Evidence-based medicine (EBM), the paradigm of modern medicine, began at the end of the last century at McMaster University in Canada, with the aim of progressing from the empiricism that had dominated medicine until the 1980s and decision-making overly based on individual doctors’ habits and experience.1,2 There are many definitions of EBM, but all can be summarized by the concept of acting and making decisions based on existing evidence, making it a process in pursuit of the best scientific arguments to solve the problems encountered in everyday clinical practice. In other words, the conscious, clear and sensible use of the best evidence available in making decisions on the care of the individual patient.3 EBM has been a major advance in the practice of medicine but has several important limitations. First, with the sheer quantity of information available, at least in some areas such as heart failure (HF)— hundreds and thousands of studies and publications that are added almost daily to the knowledge base—it is impossible to read, analyze, and evaluate such a volume of data. In addition, not all the evidence is of equal value; at the peak of this hierarchy are clinical trials and meta-analyses, which are also abundant and, at times, report contradictory results. This has led to the need for information summaries, the most widely consulted being the clinical practice guidelines (CPGs) issued by the various scientific societies.4,5 In fact, these guidelines have become the new “textbooks”, replacing the classical medical tomes.
However, CPGs also have their limitations. Although they use objective criteria to review and assess the selected information, they are drafted by a group of experts, appointed by scientific societies, which could introduce personal biases in the final drafting of the guidelines and their recommendations. In fact, this led the Spanish Society of Cardiology to create a Clinical Practice Guidelines Committee that critically appraises each CPG issued by the European Society of Cardiology (ESC) and publishes the conclusions of their analysis.6,7 Secondly, a large part of the recommendations in CPGs are based on the consensus of the experts drafting them (evidence level C), if there are no well-controlled studies on the subject. This is not a criticism, as EBM involves not only the information available in the literature but also clinical judgement, to tailor the best evidence available to solving the specific clinical problems posed by our patients in day to day practice3; this requires diagnostic skills, in which a key role is played by experience (the “clinical eye”) and the ability to evaluate the individual characteristics of each patient before making a decision (extrapolating the general recommendations of the CPGs, based on studies that include patients with particular characteristics, to our individual patients). Thirdly, CPGs are drafted and published at certain intervals, usually every 4 to 5 years in the case of the ESC, which means that new published evidence is not added to the official recommendations quickly enough, raising doubts and discussion about whether or not to incorporate new evidence into our daily practice. The societies issuing CPGs have tried to address this problem by publishing updates on specific aspects of strong interest before the new general revision of CPGs.8 Last, but to my mind not least, there may be a temptation to “sacralize” CPGs, following these recommendations—and only these recommendations—to the letter, to the extent that something that is not mentioned in the CPGs appears not to exist and is not used. Given that there are many areas and subjects about which there is not—and possibly never will be—information from high-quality clinical trials, we may be denying our patients the benefit of certain diagnostic or therapeutic interventions for the sake of excessive, misunderstood, rigorous adherence to CPGs and EBM.
A clear example of these limitations of CPGs is the debate on infective endocarditis prophylaxis, for which different CPGs recommend different approaches, from use only in patients with high risk of endocarditis to the recommendation to not use prophylaxis in any patient given the lack of available evidence.9,10 This discord may lead to wide variability in professionals’ practice and, as has recently been brought to attention, may even lead to the use of endocarditis prophylaxis in situations in which it is clearly not indicated.11
Heart failure is another good example of how the role of CPGs should focus on the care of patients with this condition and how following an incorrect interpretation of CPGs can affect our daily practice. Cardiology is probably the medical specialty with the highest level of evidence from well-controlled, well-designed clinical trials, particularly in the case of and HF.4,5 The current ESC guidelines on HF were published in 2016, almost 4 years ago,4 and a new update is not planned until 2021. During this time, as is well known, a large number of studies, clinical trials and meta-analyses on HF have been published, and the presentation and publication of many others is expected in the coming months. Many of these mean—or will mean—a change in the paradigm of HF treatment,12 and others have demonstrated no benefit from certain interventions,13 to cite some well-known examples. Furthermore, as previously mentioned, there remains an apparent lack of information and evidence on many practical aspects of strong interest for physicians and patients and, for many of them, we will probably never have solid evidence. Therefore, it is important to produce documents that, with the limitations already acknowledged here, analyze these orphan topics. These documents should make recommendations based on new evidence not yet added to CPGs from nonexperimental studies (eg, cohorts), pathophysiological mechanisms, and experts’ clinical judgement. Furthermore, these documents should help us solve the specific problems posed by our patients that are currently left unanswered by CPGs. The scientific societies began this process a few years ago, and there are some high-quality examples relating to HF, from the ESC14 and the North American societies.15
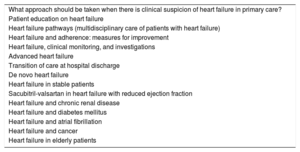
In Spain, in Revista Española de Cardiología Suplementos, a long consensus document was recently published on HF with reduced ejection fraction, titled “Expert consensus on heart failure with reduced ejection fraction: beyond the guidelines,”16 which follows this approach and attempts to answer the unresolved questions on this subject. This publication presents information on 15 topics related to HF with reduced ejection fraction (table 1) that include not only treatment-related aspects, but also those related to diagnosis, monitoring, and follow-up, updates in the different care settings (primary care, clinical pathways, transition of care at discharge), patient education and treatment adherence, types of HF (de novo, advanced, stable), and the practical approach in different types of patient and comorbidities (advanced age, diabetes, cancer, chronic renal disease, and atrial fibrillation). The drafting of this document involved the participation of cardiologists, internists, primary care physicians and nurse coordinators, and each section has a similar structure: review of the available evidence, points to consider, recommendations, and summary.
Topics analyzed in the expert consensus on heart failure with reduced ejection fraction by Anguita et al.16
| What approach should be taken when there is clinical suspicion of heart failure in primary care? |
| Patient education on heart failure |
| Heart failure pathways (multidisciplinary care of patients with heart failure) |
| Heart failure and adherence: measures for improvement |
| Heart failure, clinical monitoring, and investigations |
| Advanced heart failure |
| Transition of care at hospital discharge |
| De novo heart failure |
| Heart failure in stable patients |
| Sacubitril-valsartan in heart failure with reduced ejection fraction |
| Heart failure and chronic renal disease |
| Heart failure and diabetes mellitus |
| Heart failure and atrial fibrillation |
| Heart failure and cancer |
| Heart failure in elderly patients |
In my opinion, possibly biased from having been one of the participants in drafting the document, this type of multidisciplinary approach that combines a theoretical review of the evidence—when it exists—with the practical in the form of specific recommendations, is of strong interest, as are the documents published by the other scientific societies mentioned previously.14,15 A critical and personal reading of these documents, adapted to the professional environment of each reader and always under the umbrella of evidence and CPGs, could help us improve our routine care of patients with HF by shining a light on a normally shadowy area.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.