Cardiac rehabilitation programs (CRP) are a set of interventions to improve the prognosis of cardiovascular disease by influencing patients’ physical, mental, and social conditions. However, there are no studies evaluating the optimal duration of these programs. We aimed to compare the results of a standard vs a brief intensive CRP in patients after ST-segment elevation and non–ST-segment elevation acute coronary syndrome through the Más por Menos study (More Intensive Cardiac Rehabilitation Programs in Less Time).
MethodsIn this prospective, randomized, open, evaluator-blind for end-point, and multicenter trial (PROBE design), patients were randomly allocated to either standard 8-week CRP or intensive 2-week CRP with booster sessions. A final visit was performed 12 months later, after completion of the program. We assessed adherence to the Mediterranean diet, psychological status, smoking, drug therapy, functional capacity, quality of life, cardiometabolic and anthropometric parameters, cardiovascular events, and all-cause mortality during follow-up.
ResultsA total of 497 patients (mean age, 57.8±10.0 years; 87.3% men) were finally assessed (intensive: n=262; standard: n=235). Baseline characteristics were similar between the 2 groups. At 12 months, the results of treadmill ergometry improved by ≥ 1 MET in ≥ 93% of the patients. In addition, adherence to the Mediterranean diet and quality of life were significantly improved by CRP, with no significant differences between the groups. The occurrence of cardiovascular events was similar in the 2 groups.
ConclusionsIntensive CRP could be as effective as standard CRP in achieving adherence to recommended secondary prevention measures after acute coronary syndrome and could be an alternative for some patients and centers.
Registered at ClinicalTrials.gov (Identifier: NCT02619422).
Keywords
Health care advances in the field of acute coronary syndrome (ACS) have substantially changed its prognosis.1 However, atherosclerotic cardiovascular disease remains the leading cause of death in western countries.2 After a first myocardial infarction, the risk of new cardiovascular events remains high because of additional risk factors, among other aspects.3
In this setting, adequate secondary prevention measures are essential to reduce the social, personal, and economic burden of cardiovascular disease. Of note, many coronary patients are young and have an active professional life.4
Cardiac rehabilitation programs (CRP) have been shown to have a positive effect on cardiovascular risk factors and quality of life, leading to a lowered risk of recurrence after an infarction.5,6
Unfortunately, only a low percentage of coronary patients follow a CRP.7,8 In fact, recent data from the EUROASPIRE V survey show that in Europe only 31.8% of patients with coronary heart disease and indications for CRP are enrolled in these programs. It is clear that the implementation of the CRP must be improved in our setting.9
Although the duration of standard CRPs is 8 to 12 weeks’ duration, the optimal duration and type of CRP for obtaining the long-term benefits of healthy lifestyle patterns and the impact of these programs on cardiovascular outcomes remain unknown.10–12
Shorter protocols have been proposed that would allow CRPs to be attended by some patients, who otherwise would find it difficult to do so due to time restrictions, work, and family responsibilities. Similarly, such protocols would allow health centers to perform individualized CRP, which otherwise could be hindered by logistical difficulties, space issues, care burden, and so on. In this line, the results of some studies on 2-week CRPs only found improvements in exercise capacity and substitute variables, such as oxidative stress and inflammatory markers; however, these studies did not directly compare their results with those of standard programs of longer duration.13–15
Consequently, the primary objective of this study was to analyze whether an intensive CRP (2 weeks with booster sessions) could improve adherence to physical activity, the Mediterranean diet, smoking cessation, and the use of medical treatments as recommended in the guidelines as a standard CRP (8 weeks). The secondary objective was to analyze its impact on quality of life, psychological state (anxiety and depression), and cardiovascular results at 1 year.
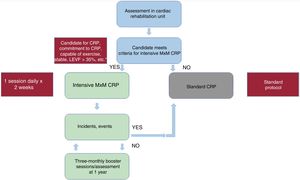
METHODSDesignWe conducted a prospective, randomized, open, blinded endpoint (PROBE design) multicenter trial. This type of design tends to minimize evaluation bias. The study included patients who were 18 years or older, had been diagnosed with ST-segment elevation ACS or non–ST-segment elevation ACS 2 months before the initial visit, and had sufficient cognitive ability to understand educational workshops, were physically capable of exercising, and were prepared to give written informed consent. The study excluded patients with left ventricular ejection fraction of 35% or less, New York Heart Association (NYHA) III-IV functional class, refractory angina, or contraindications for physical activity.
