Up to 4% of patients with acute chest pain, normal electrocardiogram, and negative troponins present major adverse cardiac events as a result of undiagnosed acute coronary syndrome. Our aim was to compare the diagnostic performance of multidetector computed tomography and exercise echocardiography in patients with a low-to-intermediate probability of coronary artery disease.
MethodsWe prospectively included 69 patients with acute chest pain, normal electrocardiogram, and negative troponins who underwent coronary tomography angiography and exercise echocardiography. Patients with coronary stenosis ≥ 50% or Agatston calcium score ≥ 400 on coronary tomography angiography or positive exercise echocardiography, or with inconclusive results, were admitted to rule out acute coronary syndrome.
ResultsAn acute coronary syndrome was confirmed in 17 patients (24.6%). This was lower than the suspected 42% based on coronary tomography angiography (P<.05) and not significantly different than the suspected 29% based on the results of exercise echocardiography (P=.56). Exercise echocardiography was normal in up to 37% of patients with pathological findings on coronary tomography angiography. The latter technique provided a higher sensitivity (100% vs 82.3%; P=.21) but lower specificity (76.9% vs 88.4%; P=.12) than exercise echocardiography for the diagnosis of acute coronary syndrome, although without reaching statistical significance. Increasing the stenosis cutoff point to 70% increased the specificity of coronary tomography angiography to 88.4%, while maintaining high sensitivity.
ConclusionsCoronary tomography angiography offers a valid alternative to exercise echocardiography for the diagnosis of acute coronary syndrome among patients with low-to-intermediate probability of coronary artery disease. A combination of both techniques could improve the diagnosis of acute coronary syndrome.
Keywords
The absence of electrocardiographic signs of ischemia or myocardial necrosis markers is common in patients with chest pain and acute coronary syndrome (ACS). Stratification based on clinical parameters has limited usefulness in the diagnosis and prognosis of these patients.1,2 Up to 60% of patients admitted for study do not have ACS.3 Furthermore, ACS is misdiagnosed in up to 4% of patients with ACS, who are mistakenly discharged.4 In this group of patients, the mortality or infarction rate may be 3% per month and up to 4.8% at 6 months.5 For this reason, chest pain units have been implemented and protocols established to expedite the diagnosis of these patients.6 These protocols include the performance of noninvasive techniques such as stress testing, exercise echocardiography, or myocardial perfusion imaging, which detect hemodynamically significant lesions by demonstrating ischemia inducible by stress.7,8 However, these techniques have limited usefulness due to their low diagnostic sensitivity, which makes it difficult to definitively rule out ACS in the emergency department.9,10 Noninvasive coronary angiography using multidetector computed tomography (MDCT) has also been used to rule out ACS in the emergency department.11–14 The information provided by MDCT is fundamentally anatomical and indicates the presence and extent of coronary artery disease (CAD). However, the information provided by ischemia detection tests is functional. This study compared the diagnostic performance of MDCT to that of exercise echocardiography in patients with suspected ACS and a low-to-intermediate probability of CAD.
METHODSStudy PatientsThe characteristics of the chest pain unit in our hospital have been previously described.3 The unit applies a diagnostic protocol to assess patients with nontraumatic chest pain, according to the guidelines of the Spanish Society of Cardiology.15
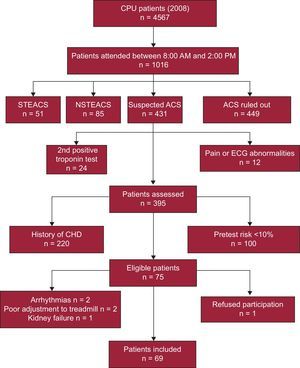
This study consecutively included patients without a history of cardiac disease who attended the emergency department with typical or atypical angina during working hours between Tuesday and Friday in 2008. Only patients with a negative troponin level within 6h of pain onset and no electrocardiographic signs of ischemia were included. These patients are typically considered candidates for exercise stress testing. The study also included patients older than 35 years who had a pretest probability of CAD greater than 10% according to the nomograms developed by Pryor et al.16Figure 1 shows the patient selection flowchart. Exclusion criteria were contraindications to MDCT, such as irregular heart rhythm, kidney failure (creatinine > 1.3mg/dL), anaphylactic reaction to iodine contrast, contraindications to beta blockers, and contraindications to exercise testing.
