Keywords
INTRODUCTION
Heart failure (HF) is one of the most prevalent and fatal disorders, with one of the highest resource consumption rates in healthcare systems. In Spain, at least 2% of the population over 40 years old and between 6% and 10% of the population over 60 suffer from HF.1 It is the leading cause of hospitalization among those over 65 years old, with 74 000 hospitalizations per year. As such, it consumes between 1.8% and 3.1% of the healthcare budget.2,3 It is a progressive and fatal disorder for which prognosis is unsatisfactory, even with proper treatment. The mortality rate at 4 years is 50%, while the rate in people suffering from severe HF is about 1 year,4 similar to more aggressive cancer types.
To ascertain the severity of HF5 we usually examine the symptoms, limitations in physical activity6 and the structural changes produced in the heart.7
The optimal drug therapy (ODT) for HF has made use of multiple strategies which included and combined the following: ACE inhibitors or angiotensin-converting enzyme inhibitors, angiotensin II receptor antagonists, aldosterone antagonists, and beta-blockers. However, a large number of patients continued to suffer from a lower quality of life and have a high mortality rate. These are non-responder patients, who continued suffering despite receiving proper drug treatment.
Cardiac resynchronization therapy (CRT) is a technology that offers a new treatment option for patients with HF. As a mechanical device, it aims to improve the effectiveness of blood pumping by coordinating the various segments of the heart, which previously functioned without synchronization.8 The performance mechanism of CRT corrects the electromechanical asynchrony by acting on the atrioventricular, interventricular, intraventricular, and intramural delay. It therefore improves the haemodynamic parameters and the cardiac function without increasing oxygen consumption.9 It can be used together with an implantable cardioverterdefibrillator (CRT-ICD). It is estimated that between 20% and 30% of patients with symptomatic HF and 10% of unselected HF patients suffer from intraventricular conduction disorders, and these patients could benefit from CRT.10 At present, to reduce morbidity and mortality,5,7 CRT is recommended in clinical practice guidelines for the treatment of patients in functional class III and IV of the New York Heart Association (NYHA) who remain symptomatic despite ODT and have a decreased ejection fraction and prolonged QRS.
The continuing emergence of new healthcare technologies requires the assessment of additional benefits provided by these technologies in relation to the increasing healthcare expenditure involved.
In this context, this paper will carry out an economic evaluation of CRT by comparing it with ODT for the treatment of patients with HF in NYHA functional class III and IV, within the Spanish healthcare setting.
METHOD
A cost-benefit analysis was performed in patients with HF in NYHA functional class III and IV and with a decreased ejection fraction and prolonged QRS. The analysis included 4 treatment alternatives. The first consisted of CRT. The second included CRT without defibrillation capability, in addition to optimal drug therapy (CRT + ODT), and the third also incorporated defibrillation capability (CRT - ICD + ODT). Quality-adjusted life years (QALYs) were used as the main measure of effectiveness. The evaluation was developed from the perspective of the financial backer (National Healthcare System), and both the costs and effects that would occur in the future were discontinued at a rate of 3%.11
Baseline Characteristics of the HF Population
Four Spanish registers of patients with HF were used12-15 to determine the age characteristics of the reference population. Thus, based on 7939 patients included in the abovementioned records, our cohort was composed of 39.5% women and the mean age was 69.3 years.
Non-Cardiac Mortality
It is assumed that the value in this variable is not affected by the treatment received.
This variable was calculated with data on mortality by cause that were available from the Spanish National Statistics Institute, according to the International Statistical Classification of Diseases and Related Health Problems (ICD) 10 (http://www.ine.es/jaxi/tabla.do?path=/t15/p417/ a2007/l0/&file=01000.px&type=pcaxis&L=0) for 2007, adjusted by sex and age group.
Any mortality related to heart disease, codes I44 to I50 of the ICD-10, was deducted from the overall mortality variable for each age group and sex. The probability of dying from other causes, age and sex weighted, was calculated with these figures and those of the population, also by age and sex.
