Endomyocardial biopsy (EMB) is the only technique able to establish an etiological diagnosis of myocarditis or inflammatory cardiomyopathy (ICM). The aim of this study was to analyze the clinical profile, outcomes, and prognostic factors of patients with suspected myocarditis/ICM undergoing EMB.
MethodsWe retrospectively analyzed the clinical characteristics, histological findings, and follow-up data of all patients with suspected myocarditis or ICM who underwent EMB between 1997 and 2019 in a Spanish tertiary hospital. The diagnostic yield was compared using the Dallas criteria vs immunohistochemical criteria (IHC).
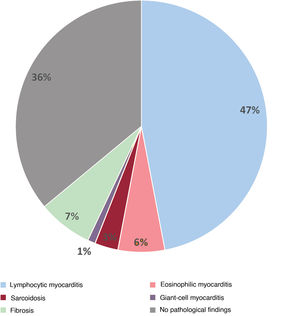
ResultsA total of 99 patients underwent EMB (67% male; mean age, 42±15 years; mean left ventricular ejection fraction [LVEF], 34%±14%). Myocarditis or ICM was confirmed in 28% with application of the Dallas criteria and in 54% with the IHC criteria (P <.01). Lymphocytic myocarditis was diagnosed in 47 patients, eosinophilic myocarditis in 6, sarcoidosis in 3, and giant cell myocarditis in 1 patient. After a median follow-up of 18 months, 23 patients (23%) required heart transplant (HTx), a left ventricular assist device (LVAD), and/or died. Among the patients with IHC-confirmed myocarditis, 21% required HTx/LVAD or died vs 7% of those without inflammation (P=.056). The factors associated with a worse prognosis were baseline LVEF ≤ 30%, left ventricular end-diastolic diameter ≥ 60mm, and NYHA III-IV, especially in the presence of inflammation.
ConclusionsEMB allows an etiological diagnosis in more than half of patients with suspected myocarditis/ICM when IHC techniques are used. IHC-confirmed inflammation adds prognostic value and helps to identify patients with a higher probability of developing complications.
Keywords
Myocarditis is defined as inflammation of the heart muscle and is estimated to be involved in 0.5-4% of hospital admissions for heart failure (HF).1 When the inflammatory features are associated with systolic ventricular dysfunction, it is termed inflammatory cardiomyopathy (ICM).2,3 Both myocarditis and ICM can be due to multiple etiologies, including infection and autoimmune or toxic processes.4 In clinical practice, the 2 conditions are distinguished according to the duration of symptoms, differentiating between acute myocarditis, where the history is generally <1 month, and chronic myocardial inflammation, where the history is longer and accompanied by ventricular dilatation or dysfunciton.5 Myocarditis and ICM can also be classified according to the inflammatory infiltrate on cardiac histology, as lymphocytic, eosinophilic, granulomatous (sarcoidosis being the most common) or giant cell.5
In recent years, advances in imaging techniques have improved the noninvasive diagnosis of myocarditis and ICM, mainly due to cardiac magnetic resonance (CMR).6 However, currently, endomyocardial biopsy (EMB) is the only technique that can confirm inflammation and establish the precise etiology, allowing individualized treatment to be started in certain cases.7 Although the sensitivity of EMB is relatively low when only histological criteria (Dallas criteria) are used, it has been suggested that this may be improved by increasing the number of samples or using immunohistochemical (IHC) criteria.8
Our aim was to study the clinical characteristics, histological findings, and outcomes in a series of patients with suspected myocarditis or ICM who underwent EMB and to evaluate the prognostic role of the presence of inflammation.
METHODSStudy populationWe retrospectively identified all patients who had undergone EMB (of right ventricle [RV], left ventricle [LV], or both) for suspected myocarditis or ICM between 1997 and 2019 in Clínica Puerta de Hierro and Hospital Universitario Puerta de Hierro-Majadahonda in Madrid. Patients were selected according to the American Heart Association indications for EMB9: a) new onset unexplained HF of less than 2 weeks’ duration along with hemodynamic compromise (class I indication); b) HF of 2 weeks’ to 3 months’ duration, with LV dilatation and advanced conduction defects, ventricular arrhythmias, or refractoriness to pharmacological treatment (class I indication); c) LV dilatation together with eosinophilia (IIa indication); and d) LV dilatation with advanced conduction disorders, ventricular arrhythmias, or refractoriness to pharmacological treatment of more than 3 months’ duration (IIa indication). The study was approved by the hospital's research ethics committee.
