The Canary Islands has the highest mortality from diabetes in Spain. The aim of this study was to determine possible differences in mortality due to acute myocardial infarction (AMI) during hospital admission between this autonomous community and the rest of Spain, as well as the factors associated with this mortality and the population fraction attributable to diabetes.
MethodsCross-sectional study of hospital admissions for AMI in Spain from 2007 to 2014, registered in the Minimum Basic Data Set.
ResultsA total of 415 798 AMI were identified. Canary Island patients (16 317) were younger than those living in the rest of Spain (63.93 ± 13.56 vs 68.25 ± 13.94; P < .001) and death occurred 4 years earlier in the archipelago (74.03 ± 11.85 vs 78.38 ± 11.10; P < .001). This autonomous community had the highest prevalence of smoking (44% in men and 23% in women); throughout Spain, AMI occurred 13 years earlier in smokers than in nonsmokers. Patients in the Canary Islands had the highest mortality rates whether they had diabetes (8.7%) or not (7.6%), and they also showed the highest fraction of AMI mortality attributable to diabetes (9.4; 95%CI, 4.8-13.6). After adjustment for type of AMI, diabetes, dyslipidemia, hypertension, smoking, cocaine use, renal failure, sex and age, the Canary Islands showed the highest risk of mortality vs the rest of Spain (OR = 1.25; 95%CI, 1.17-1.33; P < .001) and it was one of the autonomous communities showing no significant improvement in the risk of mortality due to AMI during the study period.
ConclusionsMortality due to AMI during hospital admission is higher in the Canary Islands than in the rest of Spain.
Keywords
Death from cardiovascular disease has fallen in developed countries and in many developing countries during the past 25 years.1 Nonetheless, ischemic heart disease is still the leading cause of death worldwide.2 Although the trend has also been downward in Spain, the Canary Islands is one of the autonomous communities with the highest mortality rates from this disease.3
In developed countries, the reduction in ischemic heart disease mortality is attributed to improved secondary and tertiary prevention via targeting of cardiovascular risk factors (CVRFs) and better management of acute coronary syndrome via the use of early interventions.4 Cardiovascular risk factors increase the likelihood of an acute myocardial infarction (AMI) but, once the event occurs, they do not necessarily behave as risk factors for in-hospital mortality. Indeed, although diabetes is associated with increased in-hospital mortality from AMI,5 this is not the case for hypertension,6,7 smoking,8,9 or dyslipidemia,10,11 which can paradoxically be associated with a lower risk of death. Similarly, age and male sex are the 2 major cardiovascular risk markers but, once an AMI occurs, female sex better predicts hospital mortality.12
The prevalences of type 2 diabetes mellitus (T2DM), hypertension, and dyslipidemia in the general population of the Canary Islands are among the highest in Spain.13 Moreover, diabetes-related mortality is much higher than in the rest of the country.14 The high exposure of the Canarian population to CVRFs is one cause of their high mortality from ischemic heart disease, but the prevalence of diabetes in people with AMI is unknown, as well as the strength of its association with mortality after an infarction. It would be of interest to determine the risk of AMI mortality associated with diabetes in the Canary Islands and compare it with that of the rest of Spain.
The objectives of this article were to determine if there are differences in in-hospital mortality from AMI between the Canary Islands and the other autonomous communities, to analyze the CVRFs associated with this mortality, and to estimate the population attributable fraction (PAF) of AMI mortality attributable to T2DM.
METHODSThis cross-sectional study examined hospital admissions with AMI as the main diagnosis recorded in Spanish hospitals from 2007 to 2014. The data were collected from the Minimum Data Set. As part of the Health Information System of the Spanish National Health System, this database integrates clinical information on discharges after hospitalization episodes from public and private centers throughout Spain. The database was requested from the Spanish Ministry of Health, Social Services, and Equality; the data provided were encrypted and, due to the anonymous nature of the database, it was not necessary to obtain informed consent or the approval of an ethics committee to conduct the study.
This study used hospital records identified with code 410 in the “Main diagnosis” column according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). Myocardial infarctions were classified according to the presence of electrocardiographic ST-segment elevation (STEMI and NSTEMI, respectively) (code 410.7). Hospitalization episodes were classified by the autonomous community where the admission occurred; cases registered in the Autonomous Cities of Ceuta and Melilla were excluded due to their small population. Information was obtained from the secondary diagnoses appearing in the Minimum Basic Data Set for each hospitalization episode, as well as age, sex, community of admission, and year and reason for hospital discharge (including death).