Effectiveness Data
Following the criteria of evidence-based medicine, a meta-analysis of previously published randomized clinical trials was used16,17 as the best source to determine the relative clinical effectiveness of the alternatives studied (Table 1). The relative risks among the various treatment options were obtained from the study of McAlister et al,17 which introduced an independent analysis for the subgroup of patients in functional class III and IV.
Utility values associated with the stages of the NYHA scale were obtained from measurements taken from 2709 patients from the Spanish INCA study.18
The patient cohort included in the model began in functional class III and IV. The temporal evolution of the functional class depended on the treatment followed. Therefore, the information of the clinical trial CARE-HF19,20 was used, since it was the study with the longest follow-up period that included Spanish patients. After 18 months, ie, the follow-up period of the abovementioned trial, we assumed that the patients remained in the functional class achieved.
Cost Data
Various sources were used to determine unit costs. Official sources were preferred, whenever possible, as they were considered less subject to bias. In this way, those procedures collected by diagnosis-related groups (DRGs) were taken from the Spanish Ministry of Health and Social Policy,21 as were the medicine prices that constitute the ODT costs.22 The prices for visits were obtained from the official prices of the Community of Madrid.23
Since the cost of CRT and CRT-ICD devices exceeded the cost of the procedure as reported by DRGs already be collected, we referred to the information submitted by the manufacturer. We used the average purchase price of the resynchronization devices in the public tenders in the first quarter of 2009. The cost of the surgery and hospital stay was added to the cost of the device, which was calculated using cost data taken from the cost accounting of the Community of Madrid.
The cost data were updated through the general index of consumer prices at constant 2009 prices, whenever necessary.
Analytical Model of Economic Evaluation
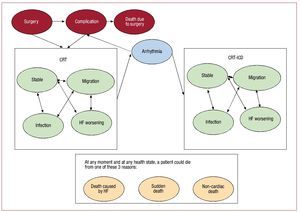
The economic evaluation was performed by adapting a previously published Markov model of the Spanish healthcare setting.16 The Markov models are representations of reality through a finite number of healthcare states, which must be comprehensive and exclusive, ie, each individual must match only one of those states. Events that may happen to each individual included in the model are modeled as steps or transitions between states, which occur at fixed-time intervals called "cycles." The likelihood that these steps occur between states is defined by the transition probabilities between states.24,25 For the patients on the CRT and CRT-ICD options, the model began with the surgery to implant the device. These patients could suffer complications leading to death or the complications were finally overcome. Subsequently, the patients went through one of the health states associated with the device implanted. These 4 states were as follows: stable, worsening of HF requiring hospitalization, local infection caused by the device, or migration of the electrode cable. In the case of the CRT device without a defibrillator and ODT, the patients, who suffered an arrhythmia that required hospitalization underwent surgery to install a CRT-ICD or an implantable cardioverter-defibrillator (ICD), respectively. At any moment, and from all health states considered, death could occur due to the following 3 reasons: worsening of HF, sudden death or other causes (Figure 1).
Figure 1. Model for the CRT alternative option. A patient with HF is implanted with the CRT. The surgery can involve complications and even death. With the device implanted, the patient may remain stable or suffer deterioration of the HF that requires hospitalization, device-related infection, or migration of the electrode cable. He may also suffer from arrhythmia that requires the updating of the CRT-ICD device. The patient can die from any of the abovementioned causes because of HF, sudden death or other causes.
The duration of the cycle in our model was 1 month, which we consider adequate to reflect the possible evolution of the disorder.
We performed a univariate sensitivity analysis on all the parameters of the model to confirm the ones that had a greater influence on the results obtained. The results of the sensitivity analysis are presented through tornado diagrams that show the degree to which the variation of the values of the different variables affects the model's results. The ranges of variation set for each variable were the confidence intervals estimated at 95%.
The model and the calculations were created using the Microsoft Excel 2003 application.
RESULTS
The results for the baseline case of our economic evaluation (Table 2), that is, a cohort of patients with an average age of 69 years and 3 months, made up of 39.5% women, were:
1. The patients treated with ODT had a discounted half-life of 3.86 years, 2.11 QALYs and the average cost of treatment was 11 722.
