Atrial fibrillation is the most common sustained arrhythmia. Because of its potentially serious clinical consequences (heart failure, stroke, and cognitive impairment), atrial fibrillation has important socioeconomic and health implications. This article reviews the major studies on the epidemiology of atrial fibrillation in Spain. Recent data suggest that in people older than 40 years, the prevalence of atrial fibrillation may be more than 4%. Given the current Spanish demography, these data would imply that more than 1 million people in Spain have atrial fibrillation.
Keywords
Atrial fibrillation (AF) is the most common sustained arrhythmia.1 It is clinically associated with heart failure, increases the risk of stroke, and causes symptoms which considerably reduce quality of life. It is unclear whether the presence of AF alone increases mortality, although some studies indicate that this is the case, both in patients with and without heart disease.2 This excess mortality was historically considered to be due to increases in heart failure and stroke associated with AF, but a recent publication has indicated that AF increases the risk of sudden death.3 Given that no studies have specifically tried to determine whether AF independently increases mortality, we cannot rule out that AF is more than a mere “companion” marker of other factors affecting survival.
As in other areas of cardiology, extraordinary progress has been made in understanding AF over the past 20 years.
We now know that the pathophysiology is initiated in many cases by bursts of abnormal electrical discharges, which require rapid, irregular activation of the atria. AF can initially be paroxysmal (with spontaneous terminations) and evolves to a persistent form when an anatomically and electrically favorable atrial substrate exists alongside the trigger points. This anatomical and electrical substrate is produced over time by AF itself, through the phenomenon known as “remodeling”, a pernicious process summarized by the phrase “AF promotes AF”.4 In focal AF, arrhythmogenic foci are generally in the vicinity of the pulmonary veins. When it becomes persistent AF, there is often a greater degree of atrial disease. The recent classification of AF as paroxysmal, persistent, and permanent aims to reflect the deterioration of the arrhythmia over time. It is not yet known why some patients progress rapidly and others do not.1
Treatment of AF and its consequences has for some time been based on the use of antiarrhythmic drugs and anticoagulants.5 Antiarrhythmic drugs have not changed substantially in recent years. Beta blockers and calcium channel blockers are still used to control the ventricular response, while class I and class III antiarrhythmics are used to restore and maintain sinus rhythm. The latter show approximately 50% effectiveness overall, although undesirable effects appear in up to 30% of patients.5,6 Noninvasive techniques that aim to electrically isolate the pulmonary veins have shown very good results in terms of reducing recurrences of arrhythmia in selected patients.5,7 Anticoagulants have evolved more than antiarrhythmic drugs, with new indications for their use in recent years. New drugs have also been discovered that appear to be more effective and safer in some populations than the classic vitamin K antagonists. Devices designed to occlude the left atrial appendage are also available and can help patients with AF and high embolic risk when anticoagulants are contraindicated.8
Much of this progress has occurred in just 10 years, as evidenced by a reading of reviews of AF literature written just a decade ago.9 Over this period, knowledge has been updated in clinical guidelines dedicated specifically to AF.10 The present article reviews the published data on the epidemiology of AF in Spain, information that is essential in assessing the social, health, and economic consequences of the disease. It has been estimated that the annual cost of each AF patient in Europe is between €450 and €3000.11
ANALYZING THE EPIDEMIOLOGY OF ATRIAL FIBRILLATION: METHODOLOGICAL FACTORSAF is the most common sustained cardiac arrhythmia and many articles report that it affects approximately 1% of the population.1 The truth is, however, that the prevalence of AF depends on the method chosen to detect it and the characteristics of the study population. The following factors affect the results of published studies:
- •
Population characteristics: AF is closely linked to age and the presence of heart disease. Recruiting patients in cardiology clinics rather than in primary care can affect study results, in terms of both the underlying disease and the treatments used. Some treatments, angiotensin converting enzyme inhibitors among them, reduce the incidence of AF.12
- •
Method of AF diagnosis: in most studies, AF is diagnosed using surface electrocardiogram (ECG); therefore, a positive diagnosis can only be obtained if the patient is experiencing AF when the ECG is performed. For obvious reasons, this method can underestimate the prevalence of paroxysmal AF, which may have clinical implications similar to chronic forms of AF. Other forms of electrocardiographic recording allow for much longer periods of monitoring, making it easier to detect subclinical AF and short bursts.13
- •
Differential AF diagnosis: most studies do not distinguish between atrial flutter and AF, and assume that they have similar clinical implications. Differential diagnosis is sometimes difficult even with intracardiac electrograms, but the fact remains that common flutter, if detected, could be cured with a simple cavotricuspid isthmus ablation.14
