The recently published European Society of Cardiology (ESC) hypertension guidelines feature several updates and changes, including a new title. The title now includes a new “diagnostic” entity—elevated blood pressure, defined as a systolic blood pressure [SBP] of 120-139mmHg or a diastolic blood pressure [DBP] of 70-89mmHg. In addition, the term arterial has been removed to shift focus from pulmonary hypertension to systemic hypertension. The updated title—2024 ESC Guidelines for the management of elevated blood pressure and hypertension—is a reminder of the continuous relationship between BP and cardiovascular risk.
One of the main changes in the new guidelines is the recommendation to target an SBP of 120-129mmHg in adults receiving BP-lowering treatment.
Another significant change is that a class I recommendation for a given drug or intervention now requires evidence of improved clinical outcomes, not just BP reduction.
Readers are reminded that hypertension is the most important modifiable risk factor for cardiovascular morbidity and mortality worldwide, and that over time it can lead to organ damage and, ultimately, cardiovascular, cerebrovascular, and kidney disease. Attention is also drawn to hypertension-mediated organ damage (eg, left ventricular hypertrophy and left atrial dilation) and its clinical consequences, such as stroke, cognitive impairment, heart failure, ischemic heart disease, atrial fibrillation, and valvular heart disease.
MeasurementsThe 2024 ESC Guidelines outline conditions for BP measurement in both office and ambulatory settings, establish different diagnostic thresholds (table 1), and, compared with the previous guidelines, describe the measurement process in a more systematic manner. They also stress the importance of out-of-office BP measurements (ambulatory [ABPM] and home [HBPM]) for diagnosis and follow-up purposes. The prominence given to out-of-office measurements is driven by the strong evidence showing that ambulatory monitoring can predict cardiovascular events and confirm white-coat and masked hypertension. Finally, the guidelines emphasize the need to use validated BP devices with confirmed accuracy and refer readers to a universal standard1 for validating these devices that was not yet available when the 2018 guidelines were published.
Comparison of elevated BP and hypertension thresholds
| BP, mmHg | Office BP | Daytime ABPM - HBPM | 24-hour ABPM | Nocturnal ABPM |
|---|---|---|---|---|
| Nonelevated BP | <120/70 | <120/70 | <115/65 | <110/60 |
| Elevated BP | 120/70 to <140/90 | 120/70 to <135/85 | 115/65 to <130/80 | 110/60 to <120/70 |
| Hypertension | ≥140/90 | ≥135/85 | ≥130/80 | ≥120/70 |
ABPM, ambulatory blood pressure monitoring (24hours); BP, blood pressure; HBPM, home blood pressure measurement.
The 2024 ESC Guidelines introduce a new systolic BP treatment target of 120-129mmHg but maintain the threshold for diagnosing hypertension at 140/90mmHg. They also clearly define orthostatic hypotension and interarm BP differences and specify that BP should be measured using an auscultatory not an automated method in pregnant women and patients with atrial fibrillation.
The new guidelines recommend opportunistic screening for elevated BP and hypertension at least every 3 years in adults younger than 40 years and at least once a year in those aged 40 years or older. For individuals with elevated BP who do not meet the threshold for BP-lowering medication, a repeat BP measurement and risk assessment within 1 year is advised.
To diagnose hypertension in patients with an office BP of 140-159/90-99mmHg, the guidelines recommend confirmation with out-of-office measurements, or, if this is not possible, repeated office measurements on separate visits. For BP levels of 160-179/100-109mmHg, diagnosis should be confirmed as soon as possible (within no more than 1 month), preferably with ABPM or HBPM. A hypertensive emergency must be ruled out in patients with BP ≥180/110mmHg.