With the variables obtained from all secondary diagnoses of the hospitalization episode, the morbidity variables or CVRFs identified were obtained via selection of the corresponding ICD-9-CM codes. To do so, dichotomous variables were created for each of the possible diagnoses and the information was grouped into a general variable that assigned to each episode the presence of that disease or CVRF. This method identified T2DM (ICD-9-CM codes from 250.00 to 250.93, selecting codes whose fifth digit was 0 or 2), hypertension (codes 401.0 to 405.99), dyslipidemia (codes 272.0 to 272.9), renal failure (codes 585.1 to 585.9), smoking (codes 305.1 and 989.84), and cocaine use (codes 304.2 and 305.6).
Statistical AnalysisQuantitative variables are expressed as mean ± standard deviation and categorical variables as frequency. Means were compared using the Student t test for 2 independent groups or analysis of variance for more than 2 groups. The annual change in the proportion of STEMI was analyzed with the chi-square test for trends.
Although the study results were obtained for all AMIs, the mortality rates in patients with and without T2DM were calculated only in the age group (45-84 years) showing stable rates of infarctions and deaths in all communities. These mortality rates were standardized by age using the direct method. To this end, the specific mortality rate/1000 patients in each 5-year age group during the study period was calculated in all autonomous communities; this rate was subsequently applied to the age structure of the standard population, which was the dataset of all infarctions in Spain during that period.
In the multivariate analysis, a linear regression model was applied to each community for the dependent variable “age at AMI”; the results are reported as regression coefficients and their 95% confidence intervals (95%CIs). Logistic regression models were also developed to estimate the risk of death during admission, both from each autonomous community vs Spain and from the last year studied (2014) vs the initial year of the period (2007); the results are reported as odds ratios (ORs) and their 95%CIs. The adjustment variables in all models were age, sex, T2DM, dyslipidemia, smoking, cocaine use, STEMI, hypertension, renal failure, and year of admission. Finally, the PAF of AMI mortality attributable to diabetes was calculated, understood as the percentage of deaths due to AMI that would be averted if T2DM were eliminated; it was calculated as the difference between the prevalence of T2DM in the deceased minus the ratio between the same prevalence of T2DM and the relative risk (OR) of death from AMI in patients with T2DM (P – [P / OR]). SPSS version 21.0 was used for the data analysis.
RESULTSIn total, there were 415 798 hospital admissions due to AMI during the study period (16 317 in the Canary Islands and 399 481 in the rest of Spain). Although the number of admissions per year remained stable between 51 500 and 53 000, the proportion of STEMI decreased over time from 66% in 2007 to 61% in 2014 (P < .001).
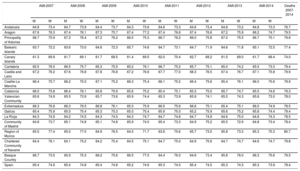
The number of in-hospital deaths was 1190 in the Canary Islands and 32 376 in the rest of the country. The ages of the patients who had an AMI, stratified by sex and autonomous community, are shown in Table 1. Patients experienced an AMI event at younger ages in the Canary Islands than in the other communities (P < .001), occurring on average 5 years earlier in women and 3 years earlier in men. In the 2007 to 2014 period, the mean age of the patients was 63.9 ± 13.6 years in the Canary Islands vs 68.3 ± 13.9 years in Spain as a whole (P < .001). Likewise, those who died during hospitalization were 4 years younger in the Canary Islands (74.0 ± 11.9 years vs 78.4 ± 11.1 years; P < .001).
