To describe the epidemiological characteristics of cardiac arrests attended in basic life support units in the Basque Country (Spain) and look for factors associated with failure of cardiopulmonary resuscitation.
MethodsWe conducted an observational study during 18 months, including all out-of-hospital cardiopulmonary resuscitation provided by basic life support units. The variables defined in the Utstein-style were considered as independent and mortality as the dependent variable. We applied descriptive and analytical statistics and evaluated the magnitude of the association using a logistic regression model, which included variables with P<.05 in the bivariate analysis.
ResultsOf 1050 cardiac arrests attended, 15.7% of patients were revived in situ. The presumed etiology was cardiac in 55.3% of cases and 71.4% occurred at home. Cardiopulmonary resuscitation was started before the arrival of the ambulance in 22.9% of cases and in 18.2% the rhythm of presentation was shockable. Variables associated with lower mortality were: shockable rhythms (relative risk=0.44; P=.003), patient aged<65 years (relative risk=0.44; P=.002), time to cardiopulmonary resuscitation<8 min (relative risk=0.56; P=.039), and out-of-home events (relative risk=0.55; P=.031).
ConclusionsCardiac arrest survival was low. Cardiopulmonary resuscitation before the arrival of the ambulance was rare. A shockable rhythm, age younger than 65 years, early cardiopulmonary resuscitation efforts, and a location away from home were associated with longer survival. It is necessary to develop strategies designed to reduce ambulance response time and educate the public in basic resuscitation.
Keywords
.
INTRODUCTIONOut-of-hospital cardiopulmonary arrest (OHCA) is an important health problem because the probability of recovery is small even though the process is potentially reversible.
The exact incidence of this condition in Spain is still not known. National estimates range from 10 0001 to 50 000 events per year.2 This lack of data is due to the lack of a specific central registry and of national studies on OHCA, to the methodological limitations of the available studies, and to differences in the criteria they used to define cardiopulmonary arrest (CRA).3,4
It seems reasonable to think that OHCA survival has increased slightly since the creation of emergency medical systems (EMS).5,6 However, many variables can have an impact on the final outcome after cardiopulmonary resuscitation (CPR) maneuvers outside the hospital setting as, in addition to the way the EMS is organized, there are the intrinsic patient characteristics to consider.
In the Basque Country, patients with OHCA are attended within the EMS, essentially through the emergency deployment of life support resources. There is usually a dual response involving the closest basic life support unit (BLSU), which is composed of nonphysician health professionals (emergency technicians and/or nurses) and starts early basic CPR, followed by an advanced life support unit (ALSU), composed of physicians and nurses with more sophisticated equipment at their disposal.
The objective of this study was to describe the epidemiological characteristics of OHCA attended by the BLSU of the emergency services network in the Basque Country and to determine the factors associated with failure of CPR efforts before transfer to a hospital emergency room.
METHODSThe study sample comprised all cases of OHCA between July 1, 2009 and December 31, 2010 in which CPR was initiated by a BLSU of the emergency health transport system of the Basque Country with semiautomatic external defibrillators at their disposal (either as the only resource available or in combination with an ALSU).
The data were taken from the central OHCA database maintained by Emergentziak-Osakidetza. Entries to this database are made using the clinical information collected with a standard form by employees of the various resources integrated into the emergency network.
The independent variables included in this study were those defined in the Utstein template7: sex, age, supposed etiology of CRA, where the CRA occurred, any resuscitation attempts (such as chest compression following instructions given by telephone from the coordination center) before the arrival of the BLSU, first electrocardiographic rhythm detected, and the time from EMS activation until the start of life support measures. The dependent variable was out-of-hospital mortality after CPR measures.
Statistical AnalysisThe results of the categorical variables are expressed as absolute frequencies and percentages while quantitative variables are expressed as medians [interquartile range].
For hypothesis testing, the chi-square test, Z test, and Mann-Whitney U test were used with a 2-tailed 95% level of significance (P<.05).
The strength of the association was assessed by including variables with P<.05 in the bivariate analysis in a multivariate logistic regression model. The relative risk (RR) of CPR failure, along with the 95% confidence interval (95%CI), were calculated according to the different variables included in the model.
The analysis was performed using the PASW 17, EpiInfo 3.5.1, and Excel 2007 software packages.
RESULTSDuring the 18 months of the study period, 1272 OHCA events with resuscitation attempts were recorded in the database; in 1050 (82.5%) of these, a basic life support resource was deployed. Case details and general characteristics are shown in Figure 1. The remaining cases (222) were attended exclusively by advanced life support resources and so were excluded from this study.