As noted, a key change in the 2024 ESC Guidelines is the introduction of the elevated BP category (SBP 120-139mmHg or DBP 70-89mmHg). This represents a significant departure from the 2018 guidelines, which focused primarily on hypertension, defined as BP ≥140/90mmHg. This traditional threshold of 140/90mmHg was maintained in the 2023 guidelines published by the European Society of Hypertension (ESH). While the ESH did not include an elevated BP category, it did emphasize the importance of risk assessment in individuals with high to normal BP (130-139mmHg).2 The addition of the elevated BP category in the 2024 ESC guidelines is based on evidence suggesting that lowering BP to within this range benefits patients with cardiovascular disease (atherosclerotic or heart failure), moderate or severe kidney disease, hypertension-mediated vascular or cardiac damage, diabetes, or familial hypercholesterolemia.
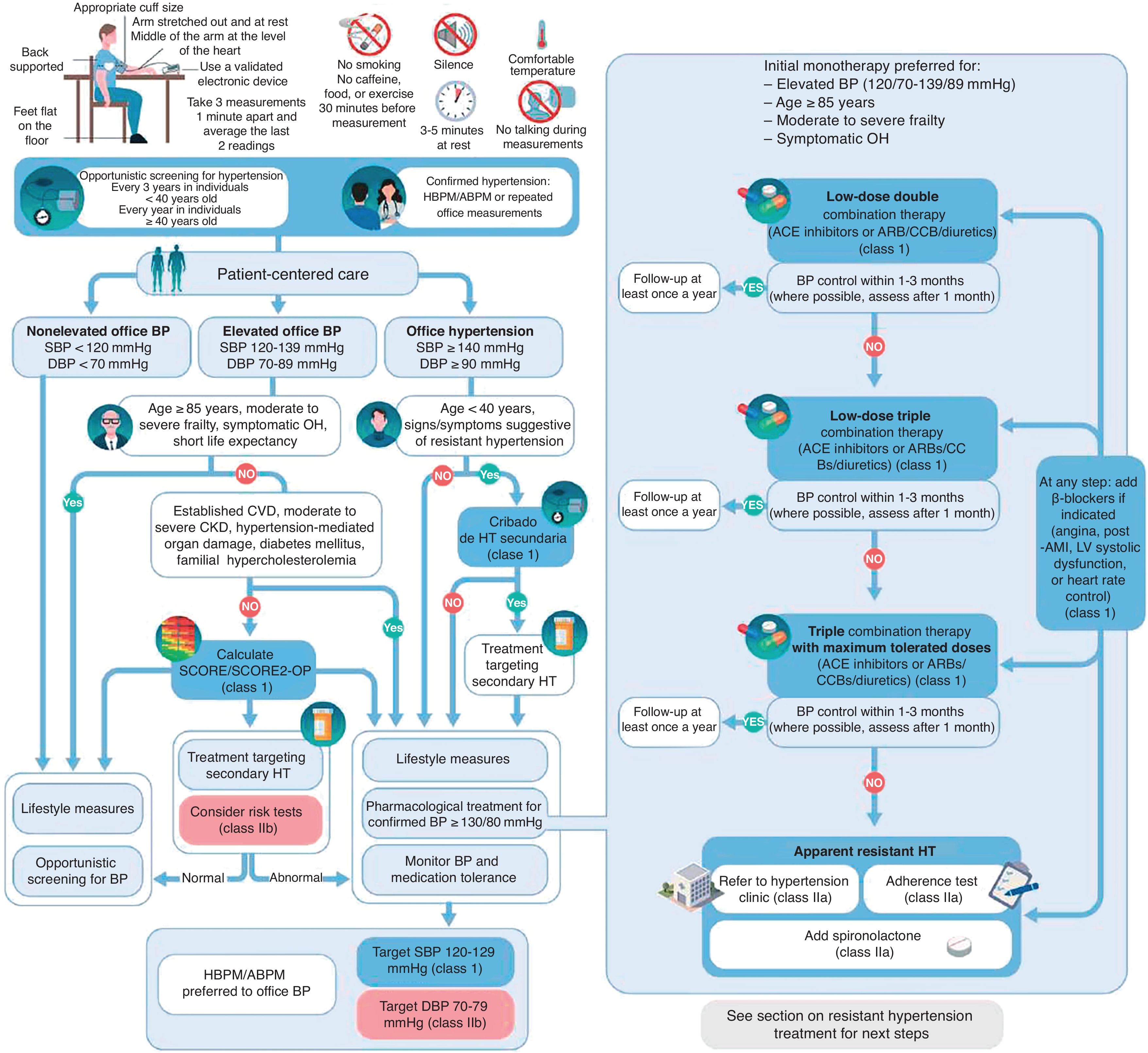
The guidelines discuss the use of predictive models such as Systematic Coronary Risk Evaluation 2 (SCORE2) and SCORE-Older Persons for risk stratification. A 10-year risk of a cardiovascular event of 10% or higher would indicate high risk and support treatment initiation, even in patients with elevated BP. The 2023 ESH guidelines also recommend using prediction models for risk stratification, although they do not explicitly endorse their use in guiding treatment decisions in patients with elevated BP (figure 1).
