There are few data on emergency visits after cryoballoon-based pulmonary vein isolation. The aim of this study was to quantify emergency department visits during the first 3 months after the procedure and to identify the reasons for consultation, final diagnoses, and the therapeutic approach.
MethodsObservational, retrospective study of 330 consecutive patients undergoing a first cryoballoon-based ablation procedure. Patients were followed up for 90 days after the procedure. We recorded emergency visits, symptoms, electrocardiographic data, and the therapeutic approach. Final diagnoses were classified as rhythm disorder, confirmed complication, possible complication, and unrelated to the procedure or to the arrhythmic disorder.
ResultsA total of 112 (34%) patients attended the emergency department, 50 (44.6%) for palpitations. Sustained atrial arrhythmias were documented in 44 (39.3%) patients. Among the 29 (25.9%) visits for complications potentially related to the procedure, 5 were confirmed inguinal puncture complications and 10 were classified as unconfirmed possible complications. Forty-one visits were unrelated to the procedure or to the arrhythmic disorder. A total of 21.4% of the visits were due to palpitations requiring no therapeutic action.
ConclusionsA third of the patients attended the emergency department at least once, with the most frequent reason being arrhythmia-related symptoms. Late complications were rare and generally mild. Up to 20% of emergency visits could potentially be avoided by the availability of a teleconsulting system with remote electrocardiogram transmission.
Keywords
Cryoballoon-based pulmonary vein isolation (PVI) is a safe and reasonably effective treatment for atrial fibrillation (AF).1,2 Although AF ablation reduces emergency department visits in the mid-term,3 such visits may be increased in the first postprocedural weeks for various reasons. In addition, the rate of major procedural complications ranges between 2% and 7.5%,4,5 and some may be delayed, such as groin vascular complications,6 embolic stroke,7 pericardial tamponade,8 persistent gastric motility disorders,9 and atrioesophageal fistulas.10 Moreover, patients are frequently advised of the value of an immediate electrocardiogram (ECG) if they experience palpitations or chest pain in the first postprocedural days to document possible arrhythmic recurrence, and this technique can often only be performed in the emergency department for logistical reasons. However, there are few data in the literature on emergency department visits and their reasons among patients who have undergone cryoballoon-based PVI for AF treatment. Thus, the aim of this study was to quantify emergency department visits in the first 90 days after an AF ablation procedure, determining the reasons for the consultation, the final diagnosis, the therapeutic approach, and the hospitalization rate, and to estimate the percentage of visits potentially avoided through the use of a remote ECG monitoring system.
METHODSThis observational and retrospective study investigated patients who underwent their first AF ablation procedure with cryoballoon-based PVI in a regional tertiary referral center for this technique between 2012 and 2018. Due to the retrospective use of anonymized data without the need for patient interaction, approval was not required from the ethics committee of the center. The procedure indications during the study years were generally in line with clinical practice guidelines, with a predominance of patients with paroxysmal AF (understood as an absence of events lasting > 7 days) and a normal heart, without severe atrial dilatation.
The procedural protocol of our center includes a previous transesophageal echocardiogram to rule out atrial thrombosis. Anticoagulation is managed to maintain a periprocedural international normalized ratio (INR) of about 2.0 to 2.5 if the patient is taking a vitamin K antagonist; if the patient is taking direct oral anticoagulants, these drugs are withdrawn. The procedure was generally performed with spontaneous breathing and with propofol and remifentanil sedation. Two femoral punctures were performed in the same vein for a multipurpose tetrapolar or decapolar diagnostic catheter and a cryoballoon introducer. A transseptal puncture was performed under ultrasound guidance in the first 110 patients and under fluoroscopic guidance using a guidewire specifically designed for transseptal puncture (SafeSept, Pressure Products, San Pedro, California, United States) in the remainder. The vast majority of procedures (from June 2012 onward) were performed using a second-generation cryoballoon (Medtronic Advance) for PVI, without additional procedures except for cavotricuspid isthmus (CTI) ablation in selected patients. The standard cryoenergy dosage comprised a 4-minute application (3 if electrical isolation of the pulmonary veins was evident in the first 60seconds) and an additional application if the isolation was delayed or the minimum temperature reached > −40°C. Patients were usually discharged 48hours after the procedure if no complications occurred. Among the general recommendations at discharge, the patients were advised to visit their closest emergency department to undergo an ECG if potentially arrhythmic symptoms developed or those related to the ablation procedure, as well as to follow the indications of the treating physician. The antiarrhythmic drug prescription at discharge for the first postprocedural months was tailored to each patient.