CPR outside the hospital measures were successful in 15.7% of the interventions, and the patients were transferred to hospital after the ALSU had restored spontaneous circulation. Resuscitation attempts were unsuccessful in 84.3% of the OHCA events.
Of the patients attended, 64.2% were men, with a median age of 70 [25] years, and 35.8% were women, with a median age of 78 [20] years. The two groups (by sex) differed significantly in frequency (P<.001) and age (P<.001). Likewise, the median age of the patients who recovered spontaneous circulation after CPR was 65 [29.5] years, significantly younger (P<.001) than those who died at the place where they were attended (74 [23.5] years).
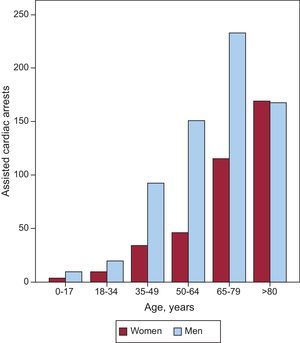
The age ranges with the most incidents were 65-79 years, with 348 (33.2%) calls, and ≥80 years, with 337 (32.2%). Twelve patients (1.1%) were under 18 years of age (Fig. 2). In this latter group, 41.7% were transported to hospital after recovery of spontaneous circulation.
Information on the most probable etiology of the CRA was not defined in 53.7% of the reports. A cardiac cause was the most commonly suspected etiology in CRA—269 (55.3%) of the entire registry—followed by respiratory conditions, with 104 events (21.4%). Trauma was responsible for 39 (8%) of the OHCA events; drowning accounted for 6 (1.2%) cases. The remaining 68 (14%) cases were due to other noncardiac etiologies.
In 71.4% of the EMS calls, the CRA was attended at home, 19.3% were attended in the public streets, and a further 9.3% in various places outside the home.
In 76.4% of the cases, a third party was present. Family members and close friends were the most frequent group of witnesses (44.1% of the arrests).
Bystanders started some type of resuscitation effort before the arrival of the first unit in 22.9% of the 981 cases in which this information was recorded.
Upon arrival of emergency services personnel, shockable electrocardiographic rhythms could be detected in 18.2% of CRA. Asystolic rhythm was the most common form of presentation (61.9%), followed by pulseless electrical activity (12.4%). Fine ventricular fibrillation (not suggestive of defibrillation) was detected as the initial rhythm in 7.4% of the cases.
The median time from EMS activation to application of the defibrillator device to the patient and the start of life support measures was 12 [8] min. This response interval was significantly lower (P<.001) when the first rhythm detected was shockable (10 [5] min) and when the CRA occurred outside the home (10 [6] min).
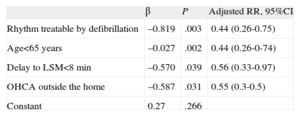
Table 1 shows the bivariate analysis of the variables associated with failure of the CPR outside the hospital measures. Table 2 shows the logistic regression model that includes the variables that achieved significance in the bivariate analysis. An initial shockable rhythm, age<65 years, delay in initiation of life support measures <8min, and CRA outside the home are associated with lower failure rates for the resuscitation measures.
General Characteristics of the Patients and Comparative Analysis According to the Immediate Outcome of the Resuscitation Measures
| Variable | Total, no. | Death, no. (%) | RSC, no. (%) | P |
| Age range | ||||
| <65 years | 363 | 284 (78.2) | 79 (21.8) | <.001 |
| ≥65 years | 685 | 599 (87.4) | 86 (12.6) | |
| Sex | ||||
| Male | 674 | 561 (83.2) | 113 (16.8) | .22 |
| Female | 376 | 324 (86.2) | 52 (13.8) | |
| Presumed etiology | ||||
| Cardiac | 269 | 200 (74.4) | 69 (25.6) | .007 |
| Extracardiac | 217 | 183 (84.3) | 34 (15.7) | |
| Place where OHCA occurred | ||||
| Home | 750 | 671 (89.5) | 79 (10.5) | <.001 |
| Outside the home | 300 | 214 (71.3) | 86 (28.7) | |
| Witnesses present | ||||
| Yes | 802 | 659 (82.2) | 143 (17.8) | <.001 |
| No | 248 | 226 (91.1) | 22 (8.9) | |
| CPR prior to EMS arrival | ||||
| Yes | 225 | 166 (73.8) | 59 (26.2) | <.001 |
| No | 756 | 657 (86.9) | 99 (13.1) | |
| First rhythm detected | ||||
| Treatable by defibrillation | 190 | 127 (66.8) | 63 (33.2) | <.001 |
| Not treated by defibrillation | 853 | 754 (88.4) | 99 (11.6) | |
| Delay between activation and start of life support | ||||
| <8 min | 137 | 100 | 37 (27%) | <.001 |
| ≥8 min | 800 | 693 (86.6) | 107 (13.4) | |
CPR, cardiopulmonary resuscitation; EMS, emergency medical system; OHCA, out-of-hospital cardiopulmonary arrest; RSC, recovery of spontaneous circulation.
