The influence of the delay between diagnosis and surgery in severe tricuspid regurgitation (TR) remains controversial. We aimed to analyze the association between delay to surgery and operative and mid-term mortality in patients with severe TR concomitant to left-valve surgery.
MethodsWe conducted an observational retrospective study analyzing risk factors in patients undergoing left-valve surgery concomitant with severe TR. The clinical and demographic variables were prospectively collected. The time of first diagnosis of TR was retrospectively collected.
ResultsA total of 253 patients were analyzed. TR was functional in 82.6%. The median latency between diagnosis and surgery was 24 months. Operative mortality was 12.2%. On multivariate analysis, higher operative mortality was associated with older age, worse preoperative NYHA functional class, triple valve surgery, hyponatremia, and anemia. The median follow-up was 35 months. Survival at 1 and 5 years was 85.2% and 73.7%, respectively. Mortality during follow-up was associated with male sex, preoperative massive TR, and longer latency between diagnosis and surgery.
ConclusionsThe variables related to worse preoperative functional class were associated with increased operative mortality. Lower mid-term survival was associated with longer latency between diagnosis of severe TR and surgery, massive preoperative TR, and older age.
Keywords
Severe tricuspid regurgitation (TR) may remain clinically silent for a prolonged period, as symptoms and signs of right ventricular dysfunction may be masked by diuretic therapy. Right heart (RH) dysfunction is an independent risk factor for operative mortality, postoperative complications, and TR recurrence after tricuspid valve repair.1,2 Delayed surgery is associated with poor results and decreased survival.1 Some authors have suggested that avoiding surgical delay in severe TR might decrease operative mortality and the development of RH failure.1,3 However, the optimal timing of surgery is not clear. In patients undergoing left-sided surgery, the European (European Society of Cardiology][ESC]/ European Association for Cardio-Thoracic Surgery [EACTS]) and American (American Heart Association [AHA]/American College of Cardiology [ACC]) guidelines recommend tricuspid valve surgery in symptomatic patients with severe primary TR (recommendation class I level C ESC/EACTS), in patients with severe secondary TR (recommendation class I level B ESC/EACTS) and in patients with mild or moderate secondary TR associated with tricuspid annular dilatation (≥ 40 mm or>21 mm/m2) and RH failure (recommendation class IIa level B ESC/EACTS).4,5
In patients with concomitant left-sided surgery, severe TR is not the main surgical indication. We hypothesized that delayed intervention in severe TR might increase operative mortality, allowing the development of RH dysfunction. We aimed to analyze the influence of latency between diagnosis and surgery in operative and mid-term mortality and the factors associated with mortality during follow-up in patients with severe TR concomitant to left-valve surgery. As secondary objective, we aimed to identify the factors associated with postoperative RH failure.
METHODSWe conducted a retrospective and longitudinal study with a cohort design in patients older than 18 years with a diagnosis of severe TR concomitant to left-valve disease undergoing surgery. Clinical and demographic variables were prospectively collected. Time (in months) from first diagnosis of severe TR was retrospectively collected from echocardiographic patient information. The study was performed according to the strengthening the reporting of observational studies in epidemiology (STROBE) guidelines.6 The study protocol (identification number PI19-1435) received full approval by both the local Institutional research review committee and the clinical research ethics committee. The study period was from January 2012 to June 2020. We prospectively gathered data through follow-up of surviving patients. The patients were followed up either in person, by telephone, by contact with the cardiologist, and through medical records. No patients were lost to follow-up. All patients gave their written informed consent for analysis of their data.
DefinitionsOperative mortality was defined as in-hospital mortality or mortality occurring within 30 days of operation. Surgical risk was preoperatively estimated according to the European System for Cardiac Operative Risk (EuroSCORE) scales. Severity of tricuspid regurgitation was graded by echocardiography in 3 categories: severe TR was defined as an effective regurgitant orifice area (EROA) of ≥ 40 mm2 and a regurgitant volume (R Vol) of ≥ 45 mL. Massive TR was defined by EROA 60 to 79 mm2, R Vol 60 to 74 mL and vena contracta (VC) 14 to 20 mm and torrential TR was defined by EROA ≥ 80 mm2, R Vol ≥ 75 mL, and VC ≥ 21 mm.7 In line with the World Health Organization (WHO), anemia was defined as hemoglobin level under 12mg/dL in women and 13mg/dL in men, or lower than 2 standard deviations with respect to mean levels in the reference population.8 Postoperative RH failure was defined as symptoms and signs of persistent right ventricular dysfunction [right atrial pressure (RAP)> 18mmHg with a cardiac index <2.0 L/min/m2] in the absence of elevated pulmonary capillary wedge pressure [(PCWP) (> 18mmHg)], tamponade, ventricular arrhythmias or pneumothorax and RAP/PCWP ratio higher than 0.5 and/or tricuspid annular plane systolic excursion (TAPSE) <17 mm on echocardiography9 after the surgical procedure and before hospital discharge.