Given that the effect of shorter-term intensive CRPs remains unknown, we initially calculated a sample size of 600 patients, which is the approximate number of post-ACS patients who are referred to the cardiac rehabilitation units of all the participating centers over 12 months. Subsequently, using data from a pilot study conducted at the La Paz University Hospital, a blinded independent statistician reviewed the results obtained and the sample size was recalculated to 500. A 0.025 confidence level and a power of more than 80% would allow analyses that would demonstrate differences between groups in exercise adherence, which would be assessed using the metabolic equivalent of task (MET) value on stress testing and the dietary survey. There were very few differences between groups in relation to the drugs administered to them, and so a much larger sample size than that initially estimated would be required to detect any potential differences. Clinical events were rare, and thus the study did not have sufficient statistical power to detect any differences related to them.1,15
A centralized automated 24-hour interactive voice response system was used to randomly assign patients to the intensive and control (standard) groups.
Between October 2015 and December 2016, consecutive patients were selected from 8 cardiac rehabilitation units. The study was approved by the Clinical Research Ethics Committee of the Hospital Universitario La Paz and supported by the local ethics committees of the participating centers. All patients gave their written informed consent. The study is registered with ClinicalTrials.gov (Identifier: NCT02619422).
The complete study protocol and the specific outcome variables have been previously published.16 In summary:
- •
The control CRP comprised 8 weeks of 3 supervised training sessions per week using a treadmill or exercise bike (5-minute warm-up, 35-minute moderate aerobic physical activity [Borg scale 13-15], 5-minute cool-down, and 15-20minutes of moderate-intensity dynamic isotonic exercises). This group of participants attended a total of 24 sessions. In addition, recommendations for outpatient physical exercise were given to the patients in scheduled sessions 3 times per week, and information on the disease and secondary prevention was given to them and their families once per week. The following topics were discussed in the workshops: tobacco use, Mediterranean diet, physical activity, cardiovascular risk factors, pharmacological treatment, emotional stress, erectile dysfunction, and psychological support. Finally, the patients underwent standard follow-up and were assessed at 1 year.
- •
The intensive CRP comprised 2 weeks of the same supervised training sessions, which were scheduled in 10 sequential sessions. Educational workshops were given to this group 30minutes before training. The educational booster workshops were conducted at 3, 6, and 9 months with the aim of improving adherence with secondary prevention measures through working groups coordinated by a nurse and a physical therapist with experience. This group of participants attended 10 training sessions and 3 booster sessions. These patients were assessed at 1 year.
At the initial visit, all participants underwent a baseline medical evaluation that included a review of drug therapy, anthropometric measurements, and laboratory parameters (hemoglobin, total cholesterol, low-density lipoprotein cholesterol [LDLc], high-density lipoprotein cholesterol [HDLc], triglycerides, kidney function [MDRD-4],17 and glycohemoglobin [HbA1c]). CO-oximetry testing was also performed.18 Functional capacity was quantified using the Bruce ramp protocol (MET). Finally, the patients completed the modified Trichopoulou questionnaire on adherence to the Mediterranean diet,19 the Beck Depression Inventory20 and the State-Trait Anxiety Inventory (STAI)21 to assess psychological status, and the EQ-ED-5L to measure health-related quality of life.22
Follow-up and definitionsA final visit was performed 1 year after the initial visit (randomization). We evaluated the same parameters as before and recorded cardiovascular events (stroke, nonfatal myocardial infarction, new revascularization), cardiovascular mortality, and all-cause mortality. Baseline body weight, waist circumference, lipid profile, and HbA1c values were compared with those at the end of the study. Patients were considered to be adherent to physical activity when they improved by at least 1 MET on stress testing at 12 months vs baseline values and to have quit smoking when CO-oximetry values were between 0ppm and 6ppm at 12 months.18 Adherence to the Mediterranean diet was defined as a score of 9 or more on the modified Trichopoulou questionnaire at 12 months.19 Adherence to cardiac drug therapy23 was defined as the ongoing use of the 4 main groups of cardiac therapies (aspirin, a second antiplatelet drug, beta-blockers, and statins) at 12 months.