Study ProtocolEligible patients underwent MDCT and exercise echocardiography. Exercise echocardiography was performed first in 90% of patients to avoid the negative chronotropic effect of the beta blockers needed for MDCT. Patients with negative results were discharged except when the consultant cardiologist decided to admit the patient for catheterization due to the character and persistence of chest pain. A presumptive diagnosis of ACS was established in patients with a positive exercise echocardiogram and in patients with positive MDCT, defined as the presence of at least 1 coronary lesion with stenosis ≥ 50% or an Agatston score ≥ 400. All these patients were included in the study and underwent treatment. During admission, all included patients underwent cardiac catheterization except for 3 patients who were excluded by the attending physician. Patients with inconclusive results on MDCT or exercise echocardiography were considered to have positive results for the purposes of statistical analysis. The study was approved by the hospital's ethics committee and all patients signed their informed consent.
Multidetector Computed Tomography AngiographyA 64-slice scanner (Sensation 64, Siemens Medical Solutions; Forchheim, Germany) was used. Patients with a heart rate > 65 were treated with beta blockers. Firstly, the Agatston calcium score was calculated by acquiring low-resolution images without contrast at a slice thickness of 3mm. Angiography was not performed in patients with chest pain and a documented Agatston score > 400 due to the difficulty of interpreting the coronary lumen and the high prevalence of myocardial ischemia.17 The remaining patients were administered 400μg of sublingual nitroglycerin. After administration of a bolus of 80 (10) mL of contrast (Iomeron 400®, Rovi), angiography was performed at a trigger threshold of 120 HU in the ascending aorta. Acquisition parameters were as follows: collimation, 64mm×0.6 mm; rotation time, 370ms (equivalent to a time resolution of 185ms); tube voltage, 120kV; and effective tube current, 550mA-850mA. Dose-modulation techniques were used and image acquisition was optimized between 30% and 70% of the RR interval.
Subsequently, cardiac volume was reconstructed at a slice thickness of 0.75mm and with an increase of 0.4mm between slices at 60%, 65%, 70%, and 75% of the RR interval. Images were interpreted using the Circulation® software package (Siemens; Erlangen, Germany), which allows volumetric and multiplanar reconstructions and maximum-intensity projections.
Each study was jointly evaluated by an experienced radiologist and an experienced cardiologist, who together determined the presence of luminal area stenosis<50% or ≥ 50%, nonassessable segments, and the cause of nonassessment (motion artifact or severe calcification). Differences of opinion were resolved by a third observer. The mean interpretation time was 18(8) min.
Exercise EchocardiographyPatients underwent symptom-limited treadmill exercise testing using the Bruce protocol under electrocardiographic monitoring using a Vivid 7 ultrasound system (General Electric) equipped with an exercise protocol. Images were acquired at baseline, immediately after the test, and during recuperation in parasternal long-axis and parasternal short-axis views and in 2-chamber and 4-chamber views. An echo enhancer (Sonovue®, Rovi, Madrid, Spain) was only used to improve endocardial border delineation in the case of a suboptimal acoustic window. The studies were evaluated by an experienced echocardiologist, without access to the results of other tests, according to the 17-segment model proposed by the American Heart Association. The myocardial wall motion study was considered positive in the presence of segmental wall-motion abnormalities at baseline or when induced by exercise in at least 2 adjacent segments.18
Due to the exploratory nature of this study, the overall result of exercise echocardiography was considered positive when at least of the 3 components (clinical suspicion, electrocardiographic changes, and wall-motion abnormalities) was positive. The study was considered inconclusive when the wall-motion study was not conclusive, a metabolic equivalents score of 6 was not reached, or 85% of the predicted maximum heart rate was not achieved.
Definition of Acute Coronary SyndromeAcute coronary syndrome was confirmed by the presence of typical or atypical angina plus one of the following characteristics: presence of coronary lesions with > 70% stenosis determined by cardiac catheterization; ischemia induced in a diagnostic test other than exercise echocardiography; or the presence of cardiac death, acute myocardial infarction, or need for revascularization at 6-month follow-up.18
Statistical AnalysisContinuous variables are described as mean (standard deviation). Between-groups comparisons were performed using the Student t test for continuous variables and the chi-square test for discrete variables using Yates correction as needed. A P value < .05 was used as a cutoff for statistical significance.18
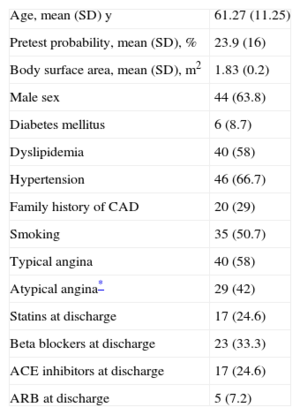
RESULTSTable 1 shows the characteristics of the 69 patients. The mean pretest probability of CAD was 24% (16%): 26% (15%) in men and 17% (20%) in women; P<.05. A final diagnosis of ACS was established in 17 patients (24.6%) and in 16 of these patients the diagnosis was based on the presence of typical or atypical angina and coronary stenosis greater than 70% on cardiac catheterization. In addition, 1 case of sudden death was recorded during follow-up in a patient with a lesion of 60% on cardiac catheterization.