2. The patients treated with CRT + ODT lived for 4.71 years, 2.80 QALYs, with a cost of treatment of 31 629. Regarding the ODT, CRT improves discounted life expectancy in this group of patients by 0.85 years and 0.70 QALYs, with an incremental cost of approximately 20 000. This means that with this option each QALY year would cost 28 612, compared with treatment with ODT.
3. In patients treated with CRT-ICD + ODT, life expectancy was 5.36 years, 3.19 QALYs, with a cost of treatment of 52 593. These results entailed an improvement of 1.50 years of life in the prognosis of patients compared to ODT and 0.65 years in comparison to resynchronization without an associated defibrillator. The QALYs increased by 1.09 and 0.39 years, respectively. These improvements were achieved with an incremental cost of 40 870 for ODT and 20 964 for CRT without a defibrillator. Therefore, the incremental cost-effectiveness ratio (ICER) was 37 591 per QALY versus ODT and 53 547 per QALY versus CRT + ODT.
Sensitivity Analysis
The results obtained in our baseline case were sensitive to individual variations in the values of the key effectiveness parameters used in the model, depending on the alternative options compared.
If we compare CRT and ODT (Figure 2), we can see that the 2 most influential parameters on the end result were the relative risks of death from HF and sudden death with CRT versus ODT. In the lowest value of the confidence interval of 95%, these risks decreased the ICER approximately to 22 500 per QALY. By contrast, when placed in the highest value of the confidence interval, the ICER reached 45 000 and 47 000 per QALY, respectively. In addition, other parameters that would boost the result of our evaluation beyond the value of 30 000 per QALY are as follows: the likelihood of arrhythmia, the migration and infection of the device, the slope of the survival curve for sudden death and the discount rate.
Figure 2. CRT versus ODT sensitivity analysis. The tornado diagram shows how the individual variations of the parameters affect, within its limitations, the result of the incremental cost-effectiveness ratio (/QALY) calculated by our model.
If the comparison analyzed was for CRT-ICD versus CRT, the result, in terms of ICER, remained constant between 48 000 and 70 000 per QALY, as shown in Figure 3. The only parameter that moved the results outside this range was the relative risk of sudden death between the systems with CRT and those with ODT. The result, therefore, varied between 33 000 and 147 000 per QALY.
Figure 3. CRT-ICD versus CRT sensitivity analysis. The tornado diagram shows how the individual variations of the parameters affect, within its limitations, the result of the incremental cost-effectiveness ratio (/QALY) calculated by our model.
DISCUSSION
The economic evaluation of healthcare technologies aims to provide information during the decision-making process on the introduction of technologies within the healthcare service portfolio. It does not seek to replace the judgment of medical professionals who have made a decision for an individual patient.
We have developed an economic evaluation model that uses the meta-analysis of randomized controlled trials (RCTs) as a source of effectiveness, which is considered the highest level of scientific evidence. The results will be valid to the extent that similar results can be achieved in routine clinical practice.
The results of the economic evaluation made for our healthcare setting are within the range of previously published studies16,26-31 for other geographical areas.
The following limitations of our economic evaluation should be noted: first, it is a developing technology, thus it is expected that the results will be further improved as the technology evolves. By including data from the first published RCTs, we are possibly skewing the results of our evaluation against CRT. Secondly, by including only randomized studies, it is possible that the results are more favorable for surgery than those achieved in the routine clinical practice.
Our model is based on published studies, the majority of which have a short follow-up period. It seems clear that the longer the follow-up period, the greater the incremental effect achieved with CRT.32 In fact, only one study has an average follow-up period of over 2 years (CARE HF),26,27 which would mean that the benefits of CRT were under-considered.
The results obtained by visual analog scale were used as quality-of-life scores, although it would have been desirable to use those obtained from the EQ-5D questionnaire. Nevertheless, they constitute the scores available in a sufficiently representative sample of Spanish patients with HF.18
It should be noted that two systematic reviews were used to determine the clinical effectiveness of CRT.16,17 The review by McAlister et al17 performed an analysis of a subgroup of patients in NYHA functional class III and IV, which is currently indicated for recourse to this procedure. We used this analysis in our evaluation to estimate the effectiveness of CRT. The sense in which this decision affects the results of our evaluation is unclear, since on the one hand the effect of CRT will be greater when this group of selected patients is independently analyzed. On the other hand, it will mean that, except for ODT, the control group includes other treatments.
