The new guidelines of the European Society of Cardiology (ESC) 2023 for the management of patients with cardiovascular (CV) disease (CVD) and diabetes incorporate a central figure that focuses on the presentation of a patient with diabetes and CVD: first case: a patient with CVD that includes atherosclerotic cardiovascular disease (ASCVD), atrial fibrillation (AF) and heart failure (HF), in whom diabetes screening must be performed; second case, a patient with diabetes in whom CVD or chronic kidney disease (CKD) must be ruled out.
In the first case, there are no changes for the diagnosis of diabetes using the already known diagnostic criteria1: a) fasting plasma glucose ≥ 126mg/dL; b) glycated hemoglobin (HbA1c) ≥ 6.5%; c) plasma glucose 2hours after an oral glucose overload test (75g) ≥ 200mg/dL; and d) plasma glucose ≥ 200mg/dL in patients with classic symptoms of hyperglycemia or a hyperglycemic crisis.
In the second case, CVD screening is recommended based on the patient's symptoms and electrocardiogram (ECG). The document does not introduce peptides in this screening, or imaging tests, or detection of ischemia in asymptomatic patients with diabetes.
Once the diagnosis of type 2 diabetes mellitus (T2DM) is established, for patients without ASCVD or severe target-organ damage (TOD), a novel T2DM-specific risk score (SCORE2-Diabetes) is introduced. CV risk categories in T2DM are now defined based on the presence of ASCVD or severe TOD or the 10-year CVD risk using SCORE2-Diabetes. This tool integrates information on conventional CVD risk factors with diabetes-specific information.2 Unfortunately, the tool does not include natriuretic peptides in the risk estimation.
More than 90% of patients with T2DM have high or very high CV risk and the application of SCORE2-Diabetes to estimate 10-year CVD risk in patients without symptomatic ASCVD or severe TOD may limit patient access to recommended sodium-glucose co-transporter-2 inhibitors (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP-1 RA) with a significant prognostic impact.
Another weak point to consider is that there are patients with T2DM and low or moderate risk, and the document provides lax therapeutic recommendations for this group of patients.
It is recommended to apply tight glycemic control (HbA1c <7%) when other societies support the target <6.5% if it can be achieved with drugs with known CV benefit that do not cause hypoglycemia.3,4
Following the figure, the document establishes pharmacological treatment recommendations according to the patient profile: a) SGLT2i and GLP-1 RA with separate recommendations for patients with and without ASCVD with severe TOD; b) SGLT2i are recommended for the treatment of HF in patients with diabetes across the entire spectrum of left ventricular ejection fraction; and c) SGLT2i and finerenone are recommended for patients with CKD.
These therapies are recommended independently of glucose control and in addition to standard of care. The remaining recommendations do not vary with respect to previous guidelines.
Heart failure and type 2 diabetes mellitusThe poor prognosis of patients with T2DM and HF is the main reason to recommend screening in all patients to allow early diagnosis of HF and treatment implementation. A systematic evaluation of signs and symptoms followed by the algorithm for HF diagnosis, including NTproBNP measurement, is indicated. The prognostic benefit of HF screening with NTproBNP in asymptomatic patients remains a gap in the evidence. The treatment of HF in patients with T2DM is in accordance with the ESC guidelines on HF. The management of T2DM should prioritize treatments that provide CV benefits with proven safety. SGLT2i are recommended in all patients regardless of left ventricular ejection fraction, HbA1c, and concomitant glucose-lowering medication. For additional glucose control, GLP-1 RA, sitagliptin, linagliptin, insulin or metformin should be added although they have neutral effects on the risk of hospitalization for HF. Pioglitazone and saxagliptin are not recommended.
Chronic kidney disease and type 2 diabetes mellitusCKD has a major effect on morbidity and mortality in patients with T2DM. Routine evaluation of estimated glomerular filtration rate (eGFR) and urine albumin-to-creatinine ratio (UACR) is indicated. Treatment of patients with T2DM and CKD aims to reduce the risk of CV events and renal failure and should be started early. Blood pressure control, SGLT2i (if eGFR ≥ 20mL/min/1.73 m2), finerenone (if eGFR >60mL/min/1.73 m2 with UACR ≥ 30mg/mmoL or eGFR 25-60mL/min/1.73 m2 and UACR ≥ 3mg/mmoL), statins and an angiotensin-converting enzyme inhibitor or angiotensin-II receptor blocker are indicated. Personalized HbA1c targets (between 6.5% and 8%) are suggested, although HbA1c <7% is recommended to reduce microvascular complications. For additional glucose control, GLP-1 RA (if eGFR>15mL/min/1.73 m2) are recommended due to the low risk and beneficial CV effects. Metformin (if eGFR >30mL/min/1.73 m2), dipeptidyl peptidase-4 inhibitor, or insulin are alternatives.