Clinical characteristicsData on each patient were obtained retrospectively through a review of clinical records. The baseline characteristics were obtained from the first assessment and follow-up data. Electrocardiographic and echocardiographic data prior to EMB were collected, as well as the most recent electrocardiogram and echocardiogram performed in patients who survived >3 months after EMB. CMR was also performed in some patients in the cohort, applying the classic Lake Louise diagnostic criteria.10 The date of EMB was used as the start of follow-up.
In patients who received a heart transplant (HTx), the most recent echocardiogram before the transplant was collected. We analyzed clinical events during follow-up such as serious ventricular arrhythmias (sustained ventricular tachyarrhythmia and ventricular fibrillation), ventricular assist device placement, HTx, or death from any cause.
Complications of EMB were also collected and classified, with major complications being perforation with cardiac tamponade, sustained ventricular arrhythmia with hemodynamic instability, complete atrioventricular block requiring a pacemaker, stroke, acute myocardial infarction, and the onset of severe valvular regurgitation.
Pathological analysis of endomyocardial biopsiesThe histological diagnosis of myocarditis/ICM was established using the Dallas criteria (myocardial necrosis and inflammation) or IHC criteria (≥ 14 leucocytes/mm2 with CD3+ T lymphocytes ≥ 7/mm2).3 All the histological samples underwent centralized analysis by the same pathologist with extensive experience in the study of EMB using both criteria. The samples that did not undergo IHC evaluation when they were taken (period 1997-2019) were re-analyzed using IHC for this study. Sarcoidosis was diagnosed by the presence of noncaseating granulomas; eosinophilic myocarditis, based on eosinophilic infiltrate on EMB with or without associated peripheral eosinophilia; and giant-cell myocarditis, by the presence of multinucleated giant cells with no associated granulomas, in accordance with accepted definitions.5
Statistical analysisThe statistical analysis was performed using the statistical package SPSS 21 (SPSS Inc., USA). Qualitative variables are presented as percentages, and continuous variables as mean±standard deviation. The chi-square test was used to compare qualitative variables, the Student t test was used to compare means in independent samples and the Kaplan-Meier test was used for survival curves. P values < .05 were considered significant.
RESULTSA total of 99 patients underwent EMB for suspected myocarditis or ICM during the study period. In 67% of the patients the EMB was taken from the RV; in 29%, from the LV; and in 4%, from both. A mean 3±2 samples were taken in each procedure.
Sixty-seven percent were men, with a mean age of 42±15 years. Baseline left ventricular ejection fraction (LVEF) was 32±14% and the indication for EMB was acute myocarditis with hemodynamic instability or ventricular arrhythmia in 33% of the patients (33/99) and dilated cardiomyopathy with subacute (between 2 weeks’ and 3 months’ duration) or chronic (more than 3 months) HF in the other 67% (66/99).
Diagnostic yield and therapeutic approachOn application of the Dallas histological criteria, 29 of 99 patients (29%) met the criteria for myocardial inflammation. Sensitivity was 42% (14/33 patients) in cases of acute myocarditis and was 23% (15/66 patients) in cases of subacute or chronic DCM with HF. After application of the IHC criteria, 24 additional patients met the criteria for myocardial inflammation and only 3 of the cases of eosinophilic myocarditis were Dallas-positive but IHC-negative, as the IHC criteria use total leucocytes and CD3+. In total, 54% (54/99 patients) met the IHC criteria for myocardial inflammation.