The cost data were obtained from various official sources, whenever possible. The Spanish Ministry of Health publishes both the hospital procedures of the DRGs21 and the medicines on the Name Index.22 Concerning visits, we used information published by the Community of Madrid23 in the Official Gazette, since such information is unavailable at a national level. All these sources can be considered highly representative of our scenario, although using different sources may affect the calculation methodology. The price of resynchronization devices, and therefore of related procedures, was the only datum that could not be obtained from any official source. The DRG procedures published by the Ministry, which would include the implant procedure for resynchronization systems, has a lower cost than the CRT-ICD generator. We therefore decided to calculate the costs incurred by these procedures from the information on the price for the award of public tenders in the first quarter of 2009, which was compiled by the consultancy EUCOMED for the Spanish industry. We added a price for the cost of the surgery and hospital stay in these prices, which was obtained from the analytical accounts of the Community of Madrid.
The life expectancy of patients who were implanted with the device affects the effectiveness of the device, since the greater the effectiveness is, the longer the patients will benefit from an improvement in their quality of life, and the greater the prevention of a number of events requiring hospitalization for HF. It may therefore be a factor to consider when deciding on the implant. The price of the device is a factor that greatly affects the effectiveness of the technology. If, as it appears from the technology diffusion curve, the price decreases with time, together with the actual progress and continuous improvement in the devices, it will lead to an improvement in the effectiveness of the technology.
The use of CRT-ICD features better clinical effectiveness in terms of survival and a QALY of approximately 1.5 times that achieved with CRT without a defibrillator. However, the cost increase is more than 2 times that of CRT without a defibrillator. Future research should focus on identifying the group of patients that may obtain a greater benefit from the addition of the defibrillator to the cardiac resynchronization therapy.
CONCLUSIONS
Our economic evaluation indicates that cardiac resynchronization therapy can be an effective treatment option for patients with HF and NYHA functional class III and IV, compared to the ODT option. CRT achieves a significant improvement in the median survival rate and in the QALYs. It achieves this effectiveness through an increase in the cost of just under 30 000 per QALY, which is acceptable for Spanish healthcare technologies,33 even though the result is influenced by the existing uncertainty in many parameters of the model that place the comparative effectiveness of the technology over the abovementioned limit.
CRT-ICD also achieves an improvement in the expected survival rate and in the expected QALYs, when compared to CRT without an associated defibrillator. However, this increase in effectiveness is achieved with an increase in the cost of about 60 000 per QALY. This discourages its widespread use for the patients who are the subject of our evaluation, requiring the correct selection of patients for the joint use of resynchronization and defibrillator. Further research should be undertaken to try to clarify the abovementioned group of patients.
ACKNOWLEDGMENTS
To Rodolfo Hernandez and Sergio Maeso, for their useful comments that have helped to improve the quality of this article. To Beatrice Rivas (AstraZeneca) for providing us, in a disaggregated way according to the stages of the NYHA scale, with the benefits obtained from a Spanish population and to Sonia Campos (Biotronik) for providing us with the cost data of the devices used.
ABBREVIATIONS
CRT: cardiac resynchronization therapy
CRT-ICD: cardiac resynchronization therapy with implantable cardioverter defibrillator
HF: heart failure
ICD: implantable cardioverter defibrillator
ICER: incremental cost-effectiveness ratio
NYHA: New York Heart Association
ODT: optimal drug therapy
SEE ARTICLE ON PAGES 1230-1
Project partially financed by the Quality Plan for the National Healthcare System - Spanish Ministry of Health and Social Policy.
Correspondence: Sr. D. Callejo Velasco.
Gran Vía, 27, 7.ª Planta. 28013 Madrid. Spain
E-mail: daniel.callejo@salud.madrid.org
Received February 3, 2010.
Accepted for publication May 24, 2010.