Ischemic heart disease and type 2 diabetes mellitusRecommendations for antithrombotic therapy have been strengthened in these guidelines based on the increased risk of thrombosis in patients with diabetes. In chronic coronary syndromes (CCS), clopidogrel is recommended in addition to aspirin for 6 months after coronary stent implantation, regardless of the type of stent used. The guidelines suggest considering the addition of low-dose rivaroxaban to low-dose aspirin for long-term prevention of vascular events in patients with CCS or symptomatic peripheral arterial disease (PAD) without a high risk of bleeding (not reimbursed in Spain). In patients with acute coronary syndromes (ACS) and diabetes undergoing percutaneous coronary intervention (PCI), ticagrelor or prasugrel are recommended in addition to aspirin and should be continued for 12 months. However, we should consider extending dual antiplatelet therapy beyond 12 months to up to 3 years in patients who have tolerated it without major bleeding complications. In patients with ACS or CCS undergoing PCI who have an indication for anticoagulation, triple therapy is recommended for 1 week, but could be extended to 1 month or even 3 months if the thrombotic risk outweighs the bleeding risk. This strategy is not mentioned in the ESC guidelines on SCA.5
The therapeutic strategy and revascularization techniques in patients with diabetes should not differ from those in patients without diabetes: use of drug-eluting stents, radial approach for PCI, and the use of the left internal mammary artery as a graft for coronary artery bypass grafting. The guidelines emphasize the indication for complete revascularization in ACS patients without cardiogenic shock and with multivessel disease. Of note, according to current knowledge, coronary artery bypass grafting with arterial grafts is preferred to complex PCI in patients with multivessel disease, if the patient's comorbidities are considered.
CONSEQUENCES OF THE IMPLEMENTATION OF THE GUIDELINES IN DIABETESCardiovascular and renal protection. ObesityIn patients with diabetes, assessment of CV risk is still recommended in this update, by evaluating the clinical history and the presence of symptoms suggestive of ASCVD, without specific additional tests initially.
A highly important step forward is the focus on CV and renal protection of patients with T2DM as emphasized in the Spanish Society of Cardiology consensus3: in patients with very high CV risk related to the presence of ASCVD, SGLT2i and GLP-1, RA are recommended regardless of glycemic control or patient weight and based on the results of several CV outcome trials. At the same level of recommendation as SGLT2i in T2DM and HF, finerenone is recommended in patients with T2DM and CKD, based on the evidence for the management of this patient population.
There is no specific section to address obesity, which is highly prevalent in Spain,6 or highlighting weight loss in patients with diabetes.
Type 1 diabetes mellitusRegarding type 1 diabetes mellitus (T1DM), the guidelines do not have significant updates. They do not specify CVD risk assessment or address vascular disease prevention and treatment. Statin use is suggested for T1DM patients aged >40 (or <40 years and other risk factors, microvascular end-organ damage or 10-year CVD risk ≥ 10%) to reduce CVD (IIaB recommendation). Emphasis is placed on intensive blood glucose management, patient self-management supervised by a multidisciplinary team, and avoidance of hypoglycaemia, especially in patients with established vascular disease.
Gender considerations: gestational diabetes and sex differencesIn the context of gestational diabetes, the adoption of the ‘one-step’ 75 g oral glucose tolerance test for diagnosis and the recommendation for postpartum testing represent important shifts in practice. The guidelines underscore the need for lifelong annual diabetes screening for women with a history of gestational diabetes, acknowledging their elevated risk. Moreover, the recognition of an increased CV risk in these individuals, even with normal postpartum glucose levels, requires regular CV health screening.
Regarding sex-specific considerations, the guidelines emphasize the importance of careful drug selection during pregnancy to prevent potential fetal effects, especially with drugs such as renin-angiotensin system blocking drugs. The recommended blood pressure targets during pregnancy (110-135mmHg/80-85mmHg) aim to improve pregnancy outcomes. For individuals with T2DM, particularly women, who often exhibit greater blood pressure differences and a higher prevalence of hypertension, tailored care is essential. There is a markedly elevated risk of HF with preserved ejection fraction in women, especially in the presence of diabetes. The document makes no reference to other sex-specific risk factors such as premature menopause, preterm delivery, polycystic ovary syndrome, or systemic inflammatory and autoimmune disorders. Epidemiological data suggest diabetes poses a greater CV risk for women than men, but clinical trials show that the effectiveness of treatment is similar. However, real-world data reveal an unequal application of guidelines-directed therapy. Women's underrepresentation in trials highlights the unequal application of treatment, requiring gender-balanced recruitment, sex-specific analyses, and equitable health care access for women in diabetes-related CV care.
