This study aimed to compare stress echocardiography (SE) and multidetector computed tomography (MCT) in patients admitted to a chest pain unit to detect acute coronary syndrome (ACS).
MethodsA total of 203 patients with ≥ 1 cardiovascular risk factor, no ischemic electrocardiogram changes and negative biomarkers were randomized to SE (n=103) or MTC (n=100). The primary endpoint was a combination of hard events (death and nonfatal myocardial infarction), revascularizations, and readmissions during follow-up. The secondary endpoint was the cost of the 2 strategies.
ResultsInvasive angiography was performed in 61 patients (34 [33%] in the SE group and in 27 [27%] in the MCT group, P=.15). A final diagnosis of ACS was made in 53 patients (88% vs 85%, P=.35). There were no significant differences between groups in the primary endpoint (42% vs 41%, P=.91), or in hard events (5% vs 7%, P=.42). There were no significant differences in overall cost, but costs were lower in patients with negative SE than in those with negative MCT (€557 vs €706, P <.02).
ConclusionsNo significant differences were found in efficacy and safety for the stratification of patients with a low to moderate probability of ACS admitted to a chest pain unit. The cost of the 2 strategies was similar, but cost was significantly lower for SE on comparison of negative studies.
Keywords
Approximately 5% of patients attending an emergency department due to chest pain with nondiagnostic electrocardiography and negative biomarkers for myocardial injury have an acute coronary syndrome (ACS).1,2 Traditionally, stress testing has been an essential part of the protocol used by chest pain units (CPUs).3,4 Alternative strategies are now available for more accurate stratification of these patients, for instance, stress echocardiography (SE),5–7 gated myocardial perfusion SPECT,8 and multidetector computed tomography (MDCT).9–11 Various studies have compared MDCT-based evaluation with standard evaluation,12 both in CPUs and with stable coronary disease (CD). Almost all these studies used conventional evaluation consisting of a stress test without imaging for most patients.
The aim of our study was to analyze the clinical and financial impact of SE vs MDCT in stable patients with a low-to-intermediate probability of CD who had been assessed in a CPU.
METHODSPatientsPatients were included if aged 18 to 80 years, with 1 or more cardiovascular risk factors, and referred to our CPU from the Emergency Department with suspicion of ACS, nondiagnostic ECG, and negative serial tests for markers of myocardial injury. Other requirements were last pain episode at least 12hours earlier, at least 2 ECGs performed a minimum of 6 to 12hours apart, and troponinI≤0.3mg/dL (2 or more measurements at least 6hours apart). Patients were excluded if they had a history of stent implantation, inability to perform a prolonged breath-hold (10-15s), irregular heart rate, contraindication for beta-blockers if heart rate was >65bpm or systolic blood pressure was <100mmHg, contraindication for atropine, allergy to iodinated contrast material, pregnancy, or creatinine>1.3mg/dL.
The study was approved by the Clinical Research Ethics Committee of Galicia, and all patients provided signed informed consent. Patients were assigned during office hours (8:00 a.m. to 3:00 p.m.) by a procedure based on random numbers, once they had been assessed by a cardiologist and all inclusion and exclusion criteria had been checked. Patients referred outside normal office hours remained hospitalized until they could be assessed by a cardiologist, and if referred over the weekend, they stayed until Monday. Randomization was not consecutive because the scanner was only available to the study 1 day a week, due to normal clinical practice needs. The primary endpoint was a combination of serious events (death and nonfatal myocardial infarction [MI]), revascularizations, and readmissions. The secondary endpoint was the cost of each technique.
Stress echocardiography protocolStress testing was performed using an individualized protocol based on each patient's clinical characteristics (Bruce or Naughton), along with 2-dimensional echocardiogram at rest, peak exercise, and postexercise (at 1minute). If exercise was impossible, dobutamine administration was considered. A wall motion score index was used, based on the 16-segment model proposed by the American Society of Echocardiography.13 If 85% of the theoretical maximum heart rate was not achieved, intravenous atropine was used (up to 2mg). A new contractility abnormality or worsening from baseline in 2 adjacent segments was considered ischemia. Isolated hypokinesia of the inferobasal or septobasal segment was not considered ischemia unless an adjacent segment was affected.14 Involvement of at least 3 segments was considered to be extensive ischemia, and multivessel ischemia was defined as the development of segmental motility abnormalities in more than 1 coronary territory. Akinetic areas that remained unchanged or became dyskinetic were considered necrosis. The presence of ischemia was considered to be positive SE.
