≥ 50% reduction from a baseline level between 100 and 200mg/dL; for patients at intermediate or low risk, the goal is LDL-C < 115mg/dL. Antiplatelet therapy in patients with HT is indicated only for secondary prevention, and the recommended treatment is low dose aspirin; there is no identified patient subgroup with an indication for primary prevention (previously a contentious issue in the literature).
9PATIENT FOLLOW-UPThe standout feature of the section on patient follow-up is its emphasis on patient assessment and its influence on treatment adherence. A new consideration introduced in these guidelines is the key role of nurses and pharmacists in the long-term treatment of HT. These professionals have an important role to play in patient instruction, support, and follow-up as part of a general strategy to improve BP control and achieve better adherence to treatment.
The section includes a table detailing the main interventions that could be implemented not only by physicians and health care systems, but also by patients and their support network. These interventions include strategies to facilitate adoption of a healthy lifestyle, promote patient empowerment, set up group sessions, and increase treatment accessibility. The guideline authors consider treatment nonadherence to be one of the most common causes of inadequate BP control.
10FINAL SECTIONSLike other ESC guidelines, the current document ends with 3 summary sections: “Gaps in the evidence”, which includes 26 questions (compared with half this number in the previous edition); “Key messages”; and a tabulated section listing “‘What to do’ and ‘what not to do’ messages”, each presented with its corresponding recommendation class and evidence level.
11CONCLUSIONSIn this commentary on the latest ESC/ESH guidelines on HT, we have attempted to highlight the most important content in the new CPG document, which is even more extensive than the 2013 edition. An important point of clinical interest in the new CPG is the maintenance of the previous diagnostic threshold values for HT; publication of these thresholds has been eagerly awaited in view of the debate triggered by the revised values adopted in the USA. Moreover, the European diagnostic thresholds have been maintained at the same time as target BP values for most patients have been reduced; the revised treatment targets are mostly based on the results of meta-analyses, since there have been very few new clinical trials in recent years. It might appear inconsistent to maintain a diagnostic threshold of 140/90mmHg while setting the target for BP control at < 130/80mmHg; however, the evidence indicates that these lower values have a superior prognostic value.
The treatment recommendations strengthen measures to promote lifestyle changes. Moreover, in the absence of new antihypertensive drugs in the therapeutic arsenal, the guidelines recommend combination therapy from the outset; the preferred treatment route is a polypill containing several drugs, with the aim of improving treatment adherence and thus BP control, an area that requires further attention. In addition to other treatment recommendations for specific situations, the guidelines propose follow-up norms and interventions to improve treatment adherence.
12CONFLICTS OF INTERESTNone declared.
SEC Working Group for the 2018 ESC/ESH Guidelines on Arterial Hypertension: Pilar Mazón (coordinator), Francisco Marín (coordinator), Juan Cosín-Sales, Alberto Cordero, Inmaculada Roldán, Xavier García-Moll, Carmen Suárez, and Antonio Coca.
Expert Reviewers for the 2018 ESC/ESH Guidelines on Arterial Hypertension: Carlos Escobar, Vivencio Barrios, Rafael Vidal, Pablo Díez-Villanueva, Clara Bonanad, Alberto Esteban, Pilar Zuazola, Vicente Bertomeu, Manuel Abeytua, and Pilar Zuazola.
SEC Guidelines Committee: Fernando Alfonso, Borja Ibáñez, Fernando Arribas, Gemma Berga Congost, Héctor Bueno, Arturo Evangelista, Ignacio Ferreira-González, Manuel Jiménez Navarro, Francisco Marín, Leopoldo Pérez de Isla, Antonia Sambola, Rafael Vázquez, and Ana Viana-Tejedor.