Average Age of Men and Women Hospitalized for Myocardial Infarction by Year and Autonomous Community, as Well as in Spain as a Whole, and In-hospital Deaths Between 2007 and 2014
| AMI-2007 | AMI-2008 | AMI-2009 | AMI-2010 | AMI-2011 | AMI-2012 | AMI-2013 | AMI-2014 | Deaths 2007-2014 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | W | M | W | M | W | M | W | M | W | M | W | M | W | M | W | ||
| Andalusia | 64.8 | 73.4 | 64.7 | 73.9 | 64.4 | 73.7 | 64.3 | 73.6 | 64.6 | 73.3 | 64.6 | 73.4 | 64.8 | 73.2 | 64.8 | 73.3 | 76.7 |
| Aragon | 67.6 | 76.3 | 67.4 | 76.1 | 67.3 | 75.7 | 67.4 | 77.2 | 67.4 | 76.6 | 67.4 | 76.6 | 67.2 | 75.9 | 66.2 | 74.7 | 79.5 |
| Principality of Asturias | 66.7 | 75.9 | 67.3 | 76.4 | 67.2 | 76.2 | 66.0 | 75.3 | 66.7 | 76.2 | 66.0 | 75.8 | 67.0 | 75.5 | 66.7 | 75.1 | 79.6 |
| Balearic Islands | 63.7 | 72.2 | 63.6 | 73.0 | 64.6 | 72.3 | 65.7 | 74.6 | 64.7 | 73.1 | 64.7 | 71.9 | 64.6 | 71.8 | 65.1 | 72.5 | 77.4 |
| Canary Islands | 61.3 | 69.9 | 61.7 | 69.1 | 61.7 | 68.5 | 61.4 | 69.5 | 62.0 | 70.4 | 62.7 | 68.2 | 61.5 | 69.0 | 61.7 | 68.4 | 74.0 |
| Cantabria | 65.5 | 76.0 | 66.5 | 75.7 | 65.3 | 75.5 | 65.2 | 76.1 | 66.7 | 75.2 | 65.7 | 75.1 | 65.0 | 74.2 | 65.5 | 73.3 | 79.4 |
| Castile and León | 67.2 | 76.2 | 67.6 | 76.8 | 67.8 | 76.8 | 67.2 | 76.6 | 67.7 | 77.0 | 68.3 | 76.5 | 67.4 | 76.7 | 67.1 | 75.8 | 79.9 |
| Castile-La Mancha | 66.4 | 75.7 | 66.2 | 75.0 | 67.1 | 75.2 | 66.3 | 75.4 | 66.1 | 75.2 | 66.4 | 75.6 | 65.4 | 76.1 | 66.0 | 75.6 | 79.9 |
| Catalonia | 66.0 | 75.8 | 66.4 | 76.1 | 65.8 | 75.9 | 65.6 | 75.2 | 65.4 | 75.1 | 65.3 | 75.0 | 65.7 | 74.7 | 65.5 | 74.6 | 79.3 |
| Valencian Community | 65.6 | 74.9 | 65.5 | 73.9 | 65.7 | 73.6 | 65.9 | 74.4 | 65.3 | 73.9 | 65.9 | 74.1 | 65.5 | 74.3 | 65.8 | 73.0 | 78.0 |
| Extremadura | 66.3 | 76.8 | 66.3 | 76.5 | 66.8 | 76.1 | 65.3 | 75.9 | 66.5 | 75.6 | 66.6 | 75.1 | 65.4 | 75.1 | 66.0 | 74.9 | 78.5 |
| Galicia | 65.4 | 75.9 | 65.5 | 75.4 | 65.3 | 75.3 | 65.0 | 75.4 | 65.9 | 75.0 | 65.2 | 75.9 | 65.6 | 75.2 | 65.8 | 74.4 | 79.4 |
| La Rioja | 64.3 | 74.9 | 64.2 | 74.5 | 64.3 | 74.5 | 64.3 | 74.7 | 64.7 | 74.8 | 64.7 | 74.9 | 64.6 | 75.0 | 64.8 | 74.3 | 78.5 |
| Community of Madrid | 64.8 | 73.7 | 65.1 | 74.8 | 65.1 | 74.8 | 65.9 | 74.0 | 65.4 | 73.3 | 64.9 | 75.2 | 65.5 | 72.9 | 64.8 | 73.4 | 78.4 |
| Region of Murcia | 65.5 | 77.4 | 65.0 | 77.0 | 64.9 | 76.5 | 64.5 | 71.7 | 63.6 | 75.6 | 65.7 | 73.5 | 65.8 | 73.3 | 65.3 | 75.3 | 80.7 |
| Chartered Community of Navarre | 64.4 | 76.1 | 64.1 | 75.2 | 64.2 | 75.4 | 64.5 | 75.1 | 64.7 | 75.0 | 64.9 | 75.6 | 64.7 | 74.7 | 64.6 | 74.7 | 79.8 |
| Basque Country | 66.7 | 73.5 | 65.9 | 75.3 | 66.2 | 75.6 | 66.5 | 77.0 | 64.4 | 76.0 | 64.6 | 73.4 | 65.8 | 76.0 | 66.3 | 75.6 | 79.5 |
| Spain | 65.4 | 74.9 | 65.4 | 74.8 | 65.4 | 74.6 | 65.2 | 74.6 | 65.3 | 74.5 | 65.4 | 74.5 | 65.3 | 74.3 | 65.3 | 73.9 | 78.4 |
AMI, acute myocardial infarction; M, men; W, women.