Using IHC criteria gave a higher percentage of cases of myocarditis/ICM on EMB in subacute and chronic cases than using the Dallas criteria, increasing from 23% to 52% of cases diagnosed (15/66 vs 34/66; P <.001). In the cases of acute myocarditis, biopsies were deemed positive according to the Dallas criteria and IHC criteria in 42% and 58%, respectively (14/33 vs 19/33; P=.04).
No significant differences were observed in the baseline clinical characteristics between patients with and without EMB-confirmed inflammation, except for a higher percentage of men and higher use of beta-blockers in patients without inflammation and younger age in patients with inflammation (table 1).
Baseline characteristics of patients with/without endomyocardial biopsy-confirmed inflammation
| Total (n=99) | Histologically-confirmed inflammationa (n=57) | No confirmed inflammation (n=42) | P | |
|---|---|---|---|---|
| Men | 66 (67) | 33 (58) | 33 (79) | .03 |
| Age, y | 42±15 | 39±14 | 46±16 | .016 |
| HTN | 20 (20) | 11 (20) | 9 (21) | NS |
| Diabetes mellitus | 13 (13) | 7 (13) | 6 (14) | NS |
| Hyperlipidemia | 21 (21) | 12 (21) | 9 (21) | NS |
| Acute presentation | 33 (33) | 22 (67)b | 11 (33) | NS |
| Cardiogenic shock | 27 (82) | 19 (70) | 8 (30) | |
| Ventricular arrhythmia | 2 (6) | 0 | 2 (100) | |
| Acute myocarditis + eosinophilia | 2 (6) | 2 (100)c | 0 | |
| Recurrent acute myocarditis | 2 (6) | 1 (50) | 1 (50) | |
| Subacute/chronic presentation | 66 (67) | 35 (53) | 31 (47) | NS |
| DCM 2 wks-3 mo | 17 (25) | 9 (53)d | 8 (47) | |
| DCM> 3 mo | 49 (75) | 26 (53)e | 23 (47) | |
| Autoimmune disease | 12 (12) | 7 (13) | 5 (12) | NS |
| NYHA functional class | ||||
| I | 22 (23) | 11 (19) | 11 (26) | .1 |
| II | 22 (23) | 10 (18) | 12 (29) | |
| III | 27 (27) | 15 (26) | 12 (29) | |
| IV | 28 (29) | 21 (37) | 7 (17) | |
| Atrial fibrillation | 18 (18) | 12 (22) | 6 (13) | NS |
| LVEF,% | 32±14 | 31±15 | 34±13 | NS |
| LVEDD, mm | 57±12 | 56±14 | 58±11 | NS |
| Treatment at follow-up | ||||
| Beta-blockers | 79 (80) | 41 (72) | 38 (90) | .046 |
| ACEI/ARB-II/ARNI | 84 (85) | 46 (80) | 38 (90) | NS |
| Aldosterone inhibitor | 55 (56) | 29 (51) | 26 (62) | NS |
ACEI, angiotensin converting enzyme inhibitors; ARB-II, angiotensin II receptor blockers; ARNI, angiotensin receptor-neprilysin inhibitor; DCM, dilated cardiomyopathy; HTN, hypertension; LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; NS, not significant; NYHA, New York Heart Association.
Cases of lymphocytic myocarditis confirmed using Dallas or immunohistochemical criteria, eosinophilic myocarditis, giant-cell myocarditis or sarcoidosis.
One case of eosinophilic myocarditis, 1 case of giant-cell myocarditis and 1 of sarcoidosis included in this subgroup of presentation with cardiogenic shock.
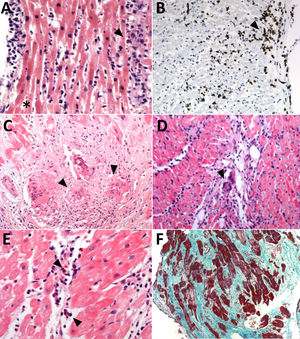
Regarding specific diagnoses, 47 patients had lymphocytic infiltrates compatible with lymphocytic myocarditis/ICM: 47% of them (22) had Dallas and IHC criteria, and the remaining 53% (25%) had IHC criteria only as there was no necrosis. An additional 10 patients were diagnosed with specific types of inflammation: 6 with eosinophilic myocarditis, 3 with sarcoidosis, and 1 with giant-cell myocarditis (figures 1 and 2). All the patients with eosinophilic myocarditis, sarcoidosis, and giant-cell myocarditis (10% of the patients from the cohort and 18% of the total with myocarditis/ICM) received immunosuppressive treatment. Among the 47 patients with a histological diagnosis of lymphocytic myocarditis/ICM, 21% (10) received immunosuppressive treatment: 12% in acute forms (2/17) and 27% in chronic forms (8/30).