At the beginning and end of the study, we compared the percentage of patients with a score of less than 14 on the Beck Depression Inventory, the percentages of patients with a score of more than 5 on the STAI,21 and their scores on the EQ-ED-5L. We also measured time to return to work after ACS.
Statistical analysisStatistical analyses were conducted with the SPSS 23.0 software package (SPSS, United States). Continuous variables are expressed as mean ± standard deviation and qualitative variables as absolute numbers and percentages. Means were compared using the Student t test or the Mann-Whitney U test as appropriate. Categorical variables were compared using the chi-square test or Fisher exact test as applicable. The analysis was conducted on an intention-to-treat basis, because the main objective was to compare the effect of an intensive vs standard CRP in terms of adherence to secondary prevention measures at 12 months. Analysis of variance (ANCOVA) was used to determine differences between baseline variables and those at 12 months. The fixed variable was the group (control or experimental) and the observed value was covariance. A 2-tail P-value of .05 or less was used as a cutoff for statistical significance.
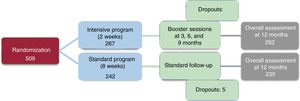
RESULTSThe study initially included 509 patients with ST-segment or non–ST-segment elevation ACS. However, 12 patients were excluded from the study because they did not complete the CRP: 7 were initially assigned to the standard arm and 5 to the intensive arm. Thus, a total of 497 patients were finally assessed (262 in the intensive group and 235 in the standard group) (figure 1).
table 1 shows the baseline clinical characteristics of the patients. The mean age of the participants was 58 years, and most were men (87.3%). In total, 50% of the participants had ST-segment elevation ACS. Mean LVEF was 56%. A high percentage of participants had cardiovascular risk factors, with dyslipidemia (65.2%) and hypertension (48.5%) being the most common. There were no statistically significant differences between groups in their baseline demographic characteristics and risk profiles.
General characteristics of the study participants stratified by assigned rehabilitation group
| Variable | Total (n = 497) | Intensive (n = 262) | Standard (n = 235) | P |
|---|---|---|---|---|
| Demographic data | ||||
| Age, y | 57.8 ± 10.0 | 57.4 ± 9.8 | 58.1 ± 10.2 | .433 |
| Men | 434 (87.3) | 226 (86.3) | 208 (88.5) | .494 |
| Educational level | .308 | |||
| None | 18 (3.7) | 9 (3.5) | 9 (3.9) | |
| Primary | 178 (36.7) | 96 (37.6) | 82 (35.7) | |
| Secondary | 186 (38.3) | 104 (40.8) | 82 (35.7) | |
| University | 103 (21.3) | 46 (18) | 57 (24.8) | |
| Active workers | 243 (48.9) | 133 (50.7) | 110 (46.8) | .485 |
| Physical examination | ||||
| Weight, kg | 81.5 ± 13.6 | 81.1 ± 13.2 | 81.7 ± 13.9 | .612 |
| Waist circumference, cm | 100.5 ± 10.3 | 99.8 ± 10.0 | 101.2 ± 10.4 | .128 |
| Cardiovascular risk factors | ||||
| Dyslipidemia | 324 (65.2) | 168 (64.1) | 156 (66.4) | .638 |
| Hypertension | 241 (48.5) | 118 (45.0) | 123 (52.3) | .107 |
| Sedentary lifestyle | 203 (40.8) | 107 (40.8) | 96 (40.9) | 1.0 |
| Smokers | 109 (21.9) | 58 (22.1) | 51 (21.7) | .243 |