Statistical analysisStatistical analysis was performed using IBM SPSS Statistics for Windows, version 22.0, released in 2013 (IBM Corp, United States). Continuous variables are expressed as mean± standard deviation or as median and interquartile range [IQR], for nonnormal distributions. The Kolmogorov-Smirnov test was used to determine the normality of each variable. Categorical variables are expressed as absolute values and percentages. Association between variables was identified by the chi-square or Fisher exact test, when categorical, and by the Student t-test or Mann Whitney U-test, when continuous. The risk-adjusted mortality rate was calculated from the standardized mortality ratio. To obtain expected deaths, the logistic equation was adjusted according to the risk characteristics of the study population. The logistic equation for the EuroSCORE was obtained from Roques et al.10 To adjust time from severe TR diagnosis to surgery for confounding factors, logistic regression models were fitted with variables selected a priori. These were variables previously identified as independent predictors of mortality in patients undergoing concomitant tricuspid and left-sided valve surgery: age, time between diagnosis of severe TR and surgery, liver cirrhosis, New York Heart Association (NYHA) ≥ III, preoperative anemia, triple valve surgery, and preoperative values of sodium and proteins. The association between analyzed variables and operative mortality in univariate analysis (P <.2) was entered in backward and forward stepwise logistic regression models. The risk factors associated with increased mortality during follow-up and actuarial survival were analyzed using a Cox model and Kaplan-Meier test. A Harrell c-statistic was calculated for the Cox model of mortality during follow-up and postoperative RH failure. A P value <.05 was considered significant.
RESULTSA cohort of 253 consecutive patients with a diagnosis of severe TR concomitant to left-valve disease undergoing surgery were analyzed. The analyzed populations corresponded to 14.9% of patients who underwent valve surgery during the study period. The clinical and demographic variables are detailed in table 1. The etiology of severe TR was mostly functional (82.6%), although it could also be due to rheumatic heart disease (12.3%), infective endocarditis (2%), cardiac implantable devices (0.4%) and tricuspid valve repair failure (2.8%). The mean age of the patients was 69±9.5 years, with a predominance of the female sex (68.8%). Preoperative TR grade was severe in 81% of the patients and massive in the remaining patients. All patients underwent concomitant left-sided valve surgery: mitral in 64%, mitral and aortic in 24.1%, and aortic in 11.9%. The tricuspid valve interventions performed included 22 tricuspid valve replacements and 231 repairs. A total of 19.8% of patients had undergone at least 1 previous open-heart surgical intervention. TR after repair was moderate in 2 patients and none or mild the rest. Median latency between diagnosis of severe TR and surgery was 24 months, with an interquartile range (IQR) of 51 months.