Endomyocardial biopsies with different pathological diagnoses. A: H-E (× 200); lymphocytic myocarditis with positive Dallas criteria; lymphocytic infiltrate (arrow) and necrosis with rupture of myocardial fibers (asterisk). B: lymphocytic myocarditis with positive immunohistochemical criteria; the brown inclusions correspond to CD3+ lymphocytes (arrow). C: H-E (×200); cardiac sarcoidosis with presence of granulomas (arrow). D: H-E (×200); giant-cell myocarditis (arrow). E: H-E (× 400); eosinophilic myocarditis (arrow indicates eosinophils). F: Masson's trichrome (× 100); dilated cardiomyopathy, with extensive fibrosis. H-E, hematoxylin-eosin.
In the remaining 42 patients, a definitive histological diagnosis was not reached (42/99, 42%): isolated fibrosis was found in 6 patients (14%) and nonpathological findings in the others. However, one of the patients with evidence of fibrosis had a positive polymerase chain reaction (PCR) for enterovirus, which was treated with interferon beta. Among the 38 patients of the cohort whose viral PCR was performed on their EMB, parvovirus B19 and Epstein-Barr virus were positive in 3 patients (8%) each, followed by the enterovirus described (1 [3%]), and human herpes virus 6 (1 [3%]).
A total of 33 patients had had an MR in the same month as the EMB. Of them, 18 (55%) were diagnosed with myocarditis using IHC criteria for EMB, but only 6 met the Lake Louise criteria for myocarditis. In total, 10 patients met MR criteria for myocarditis (6 showed inflammation on EMB and 4 did not, probably due to the patchy pattern of the inflammation).
ComplicationsThere were 4 major complications related to EMB: 2 perforations of the RV that required pericardiocentesis, one sustained ventricular tachycardia that required electrical cardioversion in an EMB of the RV, and one transient ischemic attack in an EMB of the LV. There were no deaths associated with EMB and all the major complications resolved without sequelae. The rate of complications in EMB of the RV was 4.4%, and 3.4% for the LV; this difference was not statistically significant.
Clinical events and prognostic predictorsAfter a median follow-up of 18 [interquartile range, 6-43] months after EMB, 11% of the patients (11/99) required HTx; 6% (6/99) required ventricular assistance (2 later received a transplant), and 9% (9/99) had severe ventricular arrhythmias (sustained ventricular tachycardia/ventricular fibrillation). During the follow-up period, 12 patients died: 2 of them had received a transplant and another 2 had received ventricular assistance (8/99 [9%] without receiving a transplant or ventricular assistance).
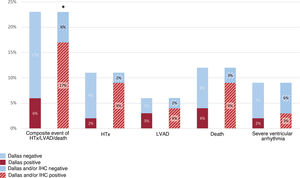
The composite event of HTx, ventricular assistance or death occurred in 23 patients (23%). In this group of patients, 26% (6/23 patients) had positive Dallas criteria on the EMB. When IHC analysis was added, 17/23 patients with HTx/ventricular assistance/death during follow-up met the criteria for inflammation, which represented 74% of the total. The difference in terms of events compared with the group without inflammation on IHC was statistically significant (P=.049) (figure 3).
Events during follow-up of patients with histological (Dallas) and immunohistochemical criteria. HTx, heart transplant; LVAD, left ventricular assist device.
*Positive vs negative Dallas or immunohistochemical criteria in patients with composite event of heart transplant, ventricular assistance or death, P = .049.
