The previous recommendations on fitness and sports activity in athletes with cardiovascular disease (CVD) of the European Society of Cardiology (ESC) were published in 2005. Aimed at competitive athletes (amateur or professional), their application to recreational sport and particularly to physical exercise in patients with CVD was very limited. Accordingly, these new guidelines,1 more than a simple update of knowledge based on new scientific evidence, represent an essential and long-awaited change in the orientation of the recommendations that can be broadly used by cardiology specialists to evaluate the sports fitness and the prescription and monitoring of physical exercise and sports activity, both competitive and recreational, of patients with CVD (figure 1).
The current guidelines comprise a document with much longer reach and breadth than their predecessor and include novel recommendations for specific patient subgroups (eg, pregnant women, older people, patients with chronic kidney disease, spinal cord injury, or cancer, and those with ventricular assist devices) and the approach to sports activities in extreme environments (eg, heat, pollution, altitude, underwater). Due to length, the document is complemented with supplementary material for the management of specific patient groups. This material, only available in the online version of the original guidelines, should not be ignored by the reader.
Ischemic heart disease is the leading cause of exercise-related sudden cardiac death2,3 in both ischemic patients and athletes older than 35 years. Accordingly, the recommendations for the assessment of the asymptomatic population older than 35 years, as well as the recommendations for sports activity in patients with coronary heart disease, are highly relevant and are available in the form of an interactive algorithm via a smartphone application in the pocket guidelines (Figures 4 and 5 of the original guidelines, respectively).
It should be clarified that the guidelines do not establish diagnostic recommendations for the management of symptomatic athletes (eg, those with chest pain or syncope), but specific recommendations on sports activities after determination of the underlying cause. Accordingly, clinicians must follow the relevant recommendations of the corresponding ESC guidelines.
COMMENTS ON THE METHODOLOGYThese guidelines represent a major advance in the form and content of the previous edition. However, the lack of prospective studies on the effects of intense exercise and competitive sports in the natural history of diseases, as well as the risk of acute cardiovascular complications in patients with previous CVD, lead to major gaps in the scientific evidence in many of the guideline recommendations, which are based on expert consensus. For this reason, the level of scientific evidence of these guidelines is lower than that of other current ESC guidelines on the management of specific diseases.
NOVELTIESIn contrast to the previous document, the current guidelines introduce an initial section describing the differences between activity and physical exercise, the components of physical fitness (morphological, muscular, motor, cardiorespiratory, and metabolic), the methodology for exercise prescription according to the FITT concept (frequency, intensity, time, and type), the types of training, and the classification of sports. These definitions not only provide uniformity to the criteria and recommendations of the document, but also help to standardize the clinical practice. The Mitchell classification of sports,4 based on the dynamic and static components of sports and used in the 2005 guidelines, is replaced by a more useful classification for clinicians. This new system establishes the type of sporting discipline according to the predominant component (skill, power, mixed, and endurance) and exercise intensity (low, medium, and high).
The recommendations on sports activities and exercise in patients with cardiomyopathies include major novelties. A genetic study is now recommended to assess the individual risk of athletes with certain cardiomyopathies. In this context, the existence of pathogenic genetic variants associated with a high risk of cardiovascular events, such as those found in lamin A/C (LMNA) and filamin C (FLNC) in patients with dilated, arrhythmogenic (ACM), or noncompaction cardiomyopathy, indicates that athletes with the same condition require a different management approach and different recommendations, which may be particularly restrictive for competitive and high-intensity sports. In addition, the guidelines establish the ACM genotypes that should undergo more frequent follow-up during the practice of physical exercise (pathogenic genetic variants in desmoplakin [DSP] and TMEM43 and in carriers of multiple pathogenic variants).