Multidetector computed tomographyA 64-detector CT scanner was used for all MDCT scans. Patients were administered an intravenous bolus of iodinated contrast material, and angiography was performed once 120 HU was reached in the ascending aorta. Dose-sparing techniques were used, optimizing acquisition at 30% to 70% of the range. If the heart rate was >65 bpm, patients received preprocedure intravenous atenolol under continuous electrocardiographic monitoring. Narrowing>50% in any coronary arteries or branches was considered significant.
Suspicion of acute coronary syndromePatients with echocardiographic ischemia in the SE group and patients with narrowing>50% in any coronary arteries or branches were referred for coronary angiography. Suspicion of ACS was confirmed when the coronary angiography showed narrowing>50% in any coronary arteries or branches in the territory that was positive using the classification technique. Patients were discharged if the triage results were negative. During follow-up, treatment was started or switched as deemed necessary by the attending physician.
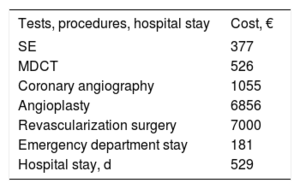
CostCosts were calculated from the time of randomization, including the costs for each technique, diagnostic coronary angiography, percutaneous or surgical revascularization, and number of days of hospitalization until medical discharge of the index event. The hospital stay was calculated from randomization to discharge of the index event, including revascularization. Table 1 lists the costs used, based on more recent economic data from our setting.15
Cost of diagnostic tests, revascularization, and hospital stay
| Tests, procedures, hospital stay | Cost, € |
|---|---|
| SE | 377 |
| MDCT | 526 |
| Coronary angiography | 1055 |
| Angioplasty | 6856 |
| Revascularization surgery | 7000 |
| Emergency department stay | 181 |
| Hospital stay, d | 529 |
MDCT, multidetector computed tomography; SE, stress echocardiography.
Prepared from the most recent economic data for our setting.15
Quantitative variables are expressed as proportions that reflect the percentage in each group, and qualitative variables are expressed as the mean±standard deviation. An intention-to-treat analysis was performed, and qualitative variables for both groups were compared using the chi-square test. For quantitative variables, a comparison of means test (Student t test) was used. For the survival analysis, the Kaplan-Meier estimator was used. A sample size of 182 patients was calculated in each group by assuming a combined-event rate of 30% in the SE group and to show a 43% decrease in the event rate in the MDCT group16,17 with a 95% significance level and 80% power. A Pvalue <.05 was considered statistically significant.
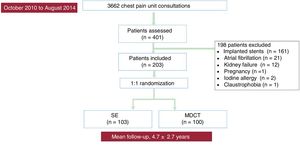
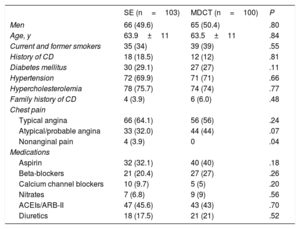
RESULTSA total of 203 patients were included between October 2010 and August 2014. Figure 1 contains the flow chart for the study. Patients’ baseline characteristics are listed in table 2. Most patients had a low TIMI score18 (68% in TIMII and 32% in TIMIII), with no differences observed between the 2 strategies (P=.37).
Patients’ baseline characteristics
| SE (n=103) | MDCT (n=100) | P | |
|---|---|---|---|
| Men | 66 (49.6) | 65 (50.4) | .80 |
| Age, y | 63.9±11 | 63.5±11 | .84 |
| Current and former smokers | 35 (34) | 39 (39) | .55 |
| History of CD | 18 (18.5) | 12 (12) | .81 |
| Diabetes mellitus | 30 (29.1) | 27 (27) | .11 |
| Hypertension | 72 (69.9) | 71 (71) | .66 |
| Hypercholesterolemia | 78 (75.7) | 74 (74) | .77 |
| Family history of CD | 4 (3.9) | 6 (6.0) | .48 |
| Chest pain | |||
| Typical angina | 66 (64.1) | 56 (56) | .24 |
| Atypical/probable angina | 33 (32.0) | 44 (44) | .07 |
| Nonanginal pain | 4 (3.9) | 0 | .04 |
| Medications | |||
| Aspirin | 32 (32.1) | 40 (40) | .18 |
| Beta-blockers | 21 (20.4) | 27 (27) | .26 |
| Calcium channel blockers | 10 (9.7) | 5 (5) | .20 |
| Nitrates | 7 (6.8) | 9 (9) | .56 |
| ACEIs/ARB-II | 47 (45.6) | 43 (43) | .70 |
| Diuretics | 18 (17.5) | 21 (21) | .52 |
ACEIs, angiotensin-converting enzyme inhibitors; ARBs: angiotensin II receptor antagonists; CD, coronary disease; MDCT, multidetector computed tomography; SE, stress echocardiography.