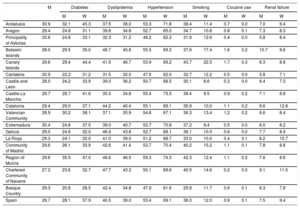
The proportion of AMI in women in each autonomous community is shown in Table 2, as well as the prevalence of T2DM, dyslipidemia, hypertension, smoking, cocaine use, and renal failure. All of these factors showed significant differences (P < .001) in their distributions among the communities. The Canary Islands had the highest prevalence of the 2 factors associated with the greatest drop in age at AMI: smoking (43.7% of men and 22.5% of women) and cocaine use (1.7% of men and 0.3% of women). Due to its high prevalence, male smokers experienced an AMI 13 years earlier than nonsmokers in the country as a whole (at 57.0 ± 11.5 years vs 70.1 ± 12.3 years; P < .001); female smokers had an infarction event almost 21 years earlier than nonsmokers (at 56.2 ± 10.9 years vs 77.0 ± 10.7 years; P < .001).
Proportion of Women and Prevalence of Risk Factors in Patients Hospitalized for Myocardial Infarction by Autonomous Community
| M | Diabetes | Dyslipidemia | Hypertension | Smoking | Cocaine use | Renal failure | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | W | M | W | M | W | M | W | M | W | M | W | ||
| Andalusia | 30.9 | 32.1 | 45.3 | 37.5 | 38.0 | 53.3 | 71.8 | 38.4 | 11.4 | 0.7 | 0.0 | 7.0 | 9.4 |
| Aragon | 29.4 | 24.8 | 31.1 | 39.8 | 34.8 | 52.7 | 65.0 | 34.7 | 10.8 | 0.8 | 0.1 | 7.3 | 8.3 |
| Principality of Asturias | 33.6 | 24.8 | 33.1 | 32.3 | 31.2 | 46.2 | 62.3 | 31.9 | 12.6 | 0.4 | 0.0 | 5.8 | 8.4 |
| Balearic Islands | 28.0 | 29.5 | 35.0 | 46.7 | 45.8 | 55.5 | 69.3 | 37.6 | 17.4 | 1.6 | 0.2 | 10.7 | 9.6 |
| Canary Islands | 29.6 | 29.4 | 44.4 | 41.5 | 46.7 | 53.9 | 69.2 | 43.7 | 22.5 | 1.7 | 0.3 | 6.3 | 8.8 |
| Cantabria | 30.9 | 22.2 | 31.2 | 31.5 | 32.0 | 47.5 | 62.0 | 32.7 | 12.2 | 0.5 | 0.0 | 5.8 | 7.1 |
| Castile and León | 28.0 | 24.2 | 33.9 | 39.0 | 36.2 | 50.7 | 68.5 | 30.1 | 8.6 | 0.3 | 0.0 | 6.4 | 7.3 |
| Castile-La Mancha | 29.7 | 28.7 | 41.6 | 35.5 | 34.8 | 55.4 | 73.5 | 39.4 | 9.5 | 0.9 | 0.2 | 7.1 | 8.8 |
| Catalonia | 29.4 | 29.0 | 37.1 | 44.2 | 40.4 | 55.1 | 69.1 | 30.9 | 10.0 | 1.1 | 0.2 | 9.6 | 12.8 |
| Valencian Community | 28.9 | 30.2 | 38.1 | 37.1 | 35.9 | 54.8 | 67.1 | 36.3 | 13.4 | 1.2 | 0.2 | 6.6 | 8.4 |
| Extremadura | 30.4 | 24.8 | 37.5 | 39.0 | 40.7 | 53.7 | 70.8 | 37.2 | 9.4 | 0.5 | 0.0 | 6.0 | 8.2 |
| Galicia | 29.0 | 24.6 | 32.0 | 46.9 | 43.8 | 52.7 | 68.1 | 36.1 | 10.0 | 0.6 | 0.0 | 7.7 | 8.9 |
| La Rioja | 29.3 | 24.1 | 32.0 | 41.0 | 39.0 | 51.2 | 68.7 | 33.0 | 10.0 | 0.4 | 0.1 | 8.2 | 10.7 |
| Community of Madrid | 29.6 | 26.1 | 33.9 | 42.6 | 41.4 | 53.7 | 70.4 | 40.2 | 15.2 | 1.1 | 0.1 | 7.8 | 8.8 |
| Region of Murcia | 29.6 | 35.5 | 47.0 | 46.6 | 46.5 | 59.3 | 74.3 | 42.3 | 12.4 | 1.1 | 0.2 | 7.6 | 8.6 |
| Chartered Community of Navarre | 27.2 | 23.6 | 32.7 | 47.7 | 43.3 | 50.1 | 69.6 | 40.5 | 14.6 | 0.2 | 0.0 | 9.1 | 11.5 |
| Basque Country | 29.3 | 20.8 | 28.5 | 42.4 | 34.8 | 47.9 | 61.6 | 29.9 | 11.7 | 0.6 | 0.1 | 6.3 | 7.8 |
| Spain | 29.7 | 28.1 | 37.9 | 40.5 | 39.0 | 53.4 | 69.1 | 36.0 | 12.0 | 0.9 | 0.1 | 7.5 | 9.4 |
M, men; W, women.