Central illustration. ABPM, ambulatory blood pressure measurement; ACE, angiotensin-converting enzyme; ARBs, angiotensin receptor blockers; CCBs, calcium channel blockers; DBP, diastolic blood pressure; HBPM, home blood pressure measurement; LV, left ventricular; OH, orthostatic hypertension; SBPM, systolic blood pressure measurement; SCORE2, Systematic Coronary Risk Evaluation 2; SCORE-OP, SCORE-Older Persons.
The components of the initial assessment remain unchanged, and include medical history, medication history, physical examination, an electrocardiogram (ECG), and routine tests, such as basic blood and urine analyses (albumin-creatinine ratio). Additional tests should be based on clinical suspicion. An echocardiogram, for example, is recommended for patients with hypertension and ECG abnormalities or signs or symptoms of heart disease. This test may also be considered for patients with elevated BP, particularly if it is likely to influence clinical decisions. Coronary artery calcium scoring is an option for patients with elevated BP or hypertension when results are likely to lead to treatment changes, as are carotid or femoral ultrasound imaging and pulse wave velocity (table 2).
Risk modifiers that can reclassify cardiovascular disease risk in patients with elevated blood pressure or hypertension
| Sex-specific modifiers (class IIaB) | Modifiers shared by men and women (IIaB) | Additional conditions that increase risk (IIbB) |
|---|---|---|
| Gestational diabetes | High-risk race/ethnicitya | CAC score >100 AU or >P75e |
| Gestational hypertension | Family history of premature-onset cardiosvascular diseaseb | Internal/external carotid plaque or femoral artery plaque |
| Preeclampsia | Autoimmune inflammatory diseasec | Arterial stiffness measured using PWVf |
| Premature delivery | Severe mental illnessd | Elevated NT-proBNP |
| ≥1 stillbirths | Human immunodeficiency virus infection | Elevated high-sensitivity troponin I |
| Recurrent miscarriages | Poverty |
AU, Agatston units; CAC, coronary artery calcium; NT-proBNP: N-terminal pro-B-type natriuretic peptide; P75, 75th percentile.
With a prevalence of 15%-30% in young hypertensive adults, secondary hypertension is now believed to be common than previously thought. The 2024 ESC Guidelines recommend appropriate screening for this condition in individuals with suggestive signs, symptoms, or medical history. Given the prevalence of secondary hypertension, early screening for primary hyperaldosteronism by renin and aldosterone measurements should be considered.
Prevention, treatment, and BP target levelsFor the first time ever, the ESC Guidelines recommend opportunistic screening to improve the prediction of adult hypertension in older children and adolescents with a family history of hypertension.