In some groups, the sum might not reach the total because of missing values.
Estimate of Adjusted Relative Risk With a Binary Logistic Regression Model for the Dependent Variable “Failure of Resuscitation Measures”
| β | P | Adjusted RR, 95%CI | |
| Rhythm treatable by defibrillation | –0.819 | .003 | 0.44 (0.26-0.75) |
| Age<65 years | –0.027 | .002 | 0.44 (0.26-0-74) |
| Delay to LSM<8 min | –0.570 | .039 | 0.56 (0.33-0.97) |
| OHCA outside the home | –0.587 | .031 | 0.55 (0.3-0.5) |
| Constant | 0.27 | .266 |
95%CI, 95% confidence interval; LSM, life-support measures; OHCA, extrahospital cardiopulmonary resuscitation; RR, relative risk.
Only those variables that retained significance are shown.
Based on the consideration that the data source for OHCA used for this study considers all resuscitations performed by emergency health resources in the Basque Country, the ratio of OHCA cases of any etiology attended during the study period (1272) and the resident population in this autonomous community, it is possible to calculate an approximate incidence of 3.9 (95%CI, 3.6-4.2) events per 10000 inhabitants or 18400 cases per year if the data were extrapolated to the entire Spanish population.
However, the latter assumption should be treated with particular care and awareness of the huge sociodemographic differences between different regions of Spain. Other authors have reported regional incidences of between 2 and 5 events per 10 000 inhabitants,8–11 which is close to the figure reported in our study.
Immediate survival after resuscitation techniques was 15.7% in our series, which is significantly lower than the recovery rates published in studies of other Spanish regions12 or those published for the United States of 27.4% (95%CI, 26.9%-27.9%).13 These differences can be attributed to differences in several factors,12 such as EMS response times, characteristics of the population, and idiosyncrasies in EMS organization, among others.
The higher proportion of men in our study (64.1% compared to 35.9% women) is in agreement with most other studies.10,13,14 Some recent studies have even pointed to a possible hormonal protective factor in women,15 which would support the lower incidence of OHCA events of cardiac etiology in premenopausal women.
Unlike other isolated studies (which report advantages for men8,14 or for women10,16,17), in the present study sex is not independently associated with acute survival after CPR.
The highest incidence of CRA occurred in individuals in their 80s and 90s: a noteworthy increase in OHCA cases was observed beyond 65 years of age, in line with most published studies. Age less than 65 years was associated with lower failure rate of out-of-hospital resucitation (RR=0.44). This study shows, once more, the association between advanced age and comorbidities, particularly those of cardiovascular origin.18
The available information on the most likely cause of the CRA (in the opinion of the emergency team) was not contained in the Utstein template in slightly over half the cases attended. This is the field that is most often left blank in the OHCA report, perhaps because of the difficulty healthcare professionals have in determining the probable etiology.
Nevertheless, 55.3% of the cases with a probable cause recorded had a cardiogenic etiology listed as the likely cause for the CRA. This percentage is well below the figures reported in Spanish studies12 and international studies,19,20 where it is usually above 75% of all cases, although rates of around 60%, closer to those observed in our community, have been reported more recently.21
Such a difference could be explained, at least partially, by a possible bias by the healthcare team in classifying the cause of the CRA. While noncardiac causes (especially trauma, drowning, or poisoning) are usually clearly identifiable even by nonhealthcare professionals, cardiopathic causes are more subtle in terms of presentation, and diagnosis of such etiologies as the cause for sudden death may be difficult to make. Therefore, it may be that most of the cases in which the etiologic cause is not indicated may in fact be a CRA of cardiac origin.