Data are expressed as No. (%) or mean±standard deviation.
Treadmill testing was possible in the 103 patients in the SE group, and the conventional Bruce protocol was used in most (96%) of these patients. In the remaining 4%, the modified Bruce protocol was used. Echocardiography contrast was not necessary for any patients. A total of 16 (15%) patients were administered intravenous atropine (1.3±0.4mg); 5 patients had an inconclusive result because 85% of the theoretical maximum heart rate was not achieved; 2patients were admitted for coronary angiography, and the remaining 3 were discharged (2 due to negative results, but having achieved 10 metabolic equivalents; 1 due to normal coronaries seen in a previous hospitalization). The SE was positive for ischemia in 36 (35%) patients, whereas necrosis was detected without associated ischemia in 2(2%) cases. The wall motility score index was 1.05±0.17 at baseline and 1.20±0.33 at peak exercise. Among the 36patients with echocardiographic ischemia, 34were referred for coronary angiography and the suspected diagnosis was confirmed in 30(88%). Hospitalization and coronary angiography were not undertaken in 2patients (1 declined invasive study; 1 opted for medical therapy due to CD precluding revascularization in a previous coronary angiogram).
Multidetector computed tomographyA total of 100 patients were randomized to MDCT. Intravenous atenolol (2.8±1.3mg) was administered in 46% of scans. Due to motion artifacts, 6studies were considered inconclusive. Three of these patients then underwent SE, which was negative. No study in the MDCT group was inconclusive as a result of excessive coronary calcification. MDCT was positive in 27patients. The diagnostic suspicion was confirmed in 23(85%) by coronary angiography.
Acute coronary syndromeA total of 142 (70%) patients were discharged from the Emergency Department, and the remaining 61 (30%) were hospitalized. ACS was confirmed in 53 (87%) of 61patients referred for coronary angiography: 30(88%) of 34patients referred for coronary angiography in the SE group and 23(85%) of 27patients referred for coronary angiography in the MDCT group (P=.35). More than half the patients (30 [60%]) had multivessel disease. Most patients admitted for coronary angiography also underwent revascularization (9 by surgery, 40 by percutaneous intervention). Four patients were medically treated: 2 due to CD precluding revascularization and 2 due to chronic occlusion and minimal territory at risk.
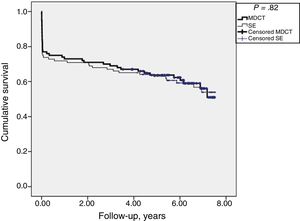
EventsMean follow-up was 4.7±2.7 years, with no significant differences found in the primary endpoint (43 [42%] patients in the SE group and 41 [41%] in the MDCT group; P=.91). Figure 2 shows the Kaplan-Meier curves for survival free of events, revascularizations, and readmissions for the 2 groups. A total of 5 serious events were recorded in the SE group and 7 in the MDCT group (5% vs 7%; P=.42). There were 8deaths (3 in the SE group and 5 in the MDCT group; P=.39) and 4 nonfatal MIs (2 in the SE group and 2 in the MDCT group; P=.51). The cause of death was cardiovascular in 4 patients (1 after inferior MI at 1223days, 1 sudden death at 1967days, 1 death due to intestinal ischemia, and 1 death due to prosthetic dysfunction), cancer-related in 3, and unknown in 1. During the first year of follow-up, there was only 1 serious event: a nonfatal MI with anterior ST-segment elevation in a patient from the MDCT group. The remaining 3 nonfatal MIs occurred 1647±542 days after randomization. There were also no significant differences between the 2 groups in combined events of serious event and revascularization (35 [34%] patients in the SE group and 29 [29%] in the MDCT group; P=.58). A total of 21 (10%) new CPU visits were recorded (9 in the SE group and 12 in the MDCT group); in the first year, 3 were in the SE group and 4 in the MDCT group.