Values express percentages.
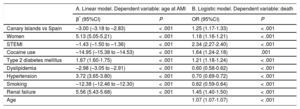
The linear model for age at AMI is shown in Table 3A: after adjustment for the factors studied, the Canary Islands continued to show a younger age at AMI than the rest of Spain (β = –3.00); in addition, cocaine users had an infarction 15 years earlier than nonusers (r = –14.95) and smokers 12 years earlier than nonsmokers (r = –12.38). The logistic model for in-hospital mortality is shown in Table 3B: the variable with the strongest association with an increased risk of death was STEMI (OR, 2.34), followed by cocaine use (OR, 1.64), renal failure (OR, 1.45), having an AMI in the Canary Islands (OR, 1.25), T2DM (OR, 1.21), and female sex (OR, 1.18). Stratification of the analysis between STEMI and NSTEMI did not modify the lower age of AMI patients in the Canary Islands (β = 3.00 for both types of AMI) but showed that the excess risk of death in the Canary Islands vs Spain was higher with STEMI (OR, 1.33) than with NSTEMI (OR, 1.18).
Factors Associated With Age at Myocardial Infarction and Risk of Death in Patients Admitted for Myocardial Infarction
| A. Linear model. Dependent variable: age at AMI | B. Logistic model. Dependent variable: death | |||
|---|---|---|---|---|
| β* (95%CI) | P | OR (95%CI) | P | |
| Canary Islands vs Spain | –3.00 (–3.18 to –2.83) | < .001 | 1.25 (1.17-1.33) | < .001 |
| Women | 5.13 (5.05-5.21) | < .001 | 1.18 (1.16-1.21) | < .001 |
| STEMI | –1.43 (–1.50 to –1.36) | < .001 | 2.34 (2.27-2.40) | < .001 |
| Cocaine use | –14.95 (–15.38 to –14.53) | < .001 | 1.64 (1.24-2.18) | .001 |
| Type 2 diabetes mellitus | 1.67 (1.60-1.75) | < .001 | 1.21 (1.18-1.24) | < .001 |
| Dyslipidemia | –2.98 (–3.05 to –2.91) | < .001 | 0.60 (0.58-0.62) | < .001 |
| Hypertension | 3.72 (3.65-3.80) | < .001 | 0.70 (0.69-0.72) | < .001 |
| Smoking | –12.38 (–12.46 to –12.30) | < .001 | 0.62 (0.59-0.64) | < .001 |
| Renal failure | 5.56 (5.43-5.68) | < .001 | 1.45 (1.40-1.50) | < .001 |
| Age | 1.07 (1.07-1.07) | < .001 | ||
95%CI, 95% confidence interval; AMI, acute myocardial infarction; OR, odds ratio; STEMI, ST-segment elevation myocardial infarction.