One of the most pertinent novelties of these guidelines is the change in the sports activity recommendations in patients with hypertrophic cardiomyopathy (HCM). For the first time, patients with HCM may participate in competitive sports or high-intensity exercise (class IIb C) if they have no risk markers (defined as the absence of previous symptoms, arrhythmias, or an abnormal blood pressure response to exercise, as well as a sudden cardiac death risk score <4%) and no risk of harm or death in the case of syncope. Equally, patients with HCM can participate in competitive sports if they are genotype positive but phenotype negative (IIb C). We note that the previous ESC and AHA/ACC recommendations contraindicated sports activities in all patients with HCM. This change to the recommendations is due to the lack of conclusive evidence of the significant increase in arrhythmic risk during exertion in athletes with low-risk HCM.5
The guidelines recommend 150minutes per week of low-intensity exercise in all people with ACM (IIa C) and allow individuals with low arrhythmic risk (asymptomatic, with minimal structural abnormalities, and fewer than 500 premature ventricular contractions/24h) to participate in low-to-moderate-intensity recreational sports (IIb C). Notably, high-intensity exercise is not recommended in any patient with ACM, even in those with a mutation but without phenotypic expression (genotype positive/phenotype negative).
In noncompaction cardiomyopathy, fitness for sports activities is based on ventricular function: competitive sports and high-intensity exercise are allowed when the left ventricular ejection fraction (LVEF) exceeds 50% in patients without symptoms and other risk markers (IIb C) and both are restricted when the LVEF is less than 40%. Athletes with a LVEF of between 40% and 49% can participate in low-to-moderate-intensity recreational sports programs (IIb C), although the guidelines do not clarify their fitness for competition.
The individualized prescription of physical exercise is considered part of the comprehensive management of dilated cardiomyopathy. Stress echocardiography assumes a major role in the differential diagnosis of physiological vs pathological cardiac remodeling (less than a 10%-15% increase in LVEF at peak exercise is considered abnormal). However, the guidelines are more restrictive regarding the LVEF threshold allowing competitive sports, which is established at 45% (as long as there are no other risk factors); this cutoff was 40% in the previous guidelines.
In the assessment of athletes with myocarditis, the authors stress that patients’ medical records should be searched for the consumption of toxins (eg, cocaine, amphetamines). After recovery from myocarditis, individuals should undergo risk assessment via imaging studies, stress test, and Holter monitoring (I B). The document highlights the value of cardiac magnetic resonance (CMR) for detecting edema and myocardial fibrosis. The resumption of any sports activity, including competitive sports, can be considered after 3 to 6 months in asymptomatic athletes with normal biological markers and complementary tests (IIa C).
In the section on arrhythmias, there are major and novel recommendations that rely on shared decision-making with the athlete in question. The main recommendations include:
- •
In individuals with an implantable cardioverter-defibrillator (ICD), according to the observations of the ICD Sports Safety Registry6—low risk of events and of poor ICD functioning/device damage during sports activities—, fitness for competitive sports activities should be evaluated based on the underlying disease, the psychological impact of possible discharges, the risk of harm associated with syncope, and the risk of trauma in the device site (IIa C).
- •
Competitive or high-intensity sports are limited to asymptomatic athletes with long QT syndrome, even those treated with beta-blockers, when the QTc is> 500ms or when there is a positive genetic study and a QTc> 470ms in men and> 480ms in women (III B). Sports activities are permitted in genotype-positive individuals who are asymptomatic and do not meet the specific circumstances for the type and setting of each sport and the extent of precautionary measures (IIa C).
- •
In asymptomatic individuals with Brugada syndrome or phenotypically negative pathogenic mutation carriers, endurance sporting activity is restricted when the core temperature might exceed 39°C (III C), although other types of sporting activity can be considered if the person is asymptomatic (class IIb).
- •
In athletes with atrial fibrillation (AF), pulmonary vein isolation has a class I B indication and represents an alternative first-line treatment in patients with recurrent symptomatic AF or in people who prefer an alternative to drugs. In addition, the guidelines stress the contraindication to class I antiarrhythmic drugs as monotherapy due to the risk of AF or flutter with a fast ventricular response during exercise.