The mid-term results of our group were similar to those described in the literature, with 73% of patients recurrence-free at 1 year without antiarrhythmic drugs. The demographic and clinical data were obtained from the patients’ medical records for the admission when the procedure was performed. Specifically, the information recorded in these medical records was used to identify the diagnoses of hypertension, diabetes mellitus, structural heart disease, and AF type. Left atrial size was classified according to the recommendations of the international echocardiography societies.11 The regional electronic medical record system implemented in the autonomous community was used to obtain follow-up data. This system records visits to the hospital emergency departments of the entire health care area, with corresponding reports on hospital admission or discharge as appropriate. Specifically, all emergency department visits during the first 90 days after the procedure were reviewed and the numbers of visits per patient were recorded. When there were repeated visits, the most relevant analysis was included (the first if all visits were for similar reasons, the first to show the presence of arrhythmia recurrence if there were various visits for potentially arrhythmic symptoms, or the first possibly related to the procedure if there were other visits for unrelated reasons).
The symptoms prompting the visit were recorded, as well as the electrocardiographic rhythm, if analyzed. The following symptoms were considered potentially arrhythmic in origin: palpitations, chest pain, dyspnea or exhaustion, and dizziness/syncope. In addition, the electrocardiographic documentation of sustained atrial tachyarrhythmia (SAT) was checked, namely, AF, flutter, or atrial tachycardia. Symptoms considered potentially related to procedural complications comprised chest pain, dyspnea, digestive discomfort, neurological abnormalities, discomfort related to the groin puncture site, and fever or other symptoms indicative of infection (in the case of the latter, if they occurred in the first 7 postprocedural days). Based on the final diagnosis, the reason for the emergency department visit was classified into 1 of 4 groups: a) rhythm disorder, documented by ECG or not; b) confirmed procedural complication; c) possible procedural complication; and d) unrelated to the procedure or the patient's arrhythmia disorder. Finally, the patients’ destination was recorded (discharge to home or admission) and the therapeutic approach during the emergency department visit due to the rhythm disorder.
Regarding the statistical analysis, quantitative variables are presented as mean±standard deviation and qualitative variables as percentages. For the comparison of means, the Student t test was used for independent data, expressed as the mean difference (95% confidence interval [95%CI]). The relationship between qualitative variables was analyzed with the chi-square test or Fisher exact test, and the relative risk is expressed as a ratio (95%CI). A multivariate logistic regression analysis was performed with the forward conditional method to evaluate the statistical independence of the clinical and demographic variables with predictive value for emergency department visit in the univariate analysis using IBM-SPSS Statistics version 20. Repeated-events survival analysis was also performed for visits prompted by rhythm disorders using the proportional measures method implemented in the PHREG procedure of SAS 9.4/STAT 13.1 software.