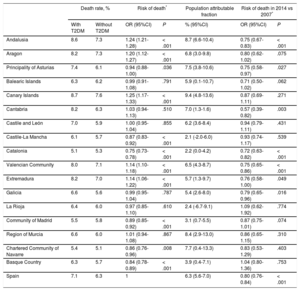
The following can be seen in Table 4: a) the Canary Islands had the highest mortality rates in patients with T2DM (8.7%); b) the rates were also highest for patients without T2DM (7.6%); c) after multivariable adjustment, the risks of death from AMI in the Canary Islands (OR, 1.25), Andalusia (OR, 1.24), and Aragon (OR, 1.20) exceeded that of Spain as a whole; d) the highest percentage of avoidable deaths if T2DM were eliminated was obtained in the Canary Islands (PAF = 9.4%), followed by Andalusia (PAF = 8.7%) and Murcia (PAF = 8.4%); and e) the risk of death in 2014 vs 2007 decreased in the country as a whole (OR, 0.80), but only significantly so in 6 of the 17 autonomous communities.
Standardized Mortality Rates of Patients Aged 45 to 84 Years With and Without T2DM Admitted for Myocardial Infarction. Estimated Risk of Death in Each Autonomous Community vs Spain. Population Attributable Fraction for Infarction Death Attributable to T2DM and Risk of Death in 2014 vs 2017
| Death rate, % | Risk of death* | Population attributable fraction | Risk of death in 2014 vs 2007* | ||||
|---|---|---|---|---|---|---|---|
| With T2DM | Without T2DM | OR (95%CI) | P | % (95%CI) | OR (95%CI) | P | |
| Andalusia | 8.6 | 7.3 | 1.24 (1.21-1.28) | < .001 | 8.7 (6.6-10.4) | 0.75 (0.67-0.83) | < .001 |
| Aragon | 8.2 | 7.3 | 1.20 (1.12-1.27) | < .001 | 6.8 (3.0-9.8) | 0.80 (0.62-1.02) | .075 |
| Principality of Asturias | 7.4 | 6.1 | 0.94 (0.88-1.00) | .036 | 7.5 (3.8-10.6) | 0.75 (0.58-0.97) | .027 |
| Balearic Islands | 6.3 | 6.2 | 0.99 (0.91-1.08) | .791 | 5.9 (0.1-10.7) | 0.71 (0.50-1.02) | .062 |
| Canary Islands | 8.7 | 7.6 | 1.25 (1.17-1.33) | < .001 | 9.4 (4.8-13.6) | 0.87 (0.69-1.11) | .271 |
| Cantabria | 8.2 | 6.3 | 1.03 (0.94-1.13) | .510 | 7.0 (1.3-1.6) | 0.57 (0.39-0.82) | .003 |
| Castile and León | 7.0 | 5.9 | 1.00 (0.95-1.04) | .855 | 6.2 (3.6-8.4) | 0.94 (0.79-1.11) | .431 |
| Castile-La Mancha | 6.1 | 5.7 | 0.87 (0.83-0.92) | < .001 | 2.1 (-2.0-6.0) | 0.93 (0.74-1.17) | .539 |
| Catalonia | 5.1 | 5.3 | 0.75 (0.73-0.78) | < .001 | 2.2 (0.0-4.2) | 0.72 (0.63-0.82) | < .001 |
| Valencian Community | 8.0 | 7.1 | 1.14 (1.10-1.18) | < .001 | 6.5 (4.3-8.7) | 0.75 (0.65-0.86) | < .001 |
| Extremadura | 8.2 | 7.0 | 1.14 (1.06-1.22) | < .001 | 5.7 (1.3-9.7) | 0.76 (0.58-1.00) | .049 |
| Galicia | 6.6 | 5.6 | 0.99 (0.95-1.04) | .787 | 5.4 (2.6-8.0) | 0.79 (0.65-0.96) | .016 |
| La Rioja | 6.4 | 6.0 | 0.97 (0.85-1.10) | .610 | 2.4 (-6.7-9.1) | 1.09 (0.62-1.92) | .774 |
| Community of Madrid | 5.5 | 5.8 | 0.89 (0.85-0.92) | < .001 | 3.1 (0.7-5.5) | 0.87 (0.75-1.01) | .074 |
| Region of Murcia | 6.6 | 6.0 | 1.01 (0.94-1.08) | .867 | 8.4 (2.9-13.0) | 0.86 (0.65-1.15) | .310 |
| Chartered Community of Navarre | 5.4 | 5.1 | 0.86 (0.76-0.96) | .008 | 7.7 (0.4-13.3) | 0.83 (0.53-1.29) | .403 |
| Basque Country | 6.3 | 5.7 | 0.84 (0.78-0.89) | < .001 | 3.9 (0.4-7.1) | 1.04 (0.80-1.36) | .753 |
| Spain | 7.1 | 6.3 | 1 | 6.3 (5.6-7.0) | 0.80 (0.76-0.84) | < .001 | |
95%CI, 95% confidence interval; OR, odds ratio; T2DM, type 2 diabetes mellitus.