Lifestyle measures for BP control, and in most cases, cardiovascular risk reduction, continue to be strongly recommended (IA) and include sodium restriction (maximum intake of 2g/d), regular physical activity, weight loss, smoking cessation, and adherence to the DASH (Dietary Approaches to Stop Hypertension) diet. The alcohol consumption limit of 100 g/wk for both men and women also remains unchanged (IB). New recommendations include restricted consumption of sugar-sweetened beverages (sugar intake limited to 10% of energy intake) (IB), potassium supplementation for patients without chronic kidney disease, and monitoring of potassium levels in patients with kidney disease or on potassium-sparing medication (IIaC).
Recommended pharmacological treatments remain largely unchanged. Angiotensin-converting enzyme inhibitors, angiotensin 2 receptor blockers, calcium antagonists, and diuretics continue to be recommended as first-line treatments for BP control and cardiovascular risk reduction. Beta-blockers should be added when patients have angina, heart failure, or myocardial infarction, or need heart rate control.
Combination therapy should be prescribed from the outset, except in patients older than 85 years, frail patients, and those with symptomatic orthostatic hypotension. The addition of spironolactone should be considered when triple combination therapy does not achieve BP control. The guidelines provide a practical algorithm to guide decisions on drug combinations and timing.
Pharmacological treatment should be initiated at BP >140/90mmHg, regardless of risk. Lifestyle changes should be the first step in high-risk patients with BP >130/80mmHg. If control is not achieved within 3 months, BP-lowering medication should be introduced.
The 2024 ESC Guidelines recommend targeting a BP of 120-129/70-79mmHg (IA) provided the medication is well tolerated. This recommendation is based on the latest studies and meta-analyses evaluating hypertension and its impact on cardiovascular risk.
BP devices and consequences of excessive BP loweringGuidance on blood-lowering devices in the 2024 ESC guidelines mainly focuses on catheter-based renal denervation, which is recommended for patients with resistant hypertension (IIbB) and patients with high cardiovascular risk and poor BP control (IIbA). This procedure, however, must be performed only in experienced centers and only in appropriately informed patients following evaluation by a multidisciplinary team. These recommendations mark a significant shift from the 2018 guidelines,3 which recommended renal denervation exclusively for research purposes.
The 2024 ESC guidelines have expanded the definition of preeclampsia to include gestational hypertension accompanied by proteinuria, maternal organ dysfunction (including kidney injury), liver dysfunction, neurological complications, or uteroplacental dysfunction. Proteinuria is no longer mandatory for diagnosis. Low- to moderate-intensity exercise during the first trimester of pregnancy is recommended to reduce the risk of preeclampsia. In addition, the BP threshold for pregnant women has been tightened to 140/90mmHg.
The 2024 ESC Guidelines introduce new groups and recommendations for isolated systolic and diastolic hypertension and orthostatic hypotension with supine hypertension. Clinicians are advised to test for orthostatic hypotension with supine hypertension before initiating or intensifying treatment. Newly diagnosed patients should be encouraged to adopt lifestyle changes and switched to BP-lowering drugs with less impact on orthostatic hypertension.
Management and treatment in special populationsYoung adults (<40 years) and very old adults (≥85 years) have been reclassified in the 2024 ESC guidelines. For older patients aged <85 years without significant frailty or comorbidities, the guidelines recommend using the same treatment targets and strategies as those used in younger patients.
Stricter BP targets have also been introduced for patients with diabetes. The guidelines now recommend starting treatment at BP >130/80mmHg and question the increased risk attributed to BP values <120/70mmHg in the 2018 guidelines.
Renin-angiotensin-aldosterone system (RAAS) inhibitors (IIaC) are recommended for patients with aortic valve stenosis or moderate to severe mitral regurgitation.
The definition and recommended management of resistant hypertension remain largely unchanged, although the new guidelines now advise referral to a specialized center. Treatment continues to require at least 3 BP-lowering drugs, including a diuretic, with the addition of spironolactone (or eplerenone if this is not tolerated) and beta-blockers if not already indicated. This recommendation has been upgraded from IIaB to IB. Catheter-based renal denervation is also mentioned as a treatment option for resistant hypertension. Renal artery angioplasty should be considered for patients with renovascular hypertension (class IIaC recommendation for patients with renal artery stenosis due to fibromuscular dysplasia), but should not be performed if significant stenosis is absent. Finally, the recommendation for using a calcium channel blocker combined with a diuretic or RAAS inhibitor in individuals from sub-Saharan Africa has been downgraded from IB to IIaB.