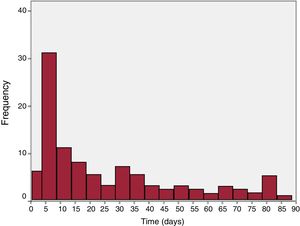
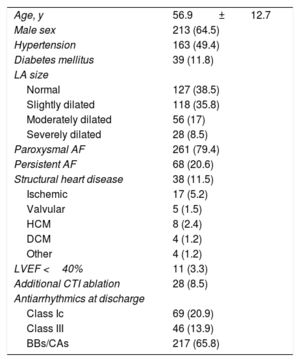
RESULTSThe analysis included 330 patients. The population characteristics are summarized in table 1. Acute success, defined as electrical disconnection of all pulmonary veins, was achieved in 316 patients (95.8%). Only 3 relevant acute procedural complications recorded during the hospital admission were related to the vascular access: 1 soft-tissue hematoma conservatively treated with compression and 2 cases of femoral artery pseudoaneurysm that required endovascular treatment via endoprosthesis implantation. In the 90 days after the procedure, 112 patients (34%) made at least 1 visit to the emergency department; of these, 41 made more than 1 visit (30 patients made 2 visits, 7 patients made 3; 3 patients made 4; and 1 patient made 5). Of the 41 patients with repeat visits, 24 always consulted for the same reason and the first of these visits was included in the analysis. Six patients were suspected to have had a previously undocumented recurrence that was noted in a subsequent visit, in which case the analysis included the first visit to document the arrhythmia. Finally, 11 patients made a visit due to suspected and/or documented recurrence at one time and for reasons not related to the procedure or the arrhythmia disorder at another time; the first visit with documented recurrence was included in the analysis (or the suspected recurrence if recurrence could not be documented in any visit). Attendance according to time after the procedure is shown in figure 1; a well-defined peak was evident between days 3 and 8. Men attended the emergency department less frequently than women (relative risk=0.69; 95%CI, 0.52-0.93). Patients who visited the emergency department also tended to be older (mean age, 59±13 years vs 56±12 years for patients without an emergency department visit; mean difference, 2.8 [–0.1 to 5.7] years), although only sex remained an independent predictor on multivariate analysis. The remaining clinical variables had no significant influence on attendance. Additional CTI ablation was also no longer associated with emergency department visits (35.7% of patients with CTI ablation vs 34% of the remainder; P=.8), the reason for the consultation, or postprocedural complications.
Baseline characteristics of the study population (n=330)
| Age, y | 56.9±12.7 |
| Male sex | 213 (64.5) |
| Hypertension | 163 (49.4) |
| Diabetes mellitus | 39 (11.8) |
| LA size | |
| Normal | 127 (38.5) |
| Slightly dilated | 118 (35.8) |
| Moderately dilated | 56 (17) |
| Severely dilated | 28 (8.5) |
| Paroxysmal AF | 261 (79.4) |
| Persistent AF | 68 (20.6) |
| Structural heart disease | 38 (11.5) |
| Ischemic | 17 (5.2) |
| Valvular | 5 (1.5) |
| HCM | 8 (2.4) |
| DCM | 4 (1.2) |
| Other | 4 (1.2) |
| LVEF <40% | 11 (3.3) |
| Additional CTI ablation | 28 (8.5) |
| Antiarrhythmics at discharge | |
| Class Ic | 69 (20.9) |
| Class III | 46 (13.9) |
| BBs/CAs | 217 (65.8) |
AF, atrial fibrillation; BBs, beta-blockers; CAs, calcium antagonists; CTI, cavotricuspid isthmus; DCM, dilated cardiomyopathy; HCM, hypertrophic cardiomyopathy; LA, left atrium; LVEF, left ventricular ejection fraction.
Values represent No. (%) or mean±standard deviation.
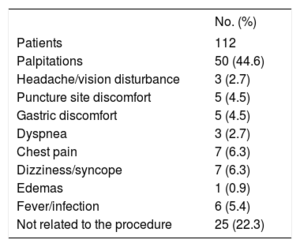
The symptoms prompting the consultation are shown in table 2. In total, 67 patients (59.8%) attended for potentially arrhythmia-related symptoms, mainly palpitations. SAT was documented in 44 patients (65.7%): AF in 34 and flutter/atrial tachycardia in 10. Specifically, SAT was documented in 39 of the 50 patients who visited due to palpitations (78%), in 3 of the 7 who visited due to chest pain, and in 1 of the 3 who visited due to dyspnea. Of the 112 visits, 29 (25.9%) were due to symptoms potentially related to procedural complications.