Most epidemiological studies of AF are American and have used surface ECG to detect AF. One of the first published studies analyzed the prevalence of AF in 122 043 males aged 16 to 50 years entering U.S. Air Force pilot training. In that study, AF was detected in only 5 individuals.15 The Framingham study later indicated a prevalence of 0.4% to 1% in the general population, although rates were observed to increase progressively with age, up to 8% in people older than 80 years.16 This relationship with age was confirmed in the ATRIA study, which analyzed the ECGs of 1.89 million American adults in 1996 and 1997 and identified 17 974 individuals with AF.17 The prevalence of AF in those younger than 55 years was 0.1%, compared to 9% in those older than 80. Both studies also found that AF was more common in men than in women in all age groups.16,17 The authors of the Framingham study suggested that the figures might double after 50 years, given the estimates for population aging.16 Recent data indicate that the prevalence of AF is increasing, possibly as a result of population aging, although other factors cannot be excluded.18
European StudiesThe Rotterdam study analyzed the incidence and prevalence of AF in a population over 55 years of age during a 7-year period.19 A total of 7983 patients were included and the investigators reported prevalence rates of 5.5% in the total population; in the 55-59 year age group the rate was 0.7%, compared to 17.8% in the 85 years and older group. Similar results were observed in an analysis published by the European Society of Cardiology.20
In Portugal, the FAMA study assessed AF prevalence in 10 447 randomly selected individuals over 40 years of age. Overall prevalence was 2.5%, with similar rates in men and women, and increased with age.21
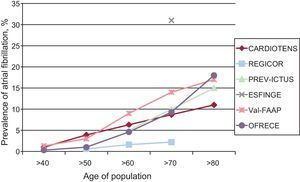
Spanish StudiesIn 1999, the CARDIOTENS study reported an overall prevalence for “chronic” AF of 4.8%, a rate which increased with each decade of life (from 1% in the under-50 group to 11.1% in those aged 80 years or more). The study included consecutive patients attended in primary care or cardiology departments, and so cannot be considered population-wide. Results were based on clinical history and an ECG was not a requirement.22
The REGICOR study was conducted in 2001 using random sampling in population strata and reported an AF prevalence of 0.7%, although it was not specifically designed to study AF.23 The population over 74 years of age was excluded.
In the PREV-ICTUS study, carried out in 2007, the ECGs of 7108 patients over 60 years of age (more than 70% with a history of hypertension [HT]) were analyzed and the AF prevalence was 8.5% (7.9% in women and 9.3% in men). Prevalence increased with age, from 4.5% at 60 to 64 years to 16.5% in those older than 85 years.24
The 2012 ESFINGE study analyzed the prevalence of AF in patients of both sexes aged ≥70 years who were hospitalized in internal medicine units or geriatric wards.25 Overall prevalence was 31.3%, and 88.7% of patients had AF before the admission. AF was persistent, long-term, or permanent in 728 cases (89.1%); in the remaining 51 cases (6.2%) it was identified as a first episode (paroxysmal or persistent). Only 4.1% of cases showed a clear secondary cause of AF.
Also published in 2012, the Val-FAAP study included 119 526 primary care patients (mean age, 52.9 [15.2] years; 40.9% male) over a 5-day period and found an AF prevalence of 6.1%, a percentage that increased with age, presence of HT, and male sex.26
The OFRECE study began in early 2009 and was sponsored by the Spanish Society of Cardiology's Research Agency. A total of 8400 subjects over 40 years of age were analyzed. Patients treated at primary care centers were randomly selected in age and sex strata by participating clinicians. The participating primary care centers were also randomly sampled.27 A total of 50 local coordinators were appointed in 46 provinces, with each being responsible for coordinating 10 randomly selected physicians. Each physician agreed to include 20 individuals in the study. The sample is representative of the current Spanish population by age. AF was deemed to be present if it appeared on ECG during the primary care physician visit or if there was a history of nonpermanent (paroxysmal or persistent) AF in the patient's medical records. ECG readings were centralized. Of the patients included, 51% had HT (90% were receiving medication), 40% had hypercholesterolemia, 15% diabetes mellitus, 5% ischemic heart disease, and nearly 7% had thyroid problems.
In total, 4.9% of the subjects were diagnosed with AF (4.4% known, 0.5% unknown). The majority (66%) had permanent AF, 23% had paroxysmal AF, and 11% persistent AF. Prevalence rates were similar for men and women, with AF being slightly more common in men up to 80 years of age, but more frequent in women beyond that age. The OFRECE study also confirmed the increase in prevalence of AF with age; prevalence was 0.3% in the 40-49 year age group, 1% in those aged 50-59 years, 4.6% in those aged 60-69, 9.3% at 70-79 years, and almost 18% in individuals over 80 years of age. Therefore, AF prevalence doubled with each decade of life beyond 60 years of age. Obesity, HT, hypercholesterolemia, and diabetes mellitus were more likely in patients with AF.
In summary, the prevalence of AF in Spain is high and consistent with rates found in other populations (Figure). Extrapolating from the OFRECE study data, of the nearly 24 million people aged over 40 in the Spanish population, 1 million would have AF and about 100 000 of them would be unidentified.