The guidelines highlight the recommendation for safe and necessary physical activity in people with CVD (moderate-intensity aerobic exercise for at least 150min/wk or at least 75min/wk vigorous aerobic activity over at least 4 or 5 days) and the need for an appropriate diagnosis and risk stratification before clinicians agree upon the individualized sports activity recommendations with patients and perform the subsequent corresponding clinical follow-up.
The guidelines consolidate the value of cardiac rehabilitation programs including physical exercise programs in ischemia patients and those with heart failure or ventricular assist devices with a class I A recommendation, as well as in patients who have undergone heart transplant (I B).
Regarding ischemic heart disease, the document endorses the competitive sports participation of individuals with chronic coronary syndrome with a low risk of events during exertion, except for activities with very high cardiovascular demand and older people (IIa C). This recommendation follows on from the ESC position paper7 of 2019 and the AHA/ACC guidelines.8 A difference from those guidelines is the establishment of similar recommendations for the sports activities of patients treated with dual antiplatelet therapy and those treated with anticoagulation: contact sports are not recommended in either case.
Explicit recommendations are made for patients with nonatherosclerotic coronary artery disease—with angina and normal coronary arteries, myocardial bridges, and coronary artery dissection—, although specific recommendations are omitted in cases of vasospastic angina.
The anatomical criteria for the risk stratification of patients with anomalous origin of a coronary artery have been simplified compared with the AHA/ACC guidelines,9 and the general high-risk anatomical criteria are considered without detailing specific indications according to the origin of the anomalous vessel (right coronary of the left sinus or vice versa or origin in the pulmonary artery), as well as the inducibility of ischemia and symptoms. They thus better match the surgical indications in the American and European guidelines on congenital heart disease in adults.
Cutoffs are established that help to differentiate physiological and pathological cardiac remodeling in athletes with valvular disease.10 The current evidence from athletes with bicuspid aortic valves indicates that there is no relationship between sports activities and elevated risk of aortic dilatation/events.11 Therefore, sports participation is not contraindicated unless patients exceed the diameter cutoff of 40mm or have other risk criteria. The most important recommendations in patients with mitral valve prolapse are aimed at identifying athletes at high risk of sudden cardiac death.
All people with congenital heart disease are recommended to perform regular and moderate-intensity exercise (I B). Exercise prescription should be individualized according to the following 5 parameters (I C): ventricular function (echocardiography/CMR), pulmonary artery pressure, aortic dimensions (contact sports should be avoided by those with an aortic diameter> 5cm), presence of arrhythmias, and O2 saturation/lung function.
The authors stress the importance of physical exercise throughout the entire pregnancy and the value of multidisciplinary teams in the management of pregnant cardiac patients. The specific recommendations for sports activity and physical exercise during pregnancy are useful. In general, resistance and water exercises, yoga, stretching, and specific pelvic floor exercises are recommended. The guidelines give little importance to strength training, although it is beneficial in this population with proper supervision. In the case of aortic disease, the authors stress the importance of an imaging study before pregnancy planning (computed tomography or CMR) and also an additional evaluation of the aortic root (CMR without gadolinium).
The recommendations on sports activities in special environments, particularly high-altitude sports and diving, are positive but insufficient to provide individualized recommendations. Due to the complex pathophysiological implications in patients with CVD, the recommendations should be made through a multidisciplinary approach involving specialists from each field.
CONFLICTING ASPECTSIn general, greater detail would be valuable in the recommendations on the individualized prescription of strength training: specific training parameters and individualized progression criteria are lacking and it is difficult to determine the individualized relative intensity values because the repetition maximum (1 RM) test proposed for this purpose is hardly feasible in practice.
The guideline definition of exercise intensity has numerous limitations. This is particularly evident in table 4 of the guidelines, which presents the values of the intensities with respect to the maximum oxygen consumption (VO2max) in a highly debatable way and includes the heart rate values vs the maximum predicted heart rate (HRmax), with the associated limitations (although its limited value is clarified in the text). A conflicting aspect is the use of METs (unit of measurement of the metabolic rate; it corresponds to 3.5mL O2/kg × min, which is the minimum oxygen consumption that the body needs to maintain its vital signs) as an absolute value for the prescription of exercise intensity, given the limitations in its application to populations with reduced physical function or specific conditions. The intensity prescription of physical exercise is always complex and these guidelines leave the most convenient methodology in each case to the arbitrary choice of specialists (table 1).