Clinical Characteristics of the Study Population (No.=69)
| Age, mean (SD) y | 61.27 (11.25) |
| Pretest probability, mean (SD), % | 23.9 (16) |
| Body surface area, mean (SD), m2 | 1.83 (0.2) |
| Male sex | 44 (63.8) |
| Diabetes mellitus | 6 (8.7) |
| Dyslipidemia | 40 (58) |
| Hypertension | 46 (66.7) |
| Family history of CAD | 20 (29) |
| Smoking | 35 (50.7) |
| Typical angina | 40 (58) |
| Atypical angina* | 29 (42) |
| Statins at discharge | 17 (24.6) |
| Beta blockers at discharge | 23 (33.3) |
| ACE inhibitors at discharge | 17 (24.6) |
| ARB at discharge | 5 (7.2) |
ACE, angiotensin-converting enzyme; ARB, angiotensin-receptor blockers; CAD, coronary artery disease; SD, standard deviation.
Data are expressed as No. (%) or mean (standard deviation).
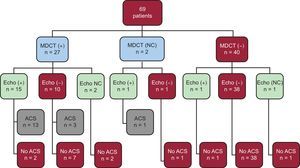
In 40 patients (58%), MDCT was normal or showed no significant lesions (stenosis<50%). Multidetector computed tomography was positive in 27 (39.1%) patients: 22 had > 50% stenosis and 5 had an Agatston score > 400. In 2 patients (2.9%) ≥ 1 proximal or middle coronary segment could not be assessed due to motion artifacts. Thus, based on MDCT, a presumptive diagnosis of ACS was established in 29 (42%) patients. All the patients with stenosis ≥ 50% on MDCT had an Agatston score > 0. In addition, 4 of the 5 patients with an Agatston score > 400 had ACS with coronary stenosis > 70% on cardiac catheterization. One patient with a calcium score = 0 and a coronary segment that could not be assessed had a severe lesion in this segment on cardiac catheterization.
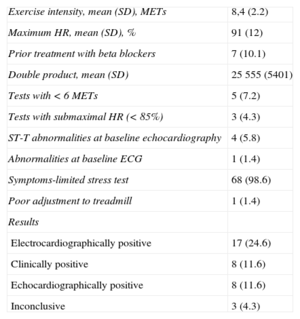
Exercise Echocardiography FindingsExercise echocardiography was negative in 49 (71%) patients, positive in 17 (24.6%), but inconclusive in 3 (4.3%) due to poor image quality or the patient achieving 85% of the predicted maximum heart rate. Table 2 shows the characteristics of exercise echocardiography. Based on the results of exercise echocardiography, ACS was suspected in 20 (29%) patients.
Characteristics of Exercise Echocardiography
| Exercise intensity, mean (SD), METs | 8,4 (2.2) |
| Maximum HR, mean (SD), % | 91 (12) |
| Prior treatment with beta blockers | 7 (10.1) |
| Double product, mean (SD) | 25 555 (5401) |
| Tests with < 6 METs | 5 (7.2) |
| Tests with submaximal HR (< 85%) | 3 (4.3) |
| ST-T abnormalities at baseline echocardiography | 4 (5.8) |
| Abnormalities at baseline ECG | 1 (1.4) |
| Symptoms-limited stress test | 68 (98.6) |
| Poor adjustment to treadmill | 1 (1.4) |
| Results | |
| Electrocardiographically positive | 17 (24.6) |
| Clinically positive | 8 (11.6) |
| Echocardiographically positive | 8 (11.6) |
| Inconclusive | 3 (4.3) |
ECG, electrocardiogram; HR, heart rate; MET, metabolic equivalent; SD, standard deviation.
Data are expressed as No. (%) or mean (standard deviation).