Approximate prevalence of atrial fibrillation in Spain; data collected in different studies from different populations.22–27
As with prevalence, the incidence of AF increases with age and presence of cardiovascular disease. In the Rotterdam study, incidence in the group aged 55 to 59 years was 1.1/1000 person-years, and increased to 20.7/1000 person-years in the 80 to 84 years age group. Lifetime risk of AF was 23.8% in men and 22.2% in women.19 In another longitudinal study, which lasted for 44 years and included almost 4000 healthy men, it was found that 7.5% had AF. The estimated risk of developing AF was 0.5/1000 person-years before 50 years of age, although the risk increased to 9.7/1000 person-years after 70 years of age.28 Given a 95-year life-span, it is estimated that men who have turned 40 have a 25% chance of developing AF.16,19
As already mentioned, population estimates suggest that the incidence and prevalence of AF will continue to increase at an alarming rate in coming years.29
To date, there have been no studies to investigate the incidence of AF in Spain.
DIFFERENT APPROACHES TO DIAGNOSING ATRIAL FIBRILLATIONIn relation to the prevalence rate, it is interesting to note the existence of subclinical AF. Patients who are asymptomatic will not seek medical care, so they are only diagnosed through the use of pulse or heart rate monitoring.
The results of a 1-week campaign to identify AF by taking the pulse of patients over 65 years of age with no history of arrhythmia were published recently. Of the 1532 patients who responded to the request for examination (mean age, 72 years; 57% women), only 1% had previously undiagnosed AF.30
In another approach to this problem, investigators took advantage of the dual-chamber pacemakers implanted in more than 2500 patients over 65 years of age who had HT and no history of AF.13 AF was defined as episodes of atrial rate over 190 bpm for a 6-min duration. At 2.5 years, 35% of patients had AF, and of those, 1 in 6 had clinical FA.
ASSOCIATED ILLNESSESThe association between AF and AH was observed in 1995, with hypertensive patients having a relative risk of developing AF of 1.42 compared to those without HT. Although the increased risk appears to be small, the high prevalence of HT means it is the cardiovascular disease most commonly observed in patients with AF.28
In Spain, the PREHVIA study analyzed the prevalence of AF in hypertensive patients in Andalusia. Of the 570 patients enrolled (mean age, 65 years; 54.5% women), 5.1% showed AF on the ECG.31
The FAPRES registry, which was published in 2010, investigated the prevalence of AF in hypertensive patients older than 64 years.32 Each of the 69 participating investigators included the first 3 hypertensive patients over 64 years of age consulting in primary care or a specialized HT unit on the first day of the week for 5 weeks.32 AF was observed in 10.3% (6.7% by ECG and 3.6% by clinical history) of the 1028 patients studied (mean age, 72 years). Factors associated with AF were age, alcohol consumption, structural heart disease, and glomerular filtration rate. Patients without AF performed more exercise than those with the condition. In other words, in general series, AF is associated with most of the usual cardiovascular risk factors, including lack of exercise. Its association with obesity is considered particularly serious and that may be one of the reasons for the apparent increase in the prevalence of AF, along with one of its consequences, sleep apnea.33,34 However, it is relatively rare in patients with coronary artery disease and stable angina.35 AF is more common when acute myocardial infarction is present and is known to lead to a poorer prognosis.36
Coronary surgery is also a risk factor for AF. A Spanish study found a 23% incidence of AF in the first month after surgery in a consecutive series of 102 patients, independently of whether cardiopulmonary bypass was used for revascularization.37
Many other factors affecting the atria have also been associated with AF, including valve disease,38 cardiomyopathy,39 and congenital heart disease.40 Intense and prolonged exercise also has been associated with AF.41 Familial forms related to certain genetic expressions that favor its appearance have also been observed.42,43
Finally, AF has been identified as a possible contributor to clinical cognitive impairment.44
LONE ATRIAL FIBRILLATIONWhen AF occurs in patients under 60 years of age without clinical or echocardiographic evidence of associated cardiopulmonary disease, including HT, it is known as lone AF.45 This form of AF has regained significance today, as it may be the best candidate for ablation techniques. In these cases, where there is no structural or metabolic cause, arrhythmogenesis stems largely from “venous” rather than “atrial” causes.46 This form of AF is observed in 10% to 20% of patients with AF in the series studied.47 In clinical practice, this type of AF will almost always be associated with paroxysmal AF. However, in a Spanish registry of 1515 patients with persistent AF referred for cardioversion, 49% had no evidence of structural heart disease.48 In these cases, it is important to stratify risk and, from the point of view of cost-effectiveness, employ first-line treatments.49–51
CONCLUSIONSAF is the most common sustained arrhythmia. Due to the severity of some of its clinical consequences (heart failure, stroke, and cognitive impairment), it is important in terms of both its socioeconomic and health impact. Its prevalence in Spain has been analyzed in selected groups of people, and the rates are similar to those observed in other countries. Recent population studies in individuals over 40 years of age have found prevalence rates in Spain >4%, a figure which, if confirmed and extrapolated, suggests that almost 1 million people in Spain may have AF. We have no data to help determine whether prevalence remains unchanged, or whether it is increasing or decreasing. However, given the magnitude of the problem, there is an urgent need to invest in knowledge that will aid in correctly stratifying patient risk and in determining, from the point of view of cost-effectiveness, which treatments should be considered as the first choice.
CONFLICTS OF INTERESTNone declared.