| Diabetes mellitus | 103 (20.7) | 50 (19.1) | 53 (22.6) | .375 |
| Clinical presentation | ||||
| ST-elevation acute myocardial infarction | 249 (50.1) | 121 (46.2) | 128 (54.5) | .073 |
| LVEF, % | 56.3 ± 9.0 | 56.6 ± 8.4 | 55.9 ± 9.5 | .395 |
| Biochemical parameters | ||||
| Hemoglobin, g/dL | 16.0 ± 14.2 | 15.3 ± 10.9 | 16.7 ± 17.0 | .269 |
| Total cholesterol, g/dL | 145.7 ± 41.9 | 143.8 ± 38.6 | 147.8 ± 45.3 | .299 |
| HDLc, g/dL | 39.1 ± 11.9 | 39.4 ± 12.6 | 38.8 ± 11.1 | .570 |
| LDLc, g/dL | 85.3 ± 36.7 | 83.7 ± 34.5 | 87.0 ± 39.0 | .328 |
| Triglycerides, g/dL | 126.4 ± 66.2 | 123.9 ± 66.5 | 129.2 ± 65.9 | .371 |
| Kidney function-MDRD-4, mL/min | 76.4 ± 28.5 | 76.3 ± 28.4 | 76.4 ± 28.6 | .965 |
| HbA1c,% | 6.0 ± 1.1 | 6.0 ± 1.1 | 6.0 ± 1.1 | .809 |
| EQ-5D-5L, Mediterranean diet, Beck Depression Inventory, STAI score | ||||
| EQ-5D-5L | 70.1 ± 17.5 | 70.1 ± 16.9 | 70.1 ± 18.2 | .981 |
| Mediterranean diet ≥ 9 | 313 (63.0) | 164 (62.6) | 149 (63.4) | .489 |
| Beck Depression Inventory | .761 | |||
| < 14 | 388 (82.0) | 199 (80.6) | 189 (83.6) | |
| 14-19 | 44 (9.2) | 24 (9.7) | 20 (8.9) | |
| 20-28 | 27 (5.8) | 15 (6.1) | 12 (5.3) | |
| ≥ 29 | 14 (3.0) | 9 (3.6) | 5 (2.2) | |
| STAI > 5 (state) | 273 (57.7) | 146 (59.4) | 127 (56.0) | .458 |
| STAI > 5 (trait) | 216 (45.7) | 112 (45.5) | 104 (45.8) | 1.0 |
| Medication prescribed at the beginning of the study | ||||
| Aspirin | 492 (99.0) | 258 (98.5) | 234 (99.6) | .376 |
| P2Y12inhibitors | 477 (96.0) | 251 (95.8) | 226 (96.2) | 1.0 |
| Beta-blockers | 432 (86.9) | 232 (88.5) | 200 (85.1) | .287 |
| Statins | 470 (94.6) | 250 (95.4) | 220 (93.6) | .431 |
| Other lipid-lowering drugs | 51 (10.3) | 26 (9.9) | 25 (10.6) | .883 |
HBA1c, glycohemoglobin; HDLc, high-density lipoprotein cholesterol; LDLc, low-density lipoprotein cholesterol; LVEF, left ventricular ejection fraction.
Values are expressed as No. (%) or mean ± standard deviation.
There were also no significant differences between the 2 groups in their biochemical parameters, the EQ-5D-5L quality of life questionnaire, Mediterranean diet, Beck Depression Inventory and STAI scores at the beginning of the study, or in cardiac therapies, antiplatelet agents, beta-blockers, lipid-lowering drugs, and the different groups of cardiac drug therapies, which were prescribed in similar numbers between the 2 groups (table 1).
After a mean follow-up of 11.8 ± 2.9 months, both CRPs improved adherence to most of the predefined secondary prevention measures (table 2). Regarding physical activity, at 12 months, the results of stress testing improved by at least 1 MET in 129 patients (94.2%) in the intensive group and 120 (93.0%) in the standard group (P=.80). There were no significant differences between groups in the other parameters (eg, diet, quitting smoking, weight, abdominal circumference, quality of life, depression, and anxiety). During the study period, there were similar changes in medication in both groups. At 12 months, 39.3% of patients in the intensive group and 38.7% of those in the standard group were taking 4 groups of cardiac medications (P2Y12 inhibitors were discontinued at the end of the study in 49.2% and 50.2% of the patients, respectively).