It has been reported that most cases of OHCA occur at the patient's residence and that the mortality associated with OHCA is higher in the home than in other places.22,23
Several factors, such as longer response times of the emergency services, may be responsible for the higher home mortality, and these should be studied more closely.22,23 We also should not forget that most situations in which resuscitation measures are attempted when they are not indicated because of their supposed futility (terminal patients, poor quality of life, etc.) more often occur at home. This is conditioned by the fact that the first resource to arrive on the scene is usually a BLSU. The ethical dilemma of not initiating CPR or initiating it while an ALSU awaits authorization by telephone from the emergency coordination center to then stop the measures could be resolved by implementing protocols that determine whether resuscitation is appropriate for patients receiving CRA in an out-of-hospital setting.24 In addition, this is an aspect that is not contemplated in the Ustein template, which could replicate this bias in other similar epidemiologic studies.10
The presence of bystanders and their ability identify CRA are variables to be taken into account when the out-of-hospital outcomes are assessed, in particular because they will have an impact on the time-to-intervention in the survival chain. A relevant aspect highlighted by this study is that, even though a bystander was present in more than 75% of the cases of CRA, few attempts were made to initiate an attempt at CPR prior to the arrival of the first responders. Nonetheless, these factors did not have a statistically significant effect on the final outcome.
Electrocardiographic rhythms were identified, and classified according to medical criteria, from electronic records extracted from the defibrillator after use. Asystolic rhythm was the most frequently detected rhythm after application of a semiautomatic external defibrillator. It is also noteworthy that very few patients had coarse ventricular fibrillation (ie, suitable to defibrillation). The 18.2% rate we observed is among the lowest of the studies reviewed.12 This simply confirms that the longer the response time, the lower the probability of finding the patient in fibrillation. The presence of a shockable rhythm when the first responders arrive is the predictive variable most strongly associated with survival after attempts at resuscitation (RR=0.44). This underscores the need to devise strategies aimed at reducing the response time before application of a semiautomatic external defibrillator.
The response time of the emergency units is among the main parameters for assessing EMS performance. In addition, the data quality is very attractive because these times are very easy to measure.
For the purposes of this study, we chose “time-to-activation of EMS-start of life support measures” as the most accurate (the times of each action are automatically recorded) and the most relevant from a clinical point of view.25 This period covers the time from receipt of the call in the emergency coordination center to the time of diagnosis of CRA, placing the defibrillator, and initiating life support. The delay will therefore include the time used to process the call, activate the emergency units, and reach the patient.
With regard to this variable, and as might be expected, a clear relationship was observed between early action and the final outcome of the resuscitation measures, with values close to those reported by other authors.9,26 However, from the clinical perspective, the response times obtained are longer than is desirable.
Finally, and in view of the outcomes obtained, it may be necessary to consider, on the one hand, strategies aimed at reducing response times in CRA cases, given that this is a key factor in the outcomes of CRA measures, and on the other, the implementation of effective training programs on resuscitation techniques among the target population.
LimitationsThis study is subject to a series of methodological limitations. First is the lack of clinical data on OHCA assisted by an ALSU as the only resource at the site. However, given that the criteria for not activating a BLSU along with an ALSU in the face of CRA (within the “dual response” strategy) are purely logistical (such as not having an emergency resource available close to the site) and nonclinical, it seems reasonable to assume that the sample used is representative.
There is also a lack of follow-up of resuscitated patients, and outcomes after transfer to hospital are not known. These gaps in information are a reflection of the difficulties faced by the basic life support resources in accessing data.
Likewise, there is no record of the quality of the CPR administered, whether by bystanders or by the care team. Similarly, no data are available on the time elapsed between the patient's loss of consciousness and activation of the EMS, or from the start of resuscitation measures by the BLSU and arrival to the ALSU. Both aspects, which can be overcome through the design of new prospective studies, could be of great interest as they would partially extend the results obtained.
CONCLUSIONSThe findings of this study show that the chances of surviving CRA in the Basque Country are low and that CPR is very seldom attempted prior to arrival of the ambulance. A shockable rhythm, age<65 years, early initiation of life support measures, and occurrence at a site outside the home were associated with increased survival until transfer to hospital.
In addition, the findings of the present study highlight the need to strive to create strategies aimed at reducing EMS response time and informing the general population of basic resuscitation techniques.
CONFLICTS OF INTERESTNone declared.
We thank all members of the basic life support resources in the network of emergency transport of the Basque Country (Red Cross, DYA [Detente y Ayuda], Transporte Sanitario Bizkaia, Ambulancias Euskadi, Larrialdiak, Gipuzkoa Emergentziak and Ambulancias Gipuzkoa) for their cooperation in collecting and sending the data, and to Emergentziak Osakidetza for providing us with access.