Factors associated with operative mortality: univariate analysis
| Variable | Nonsurvivorsn=31 | Survivorsn=222 | P |
|---|---|---|---|
| Preoperative risk factors | |||
| Sex (female) | 18 (58.1) | 156 (70.3) | .170 |
| Hypertension | 21 (67.7) | 121 (54.5) | .164 |
| Smoke | 1 (3.2) | 20 (9) | .486 |
| Diabetes mellitus | 11 (35.5) | 50 (22.5) | .114 |
| Dyslipidemia | 12 (38.7) | 83 (37.4) | .887 |
| Cirrhosis | 3 (9.7) | 5 (2.3) | .061 |
| Peripheral vascular disease | 4 (12.9) | 23 (10.4) | .755 |
| Cerebrovascular disease | 0 (0) | 3 (1.4) | 1.000 |
| Preoperative anemia | 19 (61.3) | 68 (30.6) | .001 |
| Sinus rhythm | 5 (16.1) | 34 (15.3) | 1.000 |
| NYHA ≥ III | 26 (83.9) | 126 (56.8) | .004 |
| Age, y | 71.8±7.5 | 68.6±9.7 | .081 |
| Weight, kg | 67±10.4 | 68±12.4 | .982 |
| Height, cm | 159.8±9.2 | 159.7±8.3 | .949 |
| BMI | 26.5±4.1 | 26.5±4.3 | .968 |
| GFR, mL/min/1.73 m2 | 56.8±24.3 | 68.4±42.4 | .134 |
| Preoperative Na, mMol/L | 136.9±4.1 | 139.1±3.1 | <.0001 |
| Preoperative proteins, g/dL | 6.9±0.8 | 7.2±0.6 | .047 |
| Time from diagnosis to surgery, mo | 24 [79] | 24 [47.75] | .007 |
| Preoperative treatment* | |||
| Loop diuretics | 25 (80.6) | 164 (73.9) | .417 |
| Potassium-sparing diuretics | 8 (25.8) | 45 (20.3) | .478 |
| Thiazides | 1 (3.2) | 13 (5.9) | 1.000 |
| Loop diuretics (furosemide mg) | 40 [40] | 40 [40] | .340 |
| Potassium-sparing diuretics (spironolactone mg) | 0 [25] | 0 [0] | .777 |
| Thiazides (hidroclorothiazide mg) | 0 [50] | 0 [0] | .983 |
| Echocardiographic variables | |||
| Massive TR | 9 (29) | 39 (17.6) | .127 |
| Secondary TR | 4 (12.9) | 40 (18) | .617 |
| Concomitant tricuspid stenosis | 5 (6.5) | 5 (2.3) | .207 |
| LVEF | 62.1±10 | 59.7±8.5 | .148 |
| SPP, mmHg | 59.7±14.5 | 57.9±15.9 | .574 |
| Tricuspid diameter, mm | 42±3.2 | 40.8±5.3 | .293 |
| TAPSE, mm | 17.3±3.7 | 17.6±4 | .749 |
| Surgical variables | |||
| Redo surgery | 9 (29) | 41 (18.5) | .166 |
| Triple valve operation | 12 (38.7) | 49 (22.1) | .043 |
| Redo- tricuspid surgery | 0 (0) | 7 (3.2) | .602 |
| Tricuspid valve replacement | 4 (12.9) | 18 (8.1) | .325 |
| CPB time, min | 172.1 ± 57.4 | 137.4 ± 42.3 | <.0001 |
| Aortic clamp time, min | 122.3 ± 37.6 | 102.9 ± 30.3 | .001 |
| EuroSCORE logistic | 14.1 ± 10.2 | 9.8 ± 8.2 | .010 |
| EuroSCORE II | 13 ± 10.3 | 6.7 ± 6.1 | <.0001 |
| Postoperative variables | |||
| Postoperative right heart failure | 26 (83.9) | 38 (17.1) | <.0001 |
| ICU stay, d | 5 [8] | 4 [3] | .117 |
| Intubation time, h | 48 [160] | 7 [8] | <.0001 |
| In-hospital stay, d | 9 [14.2] | 12 [16] | .007 |
BMI, body mass index; CPB, cardiopulmonary bypass; GFR, glomerular filtration rate; ICU, intensive care unit; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; SPP, systolic pulmonary pressure.
Values are expressed as No. (%), mean±standard deviation, or median [interquartile range].
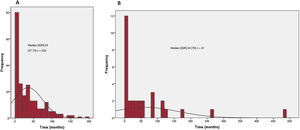
Operative mortality was 12.2%. The mortality of concomitant tricuspid and left-sided valve surgery was 9.9% among patients undergoing mitral valve surgery, 10% among patients undergoing aortic valve surgery, and 19.7% among those undergoing concomitant mitral and aortic valve surgery (P = .128). No significant differences were found in crude and standardized mortality ratios. The standardized mortality ratio was 1.28, 95% confidence interval (95%CI, 0.59-2.15) for concomitant tricuspid and mitral valve surgery; 0.80, 95%CI, 0.00001-1.88 for concomitant tricuspid and aortic valve surgery, and 1.92, 95%CI, 0.82-13.10 for concomitant tricuspid, mitral and aortic valve surgery. Although the mean latency between severe TR diagnosis and surgery was similar, a higher IQR was observed in nonsurvivors (figure 1) (P=.007)
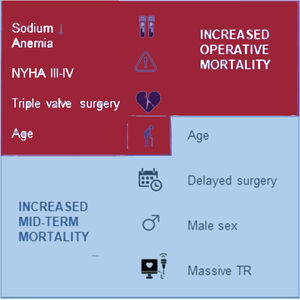
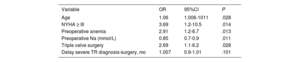
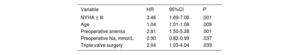
Age, triple valve surgery, worse functional status as assessed by NYHA functional class, and preoperative anemia and hyponatremia increased operative mortality (table 2). During the postoperative period, RH failure was diagnosed in 25.3% of all patients, which was the immediate cause of death in 32.8% of them. In the remaining patients, the immediate cause of death was hemorrhagic complications (4 patients), neurological damage (1 patient), respiratory disease (1 patient), left heart failure (2 patients) and infection (2 patients). The risk factors for postoperative RH failure are detailed in table 3.