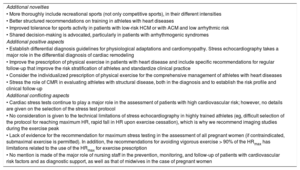
Additional novelties, positive aspects, and conflicting aspects of the guidelines
| Additional novelties |
| • More thoroughly include recreational sports (not only competitive sports), in their different intensities |
| • Better structured recommendations on training in athletes with heart diseases |
| • Improved tolerance for sports activity in patients with low-risk HCM or with ACM and low arrhythmic risk |
| • Shared decision-making is advocated, particularly in patients with arrhythmogenic syndromes |
| Additional positive aspects |
| • Establish differential diagnosis guidelines for physiological adaptations and cardiomyopathy. Stress echocardiography takes a major role in the differential diagnosis of cardiac remodeling |
| • Improve the prescription of physical exercise in patients with heart disease and include specific recommendations for regular follow-up that improve the risk stratification of athletes and standardize clinical practice |
| • Consider the individualized prescription of physical exercise for the comprehensive management of athletes with heart diseases |
| • Stress the role of CMR in evaluating athletes with structural disease, both in the diagnosis and to establish the risk profile and clinical follow-up |
| Additional conflicting aspects |
| • Cardiac stress tests continue to play a major role in the assessment of patients with high cardiovascular risk; however, no details are given on the selection of the stress test protocol |
| • No consideration is given to the technical limitations of stress echocardiography in highly trained athletes (eg, difficult selection of the protocol for reaching maximum HR, rapid fall in HR upon exercise cessation), which is why we recommend imaging studies during the exercise peak |
| • Lack of evidence for the recommendation for maximum stress testing in the assessment of all pregnant women (if contraindicated, submaximal exercise is permitted). In addition, the recommendations for avoiding vigorous exercise > 90% of the HRmax has limitations related to the use of the HRmax for exercise prescription |
| • No mention is made of the major role of nursing staff in the prevention, monitoring, and follow-up of patients with cardiovascular risk factors and as diagnostic support, as well as that of midwives in the case of pregnant women |
ACM, arrhythmogenic cardiomyopathy; CMR, cardiac magnetic resonance; HCM, hypertrophic cardiomyopathy; HR, heart rate; HRmax, maximum predicted heart rate.
The sports classification used, despite being derived from previously published guidelines,12 fails to specify which types of sports are considered contact sports posing a risk of harm to participants or third parties in the event of syncope, as included in the previous classification. These considerations are left to specialists’ discretion.
The controversy regarding the best way to assess master athletes and those who, despite having high or very high cardiovascular risk, wish to participate in high-intensity sports remains unresolved in the current document. Stress testing with or without measurement of oxygen consumption to evaluate inducible myocardial ischemia during exercise remains the current recommendation, despite its low sensitivity and specificity. There is no consensus on the use of imaging techniques for the general assessment of myocardial perfusion. Studies in master athletes show a high prevalence of stable calcified plaques in this population13–15; although this does not preclude the use of calcium scoring and coronary computed tomography angiography for the anatomical evaluation of coronary heart disease in this population group, it may raise doubts about the management of these patients, even though these plaques generally have better prognosis.
Some recommendations lack scientific evidence, such as waiting 3 to 6 months after scheduled coronary revascularization to return to competitive sport, performing an annual stress test in patients at high risk of coronary events and subclinical atherosclerosis, and using coronary angiography for risk stratification after a positive cardiac stress test, a recommendation conflicting with that of the chronic coronary syndromes guidelines16 for ischemia without high-risk criteria (III C). In addition, because master endurance athletes have qualitatively different and presumably more benign coronary artery disease—a higher rate of coronary calcification but a lower rate of unstable soft plaques—that is not associated with a higher rate of events, the value of the application of guidelines on cardiovascular prevention to this population is debatable.