The Canary Islands presents a highly unfavorable situation, with AMI and AMI-related death occurring at a younger age than in the rest of Spain. Acute myocardial infarction occurrence is strongly associated with smoking. Mortality is higher in patients in the Canary Islands with and without T2DM, and it is the autonomous community with the highest PAF of AMI mortality attributable to T2DM, that is, the community that would avoid the highest percentage of deaths if T2DM were eliminated. In addition, the archipelago did not significantly improved its risk of death during the 8-year study period.
The difference in the mean ages of the patients admitted for AMI between the Canary Islands and Spain was greater than 4 years, and it remained considerable even after adjustment for the CVRFs analyzed. These 4 years generated a loss of 65 000 years of disability-free life (4 times the 16 317 AMIs recorded in the Canary Islands) and 4700 potential years of life lost (4 times the 1190 deaths recorded in the region). This difference may be explained may be smoking, because its prevalence was particularly high in the Canary Islands and it was associated with a considerable reduction in the age of admission for AMI: more than 1 decade in men and more than 2 in women. The cross-sectional design of this study did not allow causality relationships to be established, but there were several indicators of the impact of smoking: a) the Canary Islands was the autonomous community with the highest prevalence of smoking in both sexes; b) this habit was much more common in men (44%) than in women (23%) and, accordingly, the age of admission was also younger in men; and c) the difference between the smoking rates of Canarian women and those of the other autonomous communities was higher than that of men and the difference in the age of admission was also higher. Unsurprisingly, the prevalence of smoking was much higher in patients admitted for AMI than in the general population, but a question to be answered in future studies is why the prevalence of smoking reported by the population of the archipelago is among the lowest in Spain,15,16 despite Canarian AMI patients having the highest rate. Irrespective of this question, the results indicate the need for improved smoking prevention as a more effective measure to save years of life.
Even more than tobacco, cocaine use advanced the age of AMI occurrence, but its use was fortunately low vs smoking. Both the lower age and the prevalence of cocaine use were similar to those of other countries17 and to the rates previously reported for Spain.18 However, the Canary Islands was once again at the top of the list of cocaine use in the country, although it was still infrequent vs other CVRFs. Cocaine addiction severity was associated with a considerable mortality increase (more than 60%) that was only exceeded by STEMI. The fall over time in the proportion of STEMI can probably be attributed to changes in the definition of AMI during the last decade.19 Additionally, the lower proportion of STEMI in other studies may be due to the inclusion of out-of-hospital AMIs,20 the exclusion of almost half of hospitalized patients (due to strict exclusion criteria),21 or the recruitment of AMI cases without population representativeness criteria.22 Because the determinants of care do not fall within the objectives of this work, new studies are needed to analyze if there are relevant differences among the treatments and procedures applied in each community to different types of infarction.
After cocaine, the only other CVRFs associated with increased mortality were T2DM and renal failure. For the latter, there was no previous information on its prevalence in patients with AMI in the Spanish autonomous communities; regardless, the interregional variation found here was lower than the differences published for dialysis due to end-stage renal failure secondary to T2DM.23 Although the patients who experienced both diseases were older, the excess mortality persisted after adjustment for age. The Canary Islands had the highest AMI mortality of patients with T2DM, with rates well above the national average, reaching a relative risk of 1.7 vs Catalonia (RR = 8.7/5.1), the community with the lowest mortality attributable to T2DM. This high mortality from T2DM-related AMI is consistent with the previous description of high T2DM-related mortality in the general population of the archipelago.14,24 However, the determination that mortality among patients without T2DM in these islands was also the highest in Spain was novel; it reached a relative risk of 1.5 vs the Autonomous Community of Navarra (RR = 7.6/5.1), which had the lowest AMI mortality in the absence of T2DM. This meant that the risk attributable to T2DM (difference in mortality with and without the disease) did not reflect the scale of the problem in the Canary Islands. Thus, PAF is a more appropriate tool to indicate that the Canary Islands is the community with the highest percentage of deaths that could be averted if T2DM were eliminated. The second and third places on this indicator are Andalusia and the Region of Murcia, whose PAF to T2DM exceeded 8%; in contrast, some autonomous regions had a PAF less than 4%. The usefulness of the PAF for the prevention of coronary heart disease in Spain has been determined.25
After adjustment for all of the CVRFs and markers studied, the highest relative risk of death after AMI was still found in the Canary Islands, Andalusia, and Aragon, with the lowest in Catalonia. Comparison of the mortality rates due to AMI of the highest and lowest autonomous communities revealed that the risk in the Canary Islands exceeded that in Catalonia by approximately 60%. In addition, the Canary Islands was the only 1 of the 5 communities with a risk of death higher than Spain as a whole not to show a significant or almost significant reduction between 2007 and 2014. These results indicate considerable differences in hospital mortality after AMI among the different autonomous communities, indicating a need for analysis of Spanish health system inequalities. The type of hospital, direct treatment in a cardiology unit, and percutaneous coronary intervention are significantly associated with the survival of patients admitted for AMI.26 It would be interesting to compare other factors such as the transfer time from regional hospitals (smaller islands in the Canarian archipelago) to third-level centers (main islands) for angioplasties and to analyze AMIs occurring in the tourist population, which is considerable in the archipelago, as well as other communities. These aspects require further investigation and caution should be exercised until the relevant studies are completed.