Multivariate analysis: predictive variables for operative mortality
| Variable | OR | 95%CI | P |
|---|---|---|---|
| Age | 1.06 | 1.006-1011 | .028 |
| NYHA ≥ III | 3.69 | 1.2-10.5 | .014 |
| Preoperative anemia | 2.91 | 1.2-6.7 | .013 |
| Preoperative Na (mmol/L) | 0.85 | 0.7-0.9 | .011 |
| Triple valve surgery | 2.69 | 1.1-6.2 | .028 |
| Delay severe TR diagnosis-surgery, mo | 1.007 | 0.9-1.01 | .101 |
AUC=0.671; 95%CI, 0.573-0.770; P=.0001.
95%CI, 95% confidence interval; NYHA, New York Heart Association; OR, odds ratio; TR, tricuspid regurgitation.
Multivariate analysis: predictive variables for postoperative right heart failure
| Variable | HR | 95%CI | P |
|---|---|---|---|
| NYHA ≥ III | 3.46 | 1.69-7.06 | .001 |
| Age | 1.04 | 1.01-1.08 | .009 |
| Preoperative anemia | 2.81 | 1.50-5.28 | .001 |
| Preoperative Na, mmol/L | 0.90 | 0.82-0.99 | .037 |
| Triple valve surgery | 2.04 | 1.03-4.04 | .039 |
95%CI, 95% confidence interval; HR, hazard ratio; NYHA, New York Heart Association.
C-index=0.747; 95%CI, 0.680-0.814.
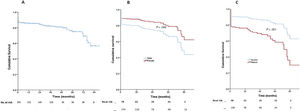
We conducted the follow-up of patients, with a mean time of 33.7±26.2 months, and median [IQR] of 35 [46.5] months. During this period, 11.3% of the patients died. Survival at 1 and 5 years was 85.2% and 73.7%, respectively (figure 2A). Male sex, latency from diagnosis of severe TR to surgery and preoperative diagnosis of massive TR were associated with higher mortality during follow-up, with c-index 0.687, 95%CI (0.611-0.765) (table 4 and figure 2B,C).
Cox regression: variables associated with higher mortality during follow-up
| Variable | HR | 95%CI | P |
|---|---|---|---|
| Age | 1.04 | 1.01-1.07 | .007 |
| Sex (male) | 1.85 | 1.08-3.22 | .025 |
| Masive preoperative TR | 2.58 | 1.48-4.51 | .001 |
| Delay severe TR diagnosis-surgery (months) | 2.11 | 1.002-1.008 | .035 |
TR, tricuspid regurgitation.
C-index=0.687; 95%CI, 0.611-0.765.
In this research, we first aimed to analyze the influence on operative and mid-term mortality of delay between diagnosis of severe TR and surgery in patients with concomitant left-valve surgery. We observed that mid-term mortality increased in patients with left-valve surgery associated with long-standing severe TR. The etiology of severe TR was mostly functional and, not infrequently, there was a latency of years between the first echocardiographic diagnosis and surgery. Surgical treatment in functional severe TR used to be influenced by the indications for left-heart valve surgery, facilitating temporal progression of TR until surgical decision. The progression of tricuspid valve disease reduced the mid-term survival of patients, even after adequate surgical correction.