Changes in the parameters assessed in the MxM trial by assigned rehabilitation group
| Variable | Intensive (n = 262) | Standard (n = 235) | Difference intensive vs standard | |||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Final | P | Baseline | Final | P | Absolute difference | P | |
| Physical examination | ||||||||
| Weight, kg | 81.1 ± 13.2 | 81.3 ± 13.7 | .864 | 81.7 ± 13.9 | 80.9 ± 13.0 | .519 | 0.2 vs –0.8 | .59 |
| Waist, cm | 99.8 ± 10.0 | 99.2 ± 10.0 | .492 | 101.2 ± 10.4 | 99.6 ± 9.8 | .086 | –0.6 vs –1.6 | .22 |
| CO-oxymetry, 0-6 ppm | 167 (88.4) | 152 (85.4) | .227 | 136 (85.5) | 129 (86.0) | .774 | –3.0 vs –0.5 | .425 |
| Biochemical parameters | ||||||||
| LDLc, g/dL | 83.7 ± 34.5 | 73.0 ± 24.0 | < .001 | 87.0 ± 39.0 | 69.2 ± 19.9 | < .001 | –10.7 vs –17.7 | .026 |
| HDLc, g/dL | 39.4 ± 12.6 | 44.7 ± 10.9 | < .001 | 38.8 ± 11.1 | 44.0 ± 12.2 | < .001 | 5.3 vs 5.2 | .953 |
| Triglycerides, g/dL | 123.9 ± 66.5 | 114.6 ± 56.9 | .086 | 129.2 ± 65.9 | 115.7 ± 68.4 | .029 | –9.3 vs –13.5 | .630 |
| HBA1c,% | 6.0 ± 1.1 | 5.8 ± 0.7 | .022 | 6.0 ± 1.1 | 5.9 ± 0.9 | .255 | –0.2 vs –0.1 | .598 |
| Functional capacity | ||||||||
| MET ≥ 1 | - | 129 (94.2) | - | - | 120 (93.0) | - | 94.2 vs 93.0 | .804 |
| MET > 2 | - | 84 (37.2) | - | - | 85 (44.5) | - | 37.2 vs 44.5 | .134 |
| Questionnaires | ||||||||
| EQ-5D-5L | 70.1 ± 16.9 | 76.9 ± 15.8 | < .001 | 70.1 ± 18.2 | 78.0 ± 15.8 | < .001 | 6.9 vs 7.9 | .834 |
| Mediterranean diet > 7 | 188 (75.2) | 203 (91.0) | < .001 | 173 (75.5) | 188 (96.9) | < .001 | 15.8 vs 21.4 | .017 |
| Mediterranean diet ≥ 9 | 164 (62.6) | 190 (85.2) | < .001 | 149 (63.4) | 174 (89.7) | < .001 | 19.6 vs 24.6 | .138 |
| Increment ≥ 1 point | - | 135 (60.8) | - | - | 144 (75.0) | - | 60.8 vs 75.0 | .002 |
| Increment ≥ 1 point | - | 100 (45.0) | - | - | 111 (57.8) | - | 45.0 vs 57.8 | .010 |
| Beck Depression Inventory <14 | 199 (80.6) | 181 (81.2) | .906 | 189 (83.6) | 166 (86.0) | .586 | 0.6 vs 2.4 | .446 |
| STAI > 5 (state) | 146 (59.4) | 119 (53.1) | .192 | 127 (56.0) | 86 (45.0) | .030 | –6.3 vs –11.0 | .109 |
| STAI > 5 (trait) | 112 (45.5) | 93 (41.6) | .402 | 104 (45.8) | 69 (36.1) | .046 | –3.9 vs –9.7 | .029 |
| Pharmacological treatment | ||||||||
| Aspirin | 258 (98.5) | 232 (88.5) | < .001 | 234 (99.6) | 209 (88.9) | < .001 | –10.0 vs –10.7 | .882 |
| P2Y12 inhibitors | 251 (95.8) | 122 (46.6) | < .001 | 226 (96.2) | 108 (46.0) | < .001 | –49.2 vs –50.2 | .857 |
| Beta-blockers | 232 (88.5) | 205 (78.2) | .002 | 200 (85.1) | 171 (72.8) | .001 | –10.3 vs –12.3 | .481 |
| Statins | 250 (95.4) | 231 (88.2) | .003 | 220 (93.6) | 198 (84.3) | .001 | –7.2 vs –9.3 | .417 |
| Other lipid-lowering drugs | 26 (9.9) | 46 (17.6) | .015 | 25 (10.6) | 48 (20.4) | .004 | 7.7 vs 9.8 | .426 |
HBA1c, glycohemoglobin; HDLc, high-density lipoprotein cholesterol; LDLc, low-density lipoprotein cholesterol; LVEF, left ventricular ejection fraction; MET, metabolic equivalents; MxM, MxM cardiac rehabilitation program.