In addition, 21% of the patients with myocarditis/ICM required transplant (HTx) or LV assist device (LVAD) vs 7% of those who did not have inflammation (12/57 vs 3/42; P=.056).
Among the patients with serious arrhythmic events (9/99), 22% (2) had positive Dallas criteria; with the addition of IHC, 33% (3). Most of the patients with arrhythmic events, therefore, did not have signs of inflammation on EMB.
Among the patients with myocarditis/ICM diagnoses on EMB (57% of the total, 57/99), mean baseline LVEF was 31±15%, with a significant increase to 46±12% at the most recent follow-up (P <.01), excluding patients who had HTx and did not have a reference echocardiogram from prior to transplant with at least 3 months of follow-up. The mean LV end-diastolic diameter was 57±15mm at baseline and 54±3mm at the end of follow-up, a difference that was not statistically significant. Of the total 57 patients with myocarditis/ICM on EMB, 27 (47%) had an improvement in LVEF greater than 10%, 6 (11%) had a baseline LVEF> 50%, 12 (21%) did not improve or worsened, and 9 (16%) received HTx. Follow-up echocardiogram was not available in 3 patients.
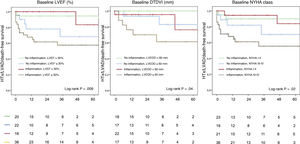
The cutoff points of LVEF ≤ 30% and left ventricular end-diastolic diameter ≥ 60mm on the baseline assessment showed a significant association with greater number of events during follow-up, especially in patients with inflammation on EMB (figure 4). Patients in New York Heart Association (NYHA) functional class III-IV with a diagnosis of inflammation also had a worse prognosis.
HTx/LVAD/death-free survival curves for various prognostic factors in 99 patients with suspected myocarditis or inflammatory cardiomyopathy who underwent EMB, shown according to presence or absence of inflammation.
EMB, endomyocardial biopsy; HTx, heart transplant; LVAD, left ventricular assist device; LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association.
In contrast, in our study, immunosuppressive treatment was not associated with a reduction in events during follow-up. Among the 20 patients treated (35% of the total patients with histologically-confirmed inflammation, 20/57), 25% required HTx/LVAD or died during follow-up vs 32% of patients with criteria for inflammation on EMB not treated with immunosuppressors (5/20 vs 12/37; P=.6). Of note, when we compared the treated patients who had a specific diagnosis of sarcoidosis, giant-cell myocarditis, or eosinophilic myocarditis with those with lymphocytic myocarditis, the rate of events was lower in the first group (2/10 [20%] vs 3/10 [30%]), although the difference was not statistically significant.
DISCUSSIONThis study reports on the largest series of patients undergoing EMB for suspected myocarditis or ICM in Spain to date. EMB provided a specific etiological diagnosis in 57% of the patients (35% in those with subacute or chronic presentation and 22% in those with acute presentation), and IHC criteria were better than Dallas criteria for the detection of myocardial inflammation. In 10 patients (10% of the total) more specific forms of myocardial inflammation were identified (sarcoidosis, eosinophilic myocarditis or giant-cell myocarditis) (figure 1).
In this series, the presence of inflammation when IHC was added as a diagnostic technique correlated with worse prognosis at follow-up, in addition to reduced LVEF and ventricular dilatation. Lastly, the incidence of major complications in EMB was 4.4%, although all of them resolved rapidly without sequelae.