Until now, the benefit of surgical correction of isolated functional TR compared with medical treatment has not been well established. Surgery should be considered early in selected symptomatic patients, but periprocedural morbidity and mortality is higher when patients present late and thresholds for severe RV dysfunction making intervention futile have not yet been defined.4,5 In this context, after diagnosis of nonsevere left-valve disease, aortic and/or mitral valve clinical and imaging studies prevail over evaluation of severe functional TR and usually determine the optimal surgical timing. Consecutively, the impact of the severity of tricuspid valve disease and right ventricular function remain underestimated. Since survival is affected, even after surgical correction of severe TR, a more exhaustive sequential echocardiographic study of the right ventricle and tricuspid valve would be advisable. In this setting, magnetic resonance imaging (MRI) can provide additional information that allows identification, over time, patients with higher surgical risk and lower mid-term survival.11
We also aimed to identify risk factors for mortality. Lower functional status was associated with increased operative mortality. We also found some preoperative biochemical markers related to an increase in operative mortality such as anemia and hyponatremia, which predicted a poor prognosis. The etiology of anemia in the study population was multifactorial: occult gastrointestinal bleeding secondary to chronic anticoagulant therapy, iron and vitamin B deficiencies, chronic disease (associated with an age-related inflammatory process)12 and dilutional anemia, associated with hyponatremia. All patients received chronic diuretic therapy before surgery and a quarter was under polytherapy with 2 or more diuretics; however, preoperative hyponatremia was related to increased operative mortality, regardless of the type and doses of diuretic treatment.
Compared with data described by other authors, crude mortality after concomitant tricuspid and left-sided valve surgery was higher in our population, but these differences were not significant when the risk-adjusted mortality rate was calculated.13–15 Nevertheless, triple valve surgery is associated with higher postoperative mortality due to right ventricular dysfunction, not related to repair or tricuspid valve replacement procedures16,17 (figure 3).
We also aimed to identify risk factors for postoperative RH dysfunction. Postoperative RH failure was observed in a quarter of patients undergoing tricuspid surgery and was the immediate cause of death in a third of them. The etiology of the postoperative RH failure was multifactorial. On the one hand, right ventricular function is reduced during cardiac surgery, independent of procedural characteristics18; on the other hand, preoperative anemia is an independent risk factor for low postoperative cardiac output.19 We observed an increased probability of postoperative RH failure after triple valve surgery; however, no correlation between preoperative right ventricular dysfunction and postoperative RH failure was identified. An explanation is that, in these patients, left-sided valve disease is the main indication for cardiac surgery and right ventricular dysfunction was underdiagnosed. Therefore, we consider that exhaustive preoperative echocardiographic and MRI evaluation of tricuspid valve and right ventricular function might identify patients at higher risk of developing postoperative RH failure.
LimitationsThis is a retrospective single-center study, with a long recruitment time and, therefore, the population might be not sufficiently representative. Obviously, the pathophysiology of TR with right ventricular impairment is a time-dependant and time-related aspect in which reversible patho-anatomical tissue changes in the right ventricle will slide into irreversible damage. Assessment of this pathophysiological process is preferably evaluated with sequential detailed echocardiography examinations. The clinical parameters (NYHA, RH failure, electrolyte abnormalities), as used in this study, are late signs and symptoms. Probably, the most appropriate follow-up after first diagnosis of severe functional TR in patients with concomitant left-valve disease will include specific sequential echocardiographic and MRI study protocols of tricuspid valve and right ventricular function. Both may help to identify markers related to higher risk of mortality, postoperative RH failure and decreased mid-term survival, advising early surgical treatment. In this study, patient follow-up was carried out in the mid-term; consequently, there are no clear conclusions about the influence of delayed surgery on long-term mortality.
CONCLUSIONSIn conclusion, our study shows that, in patients with severe TR and concomitant left-valve disease, triple valve surgery and worse preoperative functional class increases operative mortality. Longer latency between diagnosis of severe TR and surgery decreased mid-term survival, even after adequate surgical correction. We consider that, after the first diagnosis of severe TR, sequential echocardiographic and MRI studies, focused on right ventricular and tricuspid valve function, may help to determine the most appropriate timing of surgery.
FUNDINGNone.
AUTHORS’ CONTRIBUTIONSAll authors contributed to the acquisition, analysis, or interpretation of the data for the work and final approval of the version to be published. B. Segura and Y. Carrascal also contributed to the conception, design, drafting and critically revision of the work for important intellectual content.
CONFLICTS OF INTERESTNone declared.
- -
Delayed surgery of severe TR is associated with poor outcomes and decreased survival.
- -
Some authors suggest that avoiding surgical delay in severe TR might decrease operative mortality and the development of RH failure.
- -
However, the optimal timing of surgery remains controversial.
In patients with severe TR and concomitant left-valve disease:
- -
Triple valve surgery increases operative mortality.
- -
Delays in surgery associated decreased mid-term survival.
- -
After the first diagnosis of severe TR, sequential echocardiographic and MRI studies, focused on right ventricular and tricuspid valve function, may help to determine the most appropriate timing of surgery.
.
We would like to thank Manuel Carrasco Moraleja for statistical advice.