The mean stay after randomization was less than 7hours for patients with a negative result. The median hospital stay for patients referred for positive or inconclusive coronary angiography results was 7 (range, 5-10) days in the SE group and 8 (range, 5-10.25) days in the MDCT group (P=.90). There were no significant differences in the overall cost of either technique: €3872±€5363 with the SE strategy and €3033±€4120 with the MDCT strategy (P=.21). There were also no significant differences when comparing the cost of positive SE vs positive MDCT (€9682±€5294 and €9020±€3342; P=.57). However, costs were lower in patients with negative SE than in those with negative MDCT (€557with negative SE and €706with negative MDCT; P=.02).
Number of postrandomization testsSignificant differences were found in the number of echocardiograms performed during follow-up (31 [30%] patients in the SE group and 46 [46%] in the MDCT group; P=.01), as well as in the number of stress tests (4 [4%] patients in the SE group and 14 [14%] in the MDCT group; P=.01). The number of SEs performed was similar in the 2 groups (26 [25%] in the SE group; 28 [28%] in the MDCT group; P=.38). MDCT was performed in only 2patients in the SE group [2%] and in none of the MDCT patients; P=.25).
DISCUSSIONThis prospective, experimental, randomized, single-center study analyzed the clinical safety and financial cost of 2 techniques: an anatomic method (MDCT) and a functional method (SE at peak exercise) during triage of patients referred to our CPU with a low-to-intermediate probability of ACS. No significant differences in safety or efficacy were found between the 2 techniques, with lower costs in patients from the SE group not requiring hospitalization. Most patient exclusions were due to clinical characteristics that would have prevented accurate assessment with the MDCT strategy.
Anatomic strategy vs functional strategy in acute situationsVarious studies have shown that MDCT is a safe triage alternative for CPU patients with suspicion of ACS. However, vastly different strategies were used in these studies for comparison with MDCT, and certain patients were even discharged with no further testing. A recent meta-analysis12 compared the MDCT strategy with the conventional strategy in both acute and chronic cases. In acute cases, with 2919patients included in the total, no differences were found in prognosis, but there was a significant increase in the number of coronary angiograms and revascularizations with the anatomic strategy. However, most of these studies compared MDCT with conventional stress testing, which has limitations related to low sensitivity and specificity. When a stress imaging technique was used, it was almost always myocardial perfusion scan.8–10 Stress echocardiography could have advantages over nuclear perfusion techniques, particularly in the acute phase, because the technique produces rapid results, is able to detect nonmyocardial abnormalities as the cause of symptoms, has fewer contraindications, and is free of radiation. Additionally, the sensitivity of the technique is improved when peak exercise imaging is used.19–22 Very few studies have compared functional imaging by stress echocardiography with MDCT in a CPU. A previous Spanish study23 on SE and MDCT in the same patients concluded that MDCT was more sensitive but less specific than SE in the diagnosis of ACS, although the difference was not statistically significant. A recent multicenter study performed a head-to-head comparison of MDCT and dobutamine SE in 217patients in similar situations and found that MDCT was more sensitive (97% vs 52%) and had a higher negative predictive value (93% vs 52%) than SE, whereas specificity (48% vs 47%) and positive predictive value (67% vs 50%) were suboptimal and similar in both techniques.24 The PERFECT study randomized 411patients, half to SE and half to MDCT, and also found no differences in events, although more coronary angiograms and revascularizations were performed in patients who underwent MDCT.25 Another recent study also conducted in a CPU compared MDCT to SE exclusively.26 In the SE strategy, hospitalization was reduced (11% with the SE strategy vs 19% with the MDCT strategy; P=.026), as well as mean hospital stay, whereas no differences were found in cardiovascular events.
These data for acute situations differ from recent data on chronic situations, where the results were more favorable with MDCT, with fewer events reported during follow-up by the SCOT-HEART study27,28 but not by the PROMISE study.29 However, there are essential differences between these 2studies. The SCOT-HEART study actually compared conventional stress testing with MDCT added to conventional stress testing, whereas the PROMISE study compared MDCT with a functional strategy that mainly consisted of cardiac imaging with isotopes.