Endomyocardial biopsy for the etiological diagnosis of myocarditis/inflammatory cardiomyopathy
Endomyocardial biopsy is the only technique that allows the specific etiological diagnosis of different types of myocarditis/ICM. In this series, 10% of the patients had eosinophilic myocarditis, sarcoidosis, or giant-cell myocarditis and were able to receive specific immunosuppressive treatments (figure 1). Taking into account the 57 patients with a confirmed diagnosis of myocarditis/ICM, the conditions with an accepted specific treatment constituted 18% of the patients with myocarditis/ICM on EMB. The remaining 82% corresponded to lymphocytic myocarditis, for which treatment with immunosuppressants is debated. These findings are in line with previously-published series from other countries, which observed a clear predominance for lymphocytic myocarditis, followed by eosinophilic myocarditis and sarcoidosis, and lastly giant-cell myocarditis.11,12
Regarding the higher rate of positive cases of myocarditis/ICM with the IHC criteria than with the Dallas criteria, our findings add to the evidence generated in recent years that supports the use of ICH over the Dallas criteria in patients undergoing EMB. In a meta-analysis including 61 studies and more than 10 000 EMBs, published in 2020, 50.8% of the cases met ICH criteria for myocarditis vs 8% who had positive Dallas criteria.13 Although the yield using Dallas in our series was higher than this (29%), IHC confirmed the presence of inflammation in a significantly higher number of patients (54%). We believe that the higher yield found in our cohort is related to a stricter patient selection, but our findings support that, even in selected patients, it is an essential technique for appropriate histological analysis.
The concordance between the IHC criteria for EMB and the Lake Louise MR criteria was low, with a sensitivity of 33% in patients who had MR and EMB in the same month. The Lake Louise criteria used in the study were the classic criteria, not the 2018 modified criteria that include T1/T2 mapping,14 as this technology was not yet available for a large number of our patients. In a recent study, the sensitivity of the classic and updated Lake Louise criteria was reported as 38.2% and 58.8%, respecitvely,15 so our results were not vastly different. The presence of patients with CMR criteria for myocarditis who had normal EMB appears to reflect the fundamental problem with EMB, which is its low sensitivity. This is due to the issue of sampling, as myocarditis is a focal process and EMB traditionally could not be aimed at the affected areas. However, performing EMB in the LV could increase the sensitivity of EMB if imaging shows that the inflammation predominantly affects the LV.
Inflammation as a prognostic markerOur results showed that IHC-confirmed inflammation was associated with worse prognosis, as 74% of the patients with the composite event of HTx/LVAD or death had IHC criteria of inflammation on EMB, vs 26% with positive Dallas criteria in this group (figure 3).
Taking the whole cohort into account, 21% of the patients with EBM-confirmed myocarditis/ICM required a HTx or ventricular assistance, vs 7% of those who did not have signs of inflammation, including in this group those with lymphocytic (Dallas or IHC criteria), eosinophilic, or giant-cell myocarditis, and sarcoidosis. Although the differences came close to statistical significance (P=.056), these findings overall confirm that the diagnosis of myocardial inflammation according to IHC criteria is associated with worse prognosis.16
Severe arrhythmic events occurred in 9% of the cohort. In these patients, the confirmation of myocarditis on EMB (whether using Dallas or IHC criteria) was not associated with higher number of events at follow-up (figure 3).
Other prognostic markersLVEF ≤ 30%, left ventricular end-diastolic diameter ≥ 60mm, and NYHA functional class III-IV at diagnosis had a significant association with the incidence of the composite event of HTx/ventricular assistance/death at follow-up. Although these parameters had already been proposed as prognostic factors in patients with suspected myocarditis or ICM,16 in our study we observed that, when stratified by presence of inflammation on EMB added to LVEF ≤ 30%, LVEDD ≥ 60mm and NYHA III-IV, we were able to identify those subgroups with a higher number of events at follow-up (figure 4). Therefore, EMB can add prognostic information to complement imaging tests and clinical assessment.
Among the patients with myocarditis/ICM in our cohort, 37% did not have an improvement in LVEF or needed HTx at follow-up. These findings are in stark contrast to those of other series, such as a recent German series of 210 patients with EBM-confirmed myocarditis/ICM, in which 87% had an improvement at follow-up (53% had normal LVEF after a follow-up of 2 years and 34% had at least some improvement in LVEF).17 Again, this discrepancy is probably because the indications for EMB are more restrictive in our setting, where it is still reserved for patients with poor progress who do not respond to standard medical treatment.