Acute hypertensionThe 2024 ESC Guidelines contain a new section on managing acute hypertension in specific settings, such as intracerebral hemorrhage, ischemic stroke, hypertensive emergencies, pregnancy, and perioperative periods. BP-lowering treatment before hospital discharge is strongly recommended for patients with ischemic stroke. For those with intracerebral hemorrhage and a starting SBP >220mmHg, the guidelines advise against lowering BP by >70mmHg within the first hour of treatment. To prevent hematoma expansion, the recommended target is an SPB of 140-160mmHg within the first few hours. After a stroke, the target should be 120-129mmHg.
Nursing and patient-centered careThe 2024 ESC Guidelines emphasize patient-centered care and highlight the importance of involving patients in decision-making and their own care. The guidelines stress the need to consider sociodemographic differences and use effective communication strategies to help patients understand the risks of hypertension and the benefits of treatment. Readers are also reminded that a multidisciplinary care approach involving physicians, nurses, pharmacists, dietitians, and physiotherapists can improve BP control in patients with hypertension.
GUIDELINE IMPLEMENTATION: IMPLICATIONS FOR OUR SETTINGThe new threshold for elevated BP in the 2024 ESC Guidelines is accompanied by a reduction in the maximum period recommended for lifestyle interventions—now 3 months. The lower threshold for pharmacologic treatment initiation will result in higher prescription rates but presumably better control. Hypertension diagnoses, however, may be delayed in patients with BP <180/110mmHg who are not classified as high risk, as the new guidelines call for confirmation with out-of-office measurements.4 This poses challenges in areas with widely dispersed populations, where rapid access to primary care and availability of validated home BP devices may be limited.
The need for diagnostic confirmation via ABPM or HBPM may present logistical challenges, as not all patients will have access to ambulatory or home devices. Investment in technology and education for both patients and health care professionals may help address these obstacles. The guidelines recognize the challenges of proper implementation and suggest that scientific societies could play a role in evaluating potential barriers.
The introduction of the elevated BP category and the lower threshold for pharmacological treatment could result in more prescriptions for lower-risk individuals, particularly those with additional risk factors, polypharmacy, or a higher risk of adverse effects such as falls and hypotension. Caution, therefore, must be exercised when prescribing drugs to very old patients (≥85 years) or patients with moderate to severe frailty, orthostatic hypotension, or limited life expectancy. In such cases, the guidelines recommend applying the ALARA principle, that is to pursue an SBP target that is “as low as is reasonably achievable”.
According to the 2024 ESC Guidelines, resistant hypertension is diagnosed when lifestyle measures and treatment with maximally tolerated doses of a diuretic (thiazide or thiazide-like), an RAAS inhibitor, and a calcium channel blocker do not lower ABPM- or HBPM-confirmed office BP values to <140/90mmHg. The need for out-of-office confirmation may lead to diagnostic delays, as not all patients will be able to promptly return with the required readings. The guidelines also recommend referring patients with resistant hypertension to specialized centers, but again, this may not always be feasible.
The use of a target BP control range rather than a fixed value is intended to provide flexibility to both physicians and patients; the guidelines also emphasize the importance of lifestyle changes. While the 2021 ESC guidelines on cardiovascular disease prevention recommended a 2-step strategy,5 the 2024 ESC guidelines show a clear preference for a single target range, provided it is tolerated and feasible. More relaxed BP targets are proposed for patients with frailty or orthostatic hypotension.
The 2024 ESC Guidelines recommend catheter-based renal denervation in 2 cases, but require the procedure to be performed by an “experienced center”. They do not, however, specify what they mean by “experienced”, potentially complicating referrals and decisions to prescribe the procedure in our setting.