Values are expressed as No. (%) or mean ± standard deviation.
Table 2 shows the study variables by group.
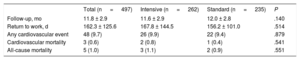
During follow-up, 48 patients (9.7%) had a new cardiovascular event: 9.9% in the intensive group and 9.4% in the standard group (P=.879). Cardiovascular death and all-cause mortality occurred in 0.6% and 1.0% of patients, respectively, with no significant differences between groups. Patients from both groups returned to work after similar periods of time (table 3).
Events during follow-up and return to work activity
| Total (n = 497) | Intensive (n = 262) | Standard (n = 235) | P | |
|---|---|---|---|---|
| Follow-up, mo | 11.8 ± 2.9 | 11.6 ± 2.9 | 12.0 ± 2.8 | .140 |
| Return to work, d | 162.3 ± 125.6 | 167.8 ± 144.5 | 156.2 ± 101.0 | .514 |
| Any cardiovascular event | 48 (9.7) | 26 (9.9) | 22 (9.4) | .879 |
| Cardiovascular mortality | 3 (0.6) | 2 (0.8) | 1 (0.4) | .541 |
| All-cause mortality | 5 (1.0) | 3 (1.1) | 2 (0.9) | .551 |
Values are expressed as No. (%) or mean ± standard deviation.
This is the first randomized study with a sufficient number of patients to analyze the feasibility and multilevel results of an intensive CRP vs standard CRP.
Several studies have clearly demonstrated the benefits of CRPs in the secondary prevention of ischemic heart disease by modifying the control of cardiovascular risk factors and promoting healthy lifestyle changes.2,11,12
However, depending on the target population, current rehabilitation protocols need to be improved and updated. They should be more cost-effective, more patient-centered, and provide more comprehensive secondary prevention.24
One of the key parameters of CRPs is their optimal duration, yet few studies have assessed this aspect. Current CRPs vary in their duration from 8 to 12 weeks: however, in practice, their duration is based more on habit than on a high-level evidence.10,25,26 As a result, it remains unclear which is the best model for current CRPs.11,12,27
In line with the results of most cardiac rehabilitation studies, the present study shows that, in general, CRPs improve functional capacity, quality of life, and adherence to the Mediterranean diet, effectively reduce LDLc levels, and are associated with low rates of cardiovascular events and death.2,5,6,11,15 However, the results of the present study, which included 500 patients with previous ACS, showed that an intensive short CRP can be as effective as standard CRP. This favorable result may be due to the use of booster sessions after the main intensive CRP had been completed as well as stricter patient follow-up.
The foregoing aspects are of relevance, because fewer patients have been included in the small number of previous studies on the impact of CRP duration on efficacy parameters, thus making it difficult to realistically compare many of the relevant parameters.10,28
In this study, the mean age of the participants was 58 years, 87% were men, and 49% were in active employment. These characteristics are also in line with those described in previous studies, which have shown that many of the patients who undergo CRP are relatively young and have work commitments.29,30
Thus, taking into account that many patients participating in CRPs have a limited period of sick leave, which may hinder adherence to programs, a short intensive protocol could be of benefit to many of them.