Acute coronary syndrome and coronary diseaseThe prevalence of ACS and obstructive CD was high (26%) in our series, in comparison with others, for example, 8% in the ROMICAT II study.9 Although more than half the patients included had a low risk of ACS (68% in TIMI I), unlike other studies, all had at least 1 cardiovascular risk factor, and most had at least 2 (94%). Furthermore, 15% had been diagnosed with CD in the past, an exclusion criterion in most earlier trials.9–11,22,24 Additionally, more than half the patients (30 [60%]) in the 2 groups had multivessel CD on coronary angiography. Last, the marker available in the emergency laboratory was conventional cardiac troponin I. If high-sensitivity troponin had been available, the diagnostic precision would likely have been improved in this population and more cases would have been detected and directly referred to coronary angiography with no need for triage techniques,30–32 thus reducing the pretest probability of ACS in the sample.
ACS was confirmed in 87% of patients referred for coronary angiography (88% in the SE group and 85% in the MDCT group). In a study by Mas et al.,23 the prevalence of coronary artery disease and ACS was also high (25%), and the suspicion was confirmed in fewer cases with both SE (67%) and MDCT (59%), with no significant differences. Most of our patients with ACS confirmed by one of the strategies underwent revascularization, unlike other studies in which more than half the patients admitted from emergency departments for coronary angiography were not revascularized.26
Follow-upThe follow-up of patients in our series was very long (more than 5 years in 62% of patients) with a similar number of ACS, revascularizations, and readmissions in the 2 groups and, therefore, this study seems to indicate similar outcomes for the SE and MDCT groups for the same length of time. The number of echocardiograms and conventional stress tests was significantly higher in the MDCT group during follow-up.
CostIn other studies, MDCT led to earlier diagnosis of ACS, although costs were not reduced and patients were more likely to undergo coronary angiography during hospitalization or follow-up.9,25,26 In the ROMICAT II study, emergency department costs were significantly lower in the MDCT group, although the overall cost until day 28 of follow-up was similar in the 2 groups. Our series showed no significant differences in overall cost, although the cost in the negative SE group was significantly lower than that of the negative MDCT group.
LimitationsFirst, this study was conducted at a single center study and had a small sample, which limits generalization. Unfortunately, due to the low availability of MDCT for this study, it was not possible to achieve a sufficient sample size to detect differences between the 2 strategies and, therefore, the null hypothesis cannot be rejected. Consequently, our study can only be considered an exploratory analysis. Nevertheless, the findings could provide a rationale for further studies along these lines. Another limitation is that the primary endpoint is a combination of events that have dissimilar clinical implications. Patient screening excluded any patients who were unable to undergo the technique or who had a contraindication for it, circumstances considered normal in clinical practice (eg, prior stents, atrial fibrillation, kidney failure). The marker used was conventional cardiac troponin I, which is less precise in diagnosing MI than high-sensitivity troponin.30–32 The physicians who performed and interpreted the tests were aware of the patients’ medical history, and the attending physicians and interventional cardiologist were likewise aware of the imaging technique result, which is a bias for the ACS diagnosis. Another bias that should be taken into account when ensuring an ACS diagnosis in the context of CD, primarily with multivessel disease and intermediate lesions, was that intracoronary techniques were rarely used, and always on orders from an interventional cardiologist. Costs did not include expenses for the hospital stay until randomization or expenses due to new visits or admissions, which lowers the overall cost reported.
CONCLUSIONSNo significant differences in safety and efficacy were found between SE and MDCT during the triage of acute chest pain in patients with a low-to-intermediate probability of ACS. However, costs were lower in patients with negative SE than in those with negative MDCT. The number of additional tests performed was also lower when an SE-based strategy was initially used.
CONFLICTS OF INTERESTNone declared.
- –
MDCT and SE are safe and effective techniques used to study patients with known or suspected CD. However, only a few studies have compared the 2 techniques in an acute setting.
- –
Additionally, a strategy using SE based mainly on exercise echography is rarely used, but could have advantages in CPUs, in view of its versatility, prompt results, comorbidity study, and absence of radiation.
- –
No significant long-term differences in safety and efficacy were found between SE and MDCT during the triage of patients with acute chest pain and a low-to-intermediate probability of ACS; however, costs were lower when MDCT was negative.
- –
Subsequent tests were also performed less often with the SE strategy.