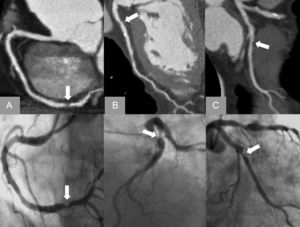
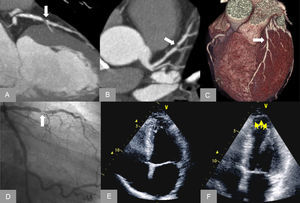
Figure 2 shows the relationship between the diagnostic tests and the diagnosis of ACS. Acute coronary syndrome was correctly ruled out in all patients with a normal MDCT. The exercise echocardiogram was positive in 1 of these patients and inconclusive in another. However, of the 29 patients with positive or inconclusive MDCT, exercise echocardiography was positive in 16 patients (55.2%), negative in 11 (37.9%), and inconclusive in 2. A final diagnosis of ACS was confirmed in 58.6% of suspected cases of ACS by MDCT and in 66.7% of suspected cases of ACS by exercise echocardiography (P=.56). Acute coronary syndrome was confirmed in 14 of the 17 patients with positive exercise echocardiography but in none of the 3 patients with inconclusive findings. Exercise echocardiography was negative in 3 patients with ACS. Figures 3 and 4 show 2 examples of concordance between negative MDCT and positive cardiac catheterization and exercise echocardiography.
Multidetector computed tomography. Curved multiplanar reconstructions of the right coronary artery (A), left anterior descending artery (B) and circumflex artery (C) showing significant coronary lesions in the 3 vessels confirmed by cardiac catheterization (lower line) in a patient with negative exercise echocardiogram.
Curved multiplanar reconstructions (A and B) and volumetric reconstructions (C) in a patient with mixed lesion with severe stenosis in the left anterior descending artery confirmed by cardiac catheterization (D). End-systolic frame on exercise echocardiography shows a dyskinetic area at the apex (arrows) inducible with exercise (E), which is not present at rest (F).
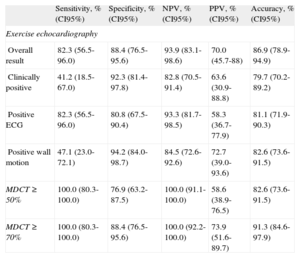
Using a ≥ 50% stenosis cutoff value, the sensitivity of MDCT was greater than that of exercise echocardiography in detecting ACS in this population (100% vs 82.3%; P>.05), but its specificity was lower (76.9% vs 88.4%: P>.05) (Table 3). Notably, when the stenosis cutoff value was raised to ≥ 70% in the retrospective analysis, the specificity of MDCT increased to that of exercise echocardiography (88.4% with both techniques) while maintaining 100% sensitivity. Separate analysis of the 3 exercise echocardiography components showed the low sensitivity but high specificity of clinical suspicion and inducible ventricular wall-motion abnormalities in detecting ACS. The assessment of electrocardiographic abnormalities alone during exercise showed acceptable values of sensitivity and specificity (82.3% and 80.8%, respectively), but a low positive predictive value (58.3%). The diagnostic accuracy of exercise echocardiography was slightly higher than that of MDCT using a 50% stenosis cutoff value (Table 3).
Diagnostic Value of Exercise Echocardiography and Multidetector Computed Tomography
| Sensitivity, % (CI95%) | Specificity, % (CI95%) | NPV, % (CI95%) | PPV, % (CI95%) | Accuracy, % (CI95%) | |
| Exercise echocardiography | |||||
| Overall result | 82.3 (56.5-96.0) | 88.4 (76.5-95.6) | 93.9 (83.1-98.6) | 70.0 (45.7-88) | 86.9 (78.9-94.9) |
| Clinically positive | 41.2 (18.5-67.0) | 92.3 (81.4-97.8) | 82.8 (70.5-91.4) | 63.6 (30.9-88.8) | 79.7 (70.2-89.2) |
| Positive ECG | 82.3 (56.5-96.0) | 80.8 (67.5-90.4) | 93.3 (81.7-98.5) | 58.3 (36.7-77.9) | 81.1 (71.9-90.3) |
| Positive wall motion | 47.1 (23.0-72.1) | 94.2 (84.0-98.7) | 84.5 (72.6-92.6) | 72.7 (39.0-93.6) | 82.6 (73.6-91.5) |
| MDCT ≥ 50% | 100.0 (80.3-100.0) | 76.9 (63.2-87.5) | 100.0 (91.1-100.0) | 58.6 (38.9-76.5) | 82.6 (73.6-91.5) |
| MDCT ≥ 70% | 100.0 (80.3-100.0) | 88.4 (76.5-95.6) | 100.0 (92.2-100.0) | 73.9 (51.6-89.7) | 91.3 (84.6-97.9) |
95%CI, 95% confidence interval; ECG, electrocardiogram; MDCT, multidetector computed tomography; NPV, negative predictive value; PPV, positive predictive value.