Immunosuppressive treatmentImmunosuppressive treatment was not associated with better prognosis nor with significant improvement in LVEF in our series, although only 20 patients were treated, and they also had varying etiologies of ICM, which makes it difficult to draw solid conclusions. All patients with eosinophilic myocarditis, sarcoidosis, or giant-cell myocarditis were treated. In the case of lymphocytic myocarditis, although immunosuppressive treatment can be considered for chronic forms,18,19 only 28% of our cohort with this diagnosis received treatment. This is because the IHC analysis was done retrospectively in many cases and the indication for immunosuppressive treatment in borderline myocarditis (inflammatory infiltrate without necrosis) is more controversial.
Some randomized trials have demonstrated that immunosuppressive treatment added to conventional treatment is superior to conventional treatment alone in terms of improvement in LVEF and functional class,18,19 but a systematic review that included 8 trials using glucocorticoids20 found no prognostic benefit. In the case of acute lymphocytic myocarditis, the recommended treatment is supportive for HF; there are no specific treatments,5 although a trial is currently underway (NCT03018834) to evaluate the efficacy of the interleukin 1 inhibitor anakinra in this group of patients.
In summary, given that current treatment regimens are highly heterogeneous, and taking into account that IHC-confirmed inflammation could be a prognostic marker, larger clinical trials are needed to standardize treatment of myocarditis and ICM. Notwithstanding, given that the presence of inflammation with the addition of IHC techniques on EMB is associated with worse prognosis in certain patients, we think that immunosuppressive treatment is an option that should be considered for patients with ICM.
LimitationsThis is a single-center, descriptive, retrospective study, based on a cohort of patients treated in a tertiary hospital with experience in EMB. Therefore, our series is subject to an undeniable bias in selection and survival. Furthermore, both neurohormonal treatment of HF and the immunosuppressive regimens used have changed over time, making it difficult to assess the true impact of immunosuppressive treatment for the treatment of myocarditis/ICM. However, the same, experienced pathologist reviewed all the histology samples, so there was no interobserver variability.
CONCLUSIONSEndomyocardial biopsy established an etiological diagnosis in more than half of the cases of suspected myocarditis or ICM when IHC techniques for the detection of inflammation were added. On a practical level, 1 in every 5 patients diagnosed benefited from a specific immunosuppressive treatment. Baseline LVEF ≤ 30%, LVEDD ≥ 60mm and NYHA III-IV were associated with clinical events at follow-up and, precisely in this subgroup, the presence of inflammation identified patients with increased risk. Based on our experience, we recommend performing EMB and using IHC techniques in the evaluation of patients with suspected myocarditis or ICM.
FUNDINGThis study was performed with partial funding from Instituto de Salud Carlos III (PI20/0320).
AUTHORS’ CONTRIBUTIONSData collection: F. Domínguez, R. Cobas Paz, L. Escobar López, F. de Frutos, M. Cobo Marcos, E. González López, FJ. Hernández Pérez, A. Briceño. Performing endomyocardial biopsies: J.F. Oteo Domínguez. Analysis of endomyocardial biopsies: C. Salas Antón, M. Colomés Iess. Statisical analysis: F. Domínguez, R. Cobas Paz. Writing and review of the manuscript: F. Domínguez, R. Cobas Paz, L. Escobar López, F. de Frutos, M. Cobo Marcos, E. González López, F.J. Hernández Pérez, C. Mitroi, M. Rivas-Lasarte, A. Briceño, M. Gómez-Bueno, P. García-Pavía, J. Segovia-Cubero.
CONFLICTS OF INTERESTP. García-Pavía is associate editor of the Revista Española de Cardiología; the journal's established editorial policy was followed to ensure impartial handling of the manuscript.
The other authors declare no conflict of interests.
- –
EMB is the only technique that can confirm the etiological diagnosis of myocarditis and ICM.
- –
In recent years, IHC techniques have helped increase the diagnostic yield for the detection of myocardial inflammation.
- –
Some studies have proposed that detection of inflammation using IHC could be of prognostic value.
- –
EMB is a safe technique in experienced centers in our setting and provides an etiological diagnosis in almost 60% of patients with suspected myocarditis or ICM.
- –
IHC not only increases the diagnostic yield of myocardial inflammation, but also identifies the patients with worse prognosis among those with ventricular dysfunction of unknown cause.