Aortic and peripheral arterial diseases and diabetesRegular screening for peripheral arterial diseases (PAD) is recommended, with clinical assessment and/or ankle-brachial index measurement. There are no new differences in the approach to PAD in persons with or without T2DM.
A treadmill test is useful in patients with intermittent claudication for assessing walking distance. Patients with intermittent claudication should take part in exercise training programs (30-45minutes, at least 3 times per week), as regular intensive exercise improves walking distance, but no recommendation level is given.
Atrial fibrillationThe guidelines emphasize the early detection of AF, with the following screening recommendations: opportunistic screening for AF by pulse taking or ECG is recommended in patients aged ≥ 65 or <65 years when other risk factors are present, because patients with diabetes exhibit a higher AF frequency at a younger age. In addition, systematic ECG screening should be considered to detect AF in patients aged ≥ 75 years, or those at high risk of stroke.
Patient education, exercise prescription, and nursing contributionThe guidelines emphasize the need for an integrated approach with contributions from several disciplines and areas of specialization that work together and focus on patients with diabetes and their families. In addition to pharmacological treatment, dietary and exercise educational interventions can significantly reduce not only body mass index or HbA1c but also the risk of microvascular complications and cardiovascular diseases in these patients. The Mediterranean diet is a new IA recommendation. Electronic cigarettes are discouraged, although a level of recommendation is missing. Individualized education programs appear to be more effective than group programs, whether carried out in person or through telemedicine.
It is recommended to increase any physical activity (eg, 10minutes of walking daily) in all patients with T2DM with or without CVD. Optimal physical activity is defined as weekly activity of 150minutes of moderate intensity or 75minutes of vigorous intensity.
It is recommended that both adults and older adults perform resistance exercise in addition to endurance exercise at least twice a week. Exercise interventions should be adapted to associated comorbidities, eg, frailty, neuropathy, or retinopathy. It is recommended to introduce structured exercise training in patients with T2DM and established CVD to improve metabolic control, exercise capacity, and quality of life, and to reduce CV events.
One of the most innovative aspects of this guidelines is the “person-centered care” approach, which encourages the participation of patients with diabetes and their families/caregivers in the disease process. Cultural, socioeconomic, and psychological factors take on special importance. Baseline clinical status, including frailty and comorbidities, and individual cognitive and emotional factors are of great importance.
Patient follow-up by a multidisciplinary team and the use of cognitive-behavioral techniques are proposed. To reduce the burden of the disease and improve self-care, a personalized treatment strategy is proposed, with shared decisions that consider patients’ preferences.
Type 2 diabetes mellitus in older patientsT2DM is more common in older adults, who are usually overweight or obese. However, these guidelines provide few specific recommendations related to older patients, who are often excluded, or underrepresented in studies and clinical trials.7 The SCORE2-Diabetes refers only to patients aged 40 to 69 years.
It is recommended to individualize HbA1c targets according to comorbidities, diabetes duration, and life expectancy. The current recommendations include lenient glycemic targets (HbA1c <69 mmoL/moL or <8.5%) and avoiding hypoglycemia in patients with short life expectancy. In patients with longer life expectancy, the use of agents with proven CV benefits and low hypoglycemic risk should be prioritized. It is recommended to adapt physical activity and exercise to associated comorbidities and frailty status.
Finally, age is a risk factor for HF development, which is frequent in these patients.
GAPSLipids and diabetes mellitusThe guidelines refer very briefly to atherogenic dyslipidemia in T2DM, in which there is an imbalance of triglyceride-rich lipoproteins containing apolipoprotein (Apo)B and those containing ApoA1 like high-density lipoprotein (HDL). This is fundamental to understanding the pathophysiological mechanism of this metabolic alteration, in which insulin resistance in diabetic patients plays a fundamental role.
There are no changes in targets, with low-density lipoprotein (LDL) being the main target (very high cardiovascular risk <55mg/dL and 50% reduction; high cardiovascular risk <70mg/dL and 50% reduction; moderate cardiovascular risk <100mg/dL). Although a slight mention is made about the non-HDL target, there is no mention of non-HDL or ApoB targets.8 There is evidence of the relationship of ApoB and non-HDL cholesterol with increased CV risk. These have even been considered secondary targets in patients with diabetes and obesity in the 2019 dyslipidemia treatment guidelines and in the CV prevention guidelines of 2021.9,10 The atherogenic dyslipidemia of T2DM is characterized by lower density and smaller lipoproteins. Therefore, the measurement of LDL (mg/dL) alone could underestimate the true risk, with ApoB or non-HDL cholesterol being a complementary and necessary marker of lipid risk.