In the evaluation of athletes with hypertension, echocardiography is only recommended to assess target organ damage in athletes who wish to practice high-intensity sports regardless of the degree of hypertension, ignoring the role of this technique in the study of advanced hypertension (with associated aortic disease). This may imply modifications in sports activity recommendations.
Regarding aortic disease, a didactic and accessible classification is made for risk stratification according to aortic diameter, underlying condition, and additional risk criteria. In contrast to the AHA/ACC guidelines,17 which establish sports activity recommendations based on the absolute diameters of the aorta or indexed values or Z-scores, the current recommendations are based on the absolute diameter of the aorta. Although this is the parameter with the most scientific evidence, it is more difficult to apply to adolescent athletes or those with an extreme body surface area. The published reference values of aortic diameters in athletes should be considered.18 In addition, the implications are unknown of the possibility of sports activity resumption after aortic surgery. There is insufficient evidence regarding the natural history of native aortic segments and the additional postoperative risk related to sports activity. The importance should be mentioned of postoperative rehabilitation in these patients.
Despite the updated concept of ACM (including cardiomyopathies characterized by fat replacement or fibrosis of both the right and left ventricles and ventricular arrhythmias), the lack of evidence on the influence of sports activity means that the recommendations are supported by data from registries of patients with arrhythmogenic right ventricular cardiomyopathy and related genetic variants (in whom high-intensity physical exercise is associated with greater disease progression and worse prognosis: increased risk of ventricular arrhythmias and major events, both in patients and in silent carriers). Therefore, competitive or high-intensity sport is restricted for patients and carriers of silent pathogenic genetic variants. These recommendations may not necessarily be extrapolated to some variants of ACM; however, there are insufficient data to support other recommendations. Furthermore, the recommendation for 150minutes of low-intensity exercise in patients with ACM is arbitrary and may be excessively restrictive in some cases; the authors are probably attempting to reconcile the lack of scientific evidence with the recommendations on physical exercise in the general population.
The reversible or irreversible nature of heart failure is not studied in depth, nor is the potential return to the level of previous activity in individuals with potentially reversible conditions, such as myocardial injury induced by toxins, drugs, blood cancer treatments, or tachycardia-induced cardiomyopathy.19
We must highlight some controversies associated with the recommendations on sports activity in athletes with arrhythmias, such as the lack of mention of the physical exercise recommendations in patients with polymorphic ventricular tachycardia (available in the recent ESC guidelines20), the debate surrounding sports activity in patients with long QT syndrome, and the indication for cavotricuspid isthmus ablation in athletes with AF who wish to remain on monotherapy with class I C drugs to prevent flutter onset (class IIa C). In the case of the latter situation, the guidelines fail to specify that this strategy should be limited to patients with a history of typical flutter—and is not useful in cases of atypical flutter—or to remember that pulmonary vein isolation has been shown to be effective for treating patients with the coexistence of both arrhythmias.
IMPLICATIONS FOR CLINICAL PRACTICE IN SPAIN AND LEGAL ASPECTSIn Spain, as in Europe, the demand for cardiological sports medicine checkups has markedly increased, which has led to the need for the creation of sports cardiology clinics. Compared with these clinics, the sports medicine training and experience of many cardiologists are lacking, which is why these guidelines may be hugely useful in decision-making concerning fitness for sports activity and exercise prescription in patients with CVD.
One of the limitations of these guidelines is that they place too much emphasis on the sports cardiology assessments of experts, an unlikely aspect in Spain because few centers are able to provide the required training. The successful development of this subspecialty requires the creation of sports cardiology units in both the public and private systems.
Some changes required for the implementation of these guidelines are improved health training of athletes and the general population regarding the role of checkups prior to sports activity and knowledge of the warning symptoms requiring consultation. Among others, emergency plans will be required in cases of cardiac arrest in sports facilities and competitions and improved protocols for cardiopulmonary resuscitation in the community.