P value not significant (>.05) for all comparisons between the overall results of exercise echocardiography and multidetector computed tomography using a cutoff value of 50% or 70%.
Cardiac catheterization was performed at admission in 29 patients. In 26 of these patients, the procedure was performed because of positive results of either exercise echocardiography or MDCT, or both. The attending clinical cardiologist also ordered cardiac catheterization procedures in 3 patients with normal test results who had recurrent chest pain, and rejected the use of cardiac catheterization in 3 patients with lesions ≥ 50% on MDCT and normal exercise echocardiography.
During admission, 12 patients underwent revascularization. All 12 patients had positive MDCT, 11 had positive exercise echocardiography, and 1 had negative exercise echocardiography. One sudden death was recorded at 5 months in a patient with a lesion > 70% on MDCT, negative results on exercise echocardiography, and 60% stenosis on cardiac catheterization. In addition, 2 patients with an initial diagnosis of ACS underwent urgent revascularization, 1 of whom initially received medical treatment. At 4-year follow-up, the other patient underwent angioplasty for a severe (50%) lesion on initial MDCT. The lesion was not responsible for the initial ACS.
DISCUSSIONThis study provides several noteworthy results. A normal MDCT or coronary stenosis < 50% on MDCT excluded ACS in a population with a nonnegligible prevalence of CAD (24.6%). The high sensitivity of MDCT contrasts with its modest specificity of 76.9%, which is significantly less than the 88.4% provided by exercise echocardiography. As expected, there were great disparities between the 2 tests. Up to 37% of patients with positive MDCT had a normal exercise echocardiogram and only a minority of these patients (3 patients in our study) had ACS. In contrast, the majority of the 17 patients with positive exercise echocardiography had significant lesions on MDCT (15 patients); the lesions were confirmed by cardiac catheterization in 13 of these patients, leading to a final diagnosis of ACS.
The presence of significant CAD in individuals at risk can be detected by MDCT even before the onset of symptoms.19,20 Recently, several multicenter trials have evaluated MDCT vs conventional diagnostic strategies in patients with a low-to-intermediate risk of ACS.12–14 Overall, the results suggest that MDCT is a faster and equally safe alternative to conventional clinical management. A normal MDCT indicates an almost negligible risk of adverse cardiac events. However, it should be noted that the prevalence of ACS or significant CAD in these studies was very low, ranging between 3.5% and 8%. Under these conditions, the negative predictive value of the techniques is very high. In our study, however, the prevalence of ACS reached 24.6% and yet MDCT maintained its high negative predictive value. Controversy exists regarding the benefit of the technique in relation to its cost-effectiveness. Goldstein et al14 demonstrated a net profit in the use of MDCT vs rest-stress myocardial perfusion imaging. However, Hoffman et al13 found no significant differences between MDCT and a conventional approach when the choice of test was decided by the physician. All studies have shown that the use of MDCT leads to a higher percentage of early discharge and reduced stay in the emergency department, thereby potentially reducing costs. However, as found in our study, MDCT has low diagnostic specificity and may lead to an increase in the number of functional tests subsequently performed.13 In this regard, our study found that the use of a 50% coronary stenosis cutoff value led to a presumptive diagnosis of ACS. This percentage is less than the 70% cutoff value required on coronary angiography, although previous studies have shown that luminal area stenosis 50% on MDCT is equivalent to a luminal diameter stenosis of 70% on catheterization. Another factor determining the low specificity was the high percentage of extensive coronary calcification, which occurred in 13% of our patients and is associated with the overestimation of luminal stenosis.21 Some of these factors can be corrected, as shown by the fact that raising the cutoff value to ≥ 70% on MDCT to establish suspected ACS increases specificity to 88%, while maintaining sensitivity at 100%.