Statins remain the standard of care and include treatment with ezetimibe and PCSK9i as IB and IA recommendations, respectively, but the guidelines continue to recommend tiered therapy across the board without reference to the possibility of intensive (combined) lipid-lowering therapy adjusted for baseline LDL levels and CV risk control targets. The document does not include bempedoic acid as part of treatment,11 despite positive results in reducing CV events and demonstrated safety in diabetic patients.
There are no references to the measures that could be adopted both in lifestyle changes and in the drugs used as antidiabetic agents that could have an impact on the improvement of atherogenic dyslipidemia, such as GLP-1 RA.
Other important gaps in cardiovascular prevention and obesityA weak point of these guidelines is that they no longer cover prediabetes, leaving aside a population at high CV risk that needs to be treated differently than the population with normoglycemia.
Most patients with T2DM (90%) have high or very high CV risk, and the application of SCORE2-Diabetes to estimate 10-year CVD risk in patients without symptomatic ASCVD or severe TOD may not reflect the true risk.
We also miss the opportunity to transfer the impact of CV outcomes of GLP-1 RA or the dual agonist beyond body weight reduction.
Given the additional beneficial effects of GLP-1 RA and SGLT2i on CV outcomes in T2DM, it is surprising that the benefits in obese individuals with T2DM are not mentioned.
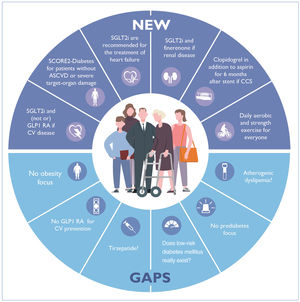
SUMMARYThe main points, as shown on figure 1, are as follows:
- -
The new SCORE2-Diabetes to estimate 10-year CVD risk in patients without symptomatic ASCVD or severe TOD may limit patient access to recommended SGLT2i and GLP-1 RA, with a potentially significant impact on prognosis.
- -
The guidelines define prediabetes criteria but lack references to cardiovascular risk assessment, and care management recommendations.
- -
The absence of a specific section on obesity is a missed opportunity to raise awareness of the direct relationship between obesity and T2DM, and with AF, CVD, and HF.
- -
The document does not focus on atherogenic dyslipidemia.
- -
The main guideline recommendations focus on the treatment of macrovascular complications in patients with ASCVD, HF, or CKD, rather than on their prevention. Patients with diabetes should be considered as potentially developing these 3 complications and treatment should aim to prevent them from the outset.
Central illustration. What is new and what are the gaps in the new ESC 2023 guidelines on diabetes? ASCVD, atherosclerotic cardiovascular disease; CCS, chronic coronary syndromes; CV, cardiovascular; GLP RA, glucagon-type peptide-I receptors agonists; SGLT2i, sodium-glucose co-transporter-2 inhibitors.
The authors encourage readers to consult the full text of the ESC 2023 guidelines to delve deeper into specific details and improve their daily practice.
FUNDINGNone.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCENo artificial intelligence has been used.
CONFLICTS OF INTERESTThe conflict-of-interest declaration documents of all authors can be seen in the supplementary data.
SEC Working Group for the 2023 ESC guidelines on cardiovascular disease in patients with diabetes: Raquel Campuzano Ruiz (coordinator), Pilar Mazón Ramos (coordinator), Almudena Castro Conde, Belén Cid Álvarez, Concepción Cruzado Álvarez, Pablo Díez-Villanueva, Rosa Fernández Olmo, Román Freixa-Pamias, Domingo Marzal Martin, Sonia Mirabet Pérez.
SEC Guidelines Committee: José Luis Ferreiro (president), Pablo Avanzas (secretary), Rut Andrea, Araceli Boraita, David Calvo, Raquel Campuzano, Victoria Delgado, Laura Dos Subirá, Juan José Gómez Doblas, María Antonia Martínez Momblan, Pilar Mazón, Domingo Pascual Figal, Juan Sanchis, José María de la Torre Hernández, David Vivas.
The names of all the authors of the article are listed in alphabetical order in Appendix A.
See related article: https://secardiologia.es/cientifico/guias-clinicas/miscelanea/14536-2023-esc-guidelines-for-the-management-of-cardiovascular-disease-in-patients-with-diabetes
Corresponding author.
E-mail addresses:raquel.campuzano@salud.madrid.org (R. Campuzano); pilarmazon@yahoo.es (P. Mazón Ramos).