In addition, the major involvement of athletes in shared decision-making represents an advance and adaptation to contemporary cardiology that challenges the paternalism of previous recommendations concerning individuals’ autonomy and values. However, this has medical-legal and ethical implications due to the lack of scientific evidence and because most of the recommendations are based on expert consensus, which is why they cannot be considered legally binding. These considerations may clash with the medical-legal requirement to sign off on the sports fitness of federated athletes. In Spain, the Sports Law is still in the development phase and the exclusion criteria for competitive sports are not yet defined. Accordingly, physicians, based on their clinical experience of sports cardiology, may award fitness outside the scope of this document.
SOCIOECONOMIC IMPLICATIONSThe risk stratification of patients with CVD prior to sports activity may increase requests for noninvasive diagnostic tests, such as stress tests, coronary computed tomography angiography, nuclear cardiology studies, CMR, genetic studies, and other interventional diagnostic tests only available in tertiary hospitals. In addition to the risk of overloading the publicly-funded health system and increasing health spending, inequalities could be created between athletes who can access private health services and those who cannot, with the consequent delays in obtaining sports fitness or exercise prescription.
The greater flexibility of competitive sports recommendations for previously contraindicated patients (eg, those with HCM) will increase the number of competing or active athletes/patients with CVD. This will necessitate the creation of cardioprotected sports environments and appropriate action plans for cardiac emergencies, with personnel trained in cardiopulmonary resuscitation and the provision of semiautomatic external defibrillators, for example. Consequent requirements will be training plans and increased investment in sports facilities.
Overall, we believe that these recommendations will have a positive impact on the overall well-being of athletes and patients and the multidisciplinary teams managing them.
CONCLUSIONSThe current recommendations should serve as a guide for clinicians in the determination of the appropriate risk assessment and stratification methods and enable these professionals to offer individualized advice on sports activity and the prescription of physical exercise to athletes/patients with CVD, through shared decision-making and respect for patient autonomy.
The guidelines should be applied in multidisciplinary settings including health care professionals of different specialties and training (eg, cardiologists, sports and exercise physicians, clinical geneticists, obstetricians, rehabilitators, nursing staff, midwives, physiotherapists), as well as other professionals in the sports field (eg, graduates in exercise science, coaches, athletic trainers) to minimize risks and achieve the best state of health and fitness during sports and physical activity of participants with CVD.
For all of these reasons, the role of sports cardiology specialists is becoming increasingly necessary, despite still being insufficiently incorporated into public health services. Accordingly, clinical cardiologists must improve their training in applying the recommendations contained in these guidelines while public and private health institutions increase their availability of specialized sports cardiology units.
The publication of these guidelines should also serve to promote research into sports and exercise cardiology to identify the best scientific evidence.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest related to the present work.
SEC Working Group for the 2020 ESC guidelines on sports cardiology and exercise in patients with cardiovascular disease: Araceli Boraita (coordinator), Carmen Adamuz (coordinator), María Alcocer Ayuga, Amelia Carro, Leonel Díaz González, Juan Ramon Heredia, Zigor Madaria, María Dolores Masiá, Miriam Rossi, Miriam Sánchez Testal, and Jordi Trias de Bes.
Expert reviewers for the 2020 ESC guidelines on sports cardiology and exercise in patients with cardiovascular disease: Pedro Azcárate, Roberto Barriales, Begoña Benito, Francisco Calvo-Iglesias, Ángeles Fuertes Moure, Fernando de la Guía, Amparo Martínez, Jesús Martínez Alday, Vanessa Moñivas, Esteban Peiró Molina, Tomás Ripoll Vera, and Alejandro de la Rosa.
SEC Guidelines Committee: Pablo Avanzas, Gemma Berga Congost, Araceli Boraita, Héctor Bueno, David Calvo, Raquel Campuzano, Victoria Delgado, Laura Dos, Ignacio Ferreira-González, Juan José Gómez Doblas, Domingo Pascual Figal, Antonia Sambola Ayala, Ana Viana Tejedor, José Luis Ferreiro (copresident), and Fernando Alfonso (copresident).