Symptoms prompting the visit
| No. (%) | |
|---|---|
| Patients | 112 |
| Palpitations | 50 (44.6) |
| Headache/vision disturbance | 3 (2.7) |
| Puncture site discomfort | 5 (4.5) |
| Gastric discomfort | 5 (4.5) |
| Dyspnea | 3 (2.7) |
| Chest pain | 7 (6.3) |
| Dizziness/syncope | 7 (6.3) |
| Edemas | 1 (0.9) |
| Fever/infection | 6 (5.4) |
| Not related to the procedure | 25 (22.3) |
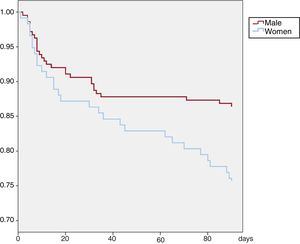
According to the final diagnosis, the reason for the visit was classified as a rhythm disorder in 56 patients (50%), as a confirmed procedural complication in 5 (4.5%), as a possible complication in 10 (8.9%), and as unrelated to the procedure or the patients’ arrhythmia disorder in 41 (36.6%). For visits due to rhythm disorders, a more detailed analysis was performed of repeated-events survival, including age, sex, AF type, and additional CTI ablation as potentially predictive variables. Again, sex was the only variable with independent predictive value: women visited with higher frequency (relative risk=2.04; P=.01). The event-free survival curve of visits for this reason stratified by sex is shown in figure 2. Regarding the symptoms potentially related to procedural complications, only visits due to discomfort related to the groin puncture were considered confirmed complications. Possible complications in the first week after the ablation included 3 visits due to headache and blurry vision, 2 visits due to chest pain with pericarditis characteristics, 3 visits due to abdominal pain/distension, and 2 visits due to dyspnea of unknown origin. In the subsequent follow-up of these patients, a definitive diagnosis was not obtained and the symptoms spontaneously resolved or were managed with symptomatic treatment. In the other visits, the final diagnosis was not related to the patients’ arrhythmic disorder or the ablation procedure. Curiously, these visits that were not related to the procedure also showed an incidence peak in the first 2 weeks after discharge and stabilized thereafter. Among the 44 patients with emergency department-documented SAT, 13 (29.5%) were treated with electrical cardioversion, 12 (27.3%) with pharmacological cardioversion, and 6 (13.6%) with pharmacological heart rate control; 13 (29.5%) received no specific treatment. Thus, of the 50 patients who visited due to palpitations, SAT was not documented in 11 and treatment was not considered necessary in 13. These 24 patients represented 21.4% of all first emergency department visits, and the outcome of these visits was, in the best-case scenario, the simple documentation of electrocardiographic rhythm. It is reasonable to believe that, at least in most of these patients, their visit could have been avoided if they had been equipped with a telemonitoring system with integrated remote ECG transmission. In total, 13 patients (3.9%) required hospital admission: for arrhythmia recurrence control (n=6), due to heart failure (n=1), due to pericarditis (n=1), or for reasons unrelated to the procedure or the patients’ index condition (n=5).
DISCUSSIONThe main findings of this study are that about one third of patients who undergo cryoballoon-related AF ablation visited the emergency department during the next 3 months, half due to potentially arrhythmic symptoms, with the arrhythmia underlying the symptoms documented in most patients. Late procedural complications were rare and generally associated with the venous puncture. Visits due to palpitations that were not specifically treated in the emergency department represented about 20% of the total.