Although body weight and abdominal circumference remained stable in our participants, there were improvements in LDLc, HDLc, and triglyceride levels in both groups. Similar results have been obtained in previous studies.10,28 However, if we consider the results of our study and those conducted in other European countries8,31 it is clear that more efforts are needed to promote body weight reduction among overweight patients and to improve lipid control.8,31
Regarding physical activity, at 12 months, the results of final stress testing improved by at least 1 MET in most patients (more than or equal to 93%), without significant differences between the groups. Previous studies have also shown that cardiac rehabilitation improves functional capacity.10,27,28,32 Studies have investigated whether cardiorespiratory fitness in patients undergoing CRP can be improved by high-intensity interval training vs moderate-intensity continuous training.33,34
The Mediterranean diet should be promoted as an objective of secondary prevention,9 as shown by the results of the PREDIMED study, which demonstrated the benefits of the Mediterranean diet in lowering the incidence of major cardiovascular events.35 In our study, both groups significantly increased their adherence to the Mediterranean diet, although adherence was higher in the standard CRP group.
Regarding tobacco use, several studies have found a significant prevalence of persistent smoking after a heart attack, reaching 55% in the EUROASPIRE V survey.8,10 Regardless of group, there was a higher rate of smoking cessation among our patients than among those in previous studies. This is a highly relevant finding, because the benefits of many treatments could be reduced or even suppressed in persistent smokers.13,14
In areas such as health-related quality of life, several studies have also demonstrated the beneficial effects of CRP.5,10,32,36 The results of the present study are similar and suggest that benefits could be independent of CRP duration.
Patients with cardiovascular disease frequently experience depression and anxiety, which could be associated with worse prognosis. Thus, depression and anxiety and their severity should be investigated in this population.37 Previous studies have shown that CRP can improve psychological aspects.10,38 Nevertheless, we found that there were no significant changes in scores on the Beck Depression Inventory, there were significant improvements in scores only in the standard CRP group on the STAI, and there was a nonsignificant trend in the intensive CRP group on the STAI.
Regarding prognosis, some studies have shown that a minimum of 25 to 36 cardiac rehabilitation sessions are needed to reduce mortality or a minimum of 36 such sessions to reduce the number of percutaneous coronary interventions,12,39,40 whereas other studies have found benefits regardless of CRP duration.41 Our study suggests that similar benefits could be obtained with an intensive protocol vs a standard one, taking into account the aforementioned lack of statistical power to detect differences in cardiovascular events. figure 2 shows a flowchart for patients candidate for a CRP depicting a protocol similar to that used in the MxM (Más por Menos) study.
This study has several limitations and thus its results should be interpreted with caution and mainly used as hypothesis generators. On the one hand, during the first year after an acute cardiovascular event, patients may be more receptive and willing to change their lifestyle to avoid a new event. The EUROASPIRE V survey showed that patients become less adherent over time, and so it would be optimal to reassess them 2 to 3 years after the initial event. On the other hand, although the study included almost 500 patients who had a relatively well-matched clinical profile, this sample size may have been insufficient to detect differences between the groups, especially in relation to infrequent events or changes in treatment. Thus, although multiple comparisons may be informative, they should be interpreted with caution. The fact that the patients were specially selected may have strongly increased their motivation to adhere with the treatments: thus, the results cannot be extrapolated to a general population with ACS.
However, the favorable preliminary results of this study show that intensive CRP is feasible in our setting. Larger studies should be conducted with adequate statistical power, especially in relation to hard clinical variables.
In a recent study conducted in Portugal, Araújo et al.42 found an inverse association between the European Society of Cardiology Acute Cardiovascular Care Association quality indicators, including CRP, for acute myocardial infarction and crude 30-day mortality for both sexes. Therefore, in our setting, the implementation of CRPs should also be improved. Despite the previously mentioned limitations, the results of this study support the implementation of intensive programs for patients who, due to their clinical, personal, family, social, or professional characteristics, are unable to attend long-term programs. Furthermore, intensive programs can improve quality standards in hospitals that are unable to serve more patients due to limited resources and may represent a cost-effective alternative to standard CRP.
CONCLUSIONSIntensive or standard CRPs are effective in increasing adherence to secondary prevention measures at 1 year. Both programs led to improved smoking cessation rates, adherence with the Mediterranean diet, functional capacity, quality of life, and LDLc control. Therefore, intensive CRPs could be an alternative in selected patients and hospitals.
FUNDINGUnconditional grant from Menarini.
CONFLICTS OF INTERESTNone declared.