The 2024 ESC recommendations on resistant hypertension are consistent with the findings of the TRIUMPH trial, which showed that dietary changes and physical exercise within a cardiac rehabilitation program improved both clinical outcomes and BP control in patients with resistant hypertension.6 Given these findings and recommendations, we may see an increased use of cardiac rehabilitation in Spanish hospitals.
The 2024 ESC Guidelines recommend motivational interviewing7 as a strategy for improving adherence to hypertension treatment. They also highlight the empowering effects of self-care, healthy lifestyle behaviors, and APBM, and mention that adherence can be improved with appropriately timed medication reviews—which help optimize treatment—and the help of family members or other social support providers. We believe that these recommendations highlight the need for specialized nursing units to support patients with hypertension.
GAPSMore epidemiological data and prospective studies are needed to improve our understanding of hypertension, in particular aspects such as sex-specific differences, risk factors, and pathophysiology, all of which can be influenced by biological, hormonal, and sociocultural conditions. Further research is also needed on the role of less traditional risk factors, such as stress, socioeconomic conditions, and barriers to health care access. The 2024 ESC Guidelines acknowledge the existence of female-specific conditions, such as preeclampsia, but provide vague guidance on how these factors could be integrated into risk assessments.
It is accepted that risk stratification and patient selection are complex, often subjective, processes. The guidelines recommend predictive models such as SCORE2, but it is unclear whether these models can be universally applied, particularly in regions that have different population characteristics and risk factor prevalences to Europe.
The 2024 ESC guidelines acknowledge the lack of evidence on the benefits of treating low-risk individuals with elevated BP and highlight the need for more consistent data to support the use of BP-lowering medication in high-risk patients with an SBP of 120-129mmHg.
The 2024 ESC Guidelines do not mention the classic terms controlled resistant hypertension (BP at target requiring ≥4 medications) or refractory hypertension (BP not at target despite ≥5 medications). This could pose challenges, particularly considering that refractory hypertension is one of the indications for catheter-based renal denervation.
The 2024 ESC Guidelines also acknowledge that hypertension is understudied in women, but do not recommend any specific strategies for improving the detection of predisposing conditions in this population.
Although previous guidelines mentioned dipping patterns, potential causes of non-dippers, and paradoxical increases in the risk of extreme dipping, the new guidelines give greater prominence to these aspects of BP in a new section on nocturnal hypertension, which defines the condition and describes potential causes, risk factors, and treatment. Nonetheless, the recommended treatments and guiding values remain largely unchanged.
Finally, the 2024 guidelines, like their predecessors, do not recommend any specific digital tools for self-management. Although the authors acknowledge advances in these tools, they note that evidence on their efficacy is still lacking.
FUNDINGNone.
USE OF ARTIFICIAL INTELLIGENCEArtificial intelligence was not used to generate the content of this article.
CONFLICTS OF INTERESTNone.
Spanish Society of Cardiology (SEC) Guidelines Committee: Pablo Avanzas (President), Pilar Mazón (Secretary), Rut Andrea Ribas, Marisol Bravo Amaro, Alberto Cordero Fort, Marisa Crespo, F. Javier Jiménez Candil, María Antonia Martínez Momblan, Sonia Mirabet Pérez, Juan Sanchis Forés, Marta Sitges Carreño, José M. de la Torre, Javier Torres Llergo, and David Vivas.
SEC Working Group for the 2024 ESC guidelines for the management of elevated blood pressure and hypertension: Vivencio Barrios (coordinator), Marisol Bravo Amaro (coordinator), Vicente Arrarte, Alejandro Berenguel, Carlos Escobar, Lorenzo Fácila, María Rosa Fernández Olmo, and Miriam Rossi López.
Corresponding author. E-mails: vivenciobarrios@gmail.com (V. Barrios); maria.sol.bravo.amaro@sergas.es (M. Bravo Amaro).