In addition to its added prognostic value,22 exercise echocardiography has been proposed as a useful tool in the emergency department to rule out ACS.23 Similar to the results of rest-stress myocardial perfusion imaging studies, a nonnegligible percentage of patients (10 out of 49; 20%) with a negative exercise echocardiogram had significant CAD on MDCT, although only 3 of the 49 (6.1%) patients had a final diagnosis of ACS. In our series, only 1 patient with negative MDCT and without a final diagnosis of ACS had a positive exercise echocardiogram. This shows the high specificity of a positive result on exercise echocardiography, which is superior to that obtained with stress nuclear imaging.24 However, in our study, the induction of wall-motion abnormalities on exercise echocardiography provided a level of sensitivity that was lower than previously reported levels. One of the factors that may have influenced this difference was the high percentage of patients with single-vessel disease, in which the technique has been recognized to have limited sensitivity. Finally, we did not evaluate wall motion during peak exercise, which has also been shown to improve the diagnostic sensitivity of the technique.25
In patients with acute chest pain, a balanced but robust strategy should be adopted to prevent errors in the detection of ACS, but without increasing the complexity and cost of screening. In this sense, a reasonable strategy would be to use the techniques in combination. The high sensitivity provided by MDCT is a good reason to use it in the first instance, whereas echocardiography could be reserved for those cases with anomalous or inconclusive results on MDCT, with the aim of reducing false-positive results. This strategy would significantly increase the total number of tests performed (30% according to our study), which would potentially increase the costs of the diagnostic strategy, although ACS would not be detected in a small percentage of patients (4.3% in our study). It remains to be seen whether this strategy can provide clinical benefits and advantages regarding its cost-effectiveness in clinical practice. Furthermore, MDCT does not appear to be an appropriate test in patients with known CAD or with classic contraindications such as kidney failure or atrial fibrillation, which are frequent in clinical practice and limit the applicability of the technique. Neither does MDCT seem to be an ideal test in patients with a very low probability of CAD, particularly in very young women, in whom the risk of radiation exposure exceeds the probability of having ACS.
The ROMICAT (Rule Out Myocardial Infarction Using Computer Assisted Tomography) study found that only 1 out of 31 patients with a final diagnosis of ACS had noncalcified plaque, although this important finding was not highlighted in the study. A recent study compared the Agatston score in 225 patients with chest pain in the emergency department, who had a significant (9%) prevalence of CAD on MDCT. A calcium score = 0 was found in 133 patients (59%), of whom 2 (1.5%) had significant CAD.26 There is also evidence that an Agatston score = 0 has high negative predictive value of adverse cardiac events at follow-up.27 In our series, all patients with ACS except one had an Agatston score > 0 on MDCT. The exception was a 74-year-old man with a severe lesion in the middle portion of the circumflex artery, which was not evaluable on MDCT due to the presence of a wall-motion artifact. Based on published studies, several scientific societies have suggested that an Agatston score = 0 could be sufficient to rule out ACS, particularly in patients at low pretest risk. Although the absence of coronary calcification makes ACS highly unlikely as the cause of chest pain, an Agatston score = 0 cannot definitively rule out ACS in a patient at high risk of CAD, as has sometimes been demonstrated.
LimitationsOur study has important limitations. Firstly, the patient sample was small and catheterization was not performed in all patients. Therefore, the sensitivity and specificity values reported should be taken with caution. Furthermore, as shown in Figure 1, the population was highly selected because the sample selection period was very limited and patients with a known history of heart disease and contraindications to either of the 2 tests were excluded. Both these factors would have caused selection bias. This initial pilot study was designed to highlight differences in the information provided by MDCT and exercise echocardiography. Therefore, larger randomized studies are needed to compare the safety and efficiency of both techniques. Furthermore, the results of both the MDCT and exercise echocardiogram were communicated to the medical team, which introduced a referral bias was that clearly influenced the diagnosis of ACS, since both techniques were used to assess the need for cardiac catheterization. Finally, no images were acquired during peak exercise, although these images have been shown to improve the diagnostic sensitivity of the technique.25
CONCLUSIONSMultidetector computed tomography provides better sensitivity but lower specificity than exercise echocardiography in patients attending the emergency department with chest pain, a normal electrocardiogram, negative troponins, and a low-to-intermediate probability of CAD, although the differences are not statistically significant. Thus, MDCT can be a valid alternative to exercise echocardiography in the diagnosis of ACS in this population. Given the disparity of information provided by these techniques, further prospective studies are needed to determine the clinical benefit of these techniques when used separately or in combination.
FUNDINGThis project was funded by the Fondo de Investigación Sanitaria para Evaluación de Tecnologías Sanitarias 2009 (PI 09/90513). J. Ortiz-Perez received a clinical research fellowship in 2008 from the Spanish Society of Cardiology for this study. The “Urgencias: procesos y patologías” research group is funded by the Generalitat de Catalunya (SGR 2009/1385).
CONFLICTS OF INTERESTNone declared.