Paradoxically, dyslipidemia, hypertension, and smoking are linked to lower mortality after AMI. As stated above, although CVRFs increase the likelihood of an AMI, they do not necessarily behave as risk factors for death. These phenomena have already been described for both the factors studied here6–11 and others not addressed, such as obesity.27 The apparent benefit on hospital mortality obtained by patients admitted with 1 or more CVRFs does not prevent their 10-year mortality from being higher than that of patients without risk factors. The difficulty in explaining these phenomena lies in the complexity of the analysis of baseline exposures. For example, participants with dyslipidemia or hypertension may or may not be correctly treated and people with obesity might be physically active. There is no doubt that patients with CVRFs have benefited from the most important mortality reductions during recent decades,28 and although there is no definitive explanation for these paradoxes, these associations disappear after adjustment for the demographic differences and baseline exposures of the patients studied.29
Strengths and LimitationsThe main limitations of the study involve the Minimum Data Set. This type of database may contain some degree of underreporting by the physicians who prepare hospital discharge reports or by the administrative coding staff when, for reasons such as work overload, severe diagnoses are more often recorded than risk factors.30 Neither can the database measure the incidence of disease in the general population because approximately 30% of AMI deaths occur in nonhospitalized patients.20 Additionally, repeat events in the same individual may lead to an underestimation of mortality vs the affected population, although not lethality vs the number of events. However, the quality of the Minimum Data Set data has been demonstrated and the data are valid for health research31 and have been successfully used in studies of cardiovascular events.5 Our main strength is the large sample size, extracted from the records of all hospitals in Spain.
CONCLUSIONSIn conclusion, in the first decades of the 21st century, the Canary Islands has shown a highly unfavorable situation vs the whole of Spain in terms of in-hospital mortality from AMI. The Canary Islands has the highest mortality of patients with or without T2DM but is the autonomous community that would avoid the highest percentage of deaths if T2DM were eliminated. Its population experiences these events 4 years sooner than the country as a whole and dies 4 years earlier. Smoking is the main causative factor because it is associated with a considerable drop in the age of admission and its prevalence is much higher in Canarian patients than in Spanish; its prevention must thus be improved. In addition to being the autonomous community with the highest risk of death from AMI, the archipelago is one of the few communities to not show a significant improvement in risk during the 8-year study period.
CONFLICTS OF INTERESTNone declared.
- –
Mortality due to T2DM is higher in the general population of the Canary Islands than in the other autonomous communities of Spain.
- –
The prevalences of T2DM, hypertension, and dyslipidemia in the archipelago are among the highest in Spain.
- –
The prevalence of CVRF is unknown in people who experience an AMI in each autonomous community, as well as the fraction of AMI mortality attributable to T2DM.
- –
The Canary Islands show a highly unfavorable situation regarding in-hospital mortality from AMI. Their increased risk of death did not significantly improve during the 8-year study period.
- –
The Canary Islands have the highest in-hospital mortality from AMI in patients with or without T2DM. It is the autonomous community that would avoid the highest percentage of deaths if T2DM were eliminated.
- –
Its population experiences these events at an age 4 years younger than the rest of the country and dies 4 years earlier. Smoking is the main associated factor.