There is little information in the literature on emergency department visits after pulmonary vein ablation, and we know of no such study that has specifically focused on the cryoballoon technique. In a recently published American registry,12 28.8% of patients visited the emergency department in the first 30 days after the AF ablation procedure, a higher percentage than that obtained in this study for that period (22%). The main reason for the visit was arrhythmia recurrence (76.8% vs 50.5% of the patients of our series), and female sex was a significant predictor of an emergency department visit in the first month or of procedural complications, which is also in line with our data. The observed 30-day hospitalization percentage was 9.7%, similar to that described in another study based on national registry data on hospitalizations in the United States,13 with readmission rates of 10.9% and 16.5% at 1 and 3 months, respectively. These rates greatly exceed those obtained in our study. This discrepancy can probably be explained by the major differences between the 2 health care systems and between the patients’ treatment protocols.
The main reason for hospitalization in the series by Freeman12 was control of arrhythmia recurrence (42% of patients), which is very similar to the 46% of our series. There were no readmissions due to embolic events or delayed tamponades secondary to perforation, an aspect confirmed by our results. Instead, 2% of admissions were reported to be due to puncture complications. In Spain, patients with these complications are usually diverted to vascular radiology for outpatient treatment within 24 to 48hours, thereby avoiding hospitalization. With these data, it seems reasonable to assume that emergency department visits due to significant procedural complications that are not puncture-related are highly infrequent.
Also of interest is the subgroup of patients who visited the emergency department due to symptoms compatible with arrhythmia recurrence and who, after electrocardiographic documentation of rhythm, were discharged with no specific treatment. In some of these patients, which represented about 20% of visits, the emergency department visit could have been avoided the availability of a telemonitoring system with remote ECG transmission. In this regard, post-AF ablation follow-up can involve software applications for patient-reported outcomes that allow the automated collection of information on quality of life and symptom parameters during follow-up.14 The addition of one or various ECG leads to these devices for remote ECG transmission—using, for example, a smartphone—could significantly reduce emergency department visits during the first few weeks after the procedure, as indicated by our results. Controlled and randomized studies should be performed to confirm this hypothesis.
LimitationsFirst, the study data were obtained from the regional electronic medical records of the public health system, which is why we have not included visits made in other regions or to private hospitals not included in the system. This situation is nonetheless probably rare in our country. Moreover, no analysis was performed of emergency department visits to health centers outside the hospital system, whose details are not recorded in the electronic medical records. Both circumstances could lead to an underestimation of the number of emergency department visits. In addition, the data analyzed are based on emergency department and hospital discharge reports; accordingly, the electrocardiographic interpretation, final diagnosis, therapeutic approach in the emergency department, and the indication for hospital admission depend on the judgment of the patients’ treating physician, who might not be an expert in this disorder. The evaluation to determine if the reason for the visit was related to the procedure was also not performed in a blinded manner, which could generate bias. Finally, specific factors associated with the regional health care system may have somehow influenced the flow of patients with specific symptoms or diseases, which would modify some results from other health care systems or areas, and it is difficult to evaluate the impact of this factor due to the absence of similar studies in other regions.
CONCLUSIONSOur results confirm that approximately one third of patients who undergo a cryoballoon procedure for AF management visit an emergency department in the first few weeks after the procedure. Palpitations were the most frequent reason for consultation, and rhythm disorders prompting the visit could be documented in 80% of the patients. Late procedural complications were rare and mainly associated with venous puncture. The availability of a remote ECG transmission system could have avoided a significant number of emergency department visits because almost half of patients who visited due to palpitations were not administered specific treatment.
CONFLICTS OF INTERESTThe authors’ institution has received educational and research assistance from Medtronic. P. Peñafiel Verdú has received personal payments from Medtronic unrelated to the present study.
- –
Cryoballoon-related pulmonary vein isolation (PVI) is a safe and reasonably effective treatment for AF.
- –
AF ablation reduces emergency department visits in the mid-term, although visits can be increased in the first postprocedural weeks for various reasons.
- –
Late complications of AF cryoballoon ablation procedures prompting emergency department visits are rare and generally related to venous puncture.
- –
Almost half of patients who visited the emergency department due to postprocedural arrhythmic symptoms were administered no specific treatment.
- –
The availability of a telemonitoring system with remote ECG transmission could avoid a significant number of emergency department visits.