Arrhythmia and cardiac electrophysiology services are an innovative and fast-growing branch of clinical cardiology. Initiating an arrhythmia unit involves proper selection of personnel, as well as technical, structural, and organizational requirements. Proper selection of personnel includes specialized and well-trained physicians, nurses, and medical technicians in the electrophysiology laboratories and on the hospital wards. Standard electrophysiology laboratories must support the full spectrum of catheter-based diagnosis and therapies of cardiac arrhythmias. This includes state-of-the-art fluoroscopy and 3-dimensional mapping systems used during complex procedures such as catheter ablation of atrial fibrillation or ventricular tachycardia. Furthermore, technical requirements need to support pacemaker and defibrillator implantation as one of the core tasks of a specialized arrhythmia unit. Outpatient clinics should fulfill technical capabilities to perform a diverse spectrum of pre-and postinterventional diagnostics, guaranteeing proper patient follow-up. Structural requirements should focus on close physical integration of individual functional units allowing for an effective and safe workflow. Finally, organizational requirements such as networking between arrhythmia specialists and referring physicians and hospitals are essential for patient recruitment and high-quality postdischarge patient care. Regular educational programs for physicians, nurses, and technicians are essential in such an innovative and fast-growing field of cardiology.
Keywords
Arrhythmia and cardiac electrophysiology (EP) services are an innovative and fast-growing branch of clinical cardiology. Hospitals establish new arrhythmia units within or separate from the general cardiology department, either extending existing services or functioning as self-contained units. Initiating an arrhythmia unit involves proper selection of personnel, as well as technical, structural, and organizational requirements. Proper selection of personnel includes specialized and well-trained physicians, nurses, and medical technicians in the EP laboratories and on the hospital wards. Monitoring systems for noninvasive electrocardiographic, hemodynamic, and respiratory assessment of patients on the general wards and in intermediate and intensive care units are an important technical requirement. In addition, standard EP laboratories must support the full spectrum of catheter-based diagnosis and therapies of cardiac arrhythmias. This includes state-of-the-art fluoroscopy and 3-dimensional mapping systems used during complex procedures such as catheter ablation of atrial fibrillation or ventricular tachycardia. Furthermore, technical requirements need to support pacemaker and defibrillator implantation as one of the core tasks of a specialized arrhythmia unit. Outpatient clinics should fulfill technical capabilities to perform a diverse spectrum of pre-and postinterventional diagnostics, guaranteeing proper patient follow-up. Structural requirements should focus on close physical integration of individual functional units allowing for an effective and safe workflow. Finally, organizational requirements such as networking between arrhythmia specialists and referring physicians and hospitals are essential for patient recruitment and high-quality postdischarge patient care. Regular educational programs for physicians, nurses, and technicians are essential in such an innovative and fast-growing field of cardiology. Considering all these requirements, establishing an arrhythmia unit in the 21st century is a challenging but worthwhile endeavor.
REQUIREMENTS FOR SUCCESSFUL ESTABLISHMENT OF AN ARRHYTHMIA UNIT PersonnelClinical cardiac EP is a fast-growing subspecialty of general cardiology. Consequently, an arrhythmia unit dedicated to EP studies, catheter ablation of complex arrhythmias, and device implantation demands highly specialized physicians, nurses, and medical technicians. The basis for these qualifications is a well-structured educational program in general cardiology as well as training and regular teaching sessions in cardiac EP. In most European countries clinical EP is not an essential part of general cardiology training. However, due to the advanced technical and intellectual skills necessary to perform successful catheter ablation and device implantation, interested physicians should seek training in qualified centers with already well-established arrhythmia units and expertise in this complex field of cardiology. Fellowship programs developed by the European Heart Rhythm Association offer cardiologists the chance to gain the necessary expertise in EP at acknowledged arrhythmia units throughout various European countries. The impetus for these fellowships is to garner physicians with the required theoretical and practical competence in noninvasive and invasive EP.1 Qualified training centers demonstrate special expertise in catheter ablation of a wide array of atrial and ventricular arrhythmias, as well as pacemaker implantation, implantable cardioverter-defibrillators, and cardiac resynchronization therapy. There is a basic and advanced training program in invasive EP and an advanced program in device implantation. To establish and verify high quality standards the trainees are required to pass the European Heart Rhythm Association accreditation exam at the end of the fellowship. Following completion of training as an arrhythmia specialist, it is expected that individuals continue to pursue regular medical education. This may be in the form of continued medical education programs or national and international congresses. Importantly, regular teaching sessions within the home institution are necessary to ensure continued theoretical and practical competency. Essential parts of formal teaching sessions should include invasive EP in addition to basic noninvasive diagnostics such as electrocardiography (ECG)- and Holter-ECG interpretation, device interrogation, and programming.
Highly qualified and subspecialized nurses and medical technicians are an integral part of the arrhythmia team. Nurses may work at the EP laboratories or be involved in patient care and monitoring on the arrhythmia wards or at outpatient clinics. Inpatient nurses require advanced knowledge in the differential diagnosis of arrhythmias, including clinical characteristics, potential hazards, and treatment options. Another important aspect is the proper recognition of procedure-related complications, eg, groin hematoma or pneumothorax, pericardial effusion, or cardiac tamponade. In the outpatient setting nurses commonly perform basic diagnostics such as 12-lead surface or Holter-ECG monitoring. Depending on individual training and aptitude they may also perform pre- and postprocedural echocardiography, device interrogation, and device programming under close supervision of an attending physician.
The nursing staff in the EP laboratory requires a specific set of qualifications. First, it is the responsibility of the nursing staff to prepare the patient for the EP procedure. Proper placement of reference patches and correct positioning of ECG leads and defibrillator patches are of paramount importance. Detailed knowledge of the various hardware components such as recording systems, mapping systems, or heart stimulators as well as troubleshooting skills in case of technical problems are important qualifications. Moreover the EP nursing staff needs profound knowledge of indications and use of medication commonly utilized during EP procedures. Depending on hospital policy, they may be in charge of initiating sedation and monitoring the sedated patient under close supervision of the responsible physician. Intraprocedural monitoring of vital parameters, administration of select medication, and regular checking of coagulation parameters during left atrial procedures are the responsibility of the nursing staff. In addition, thorough knowledge of recognition and handling of potential intraprocedural complications and life-threatening emergency situations such as sudden oxygen desaturation, hemodynamically intolerable ventricular tachycardia, or acute pericardial effusion/tamponade is essential. Depending on the organization in the EP laboratory, nurses may acquire specific training in the use and handling of different 3-dimensional mapping systems (CARTOTM, Biosense Webster Inc.; NavXTM, St. Jude Medical) and different ablation systems (eg, radio-frequency current, cryoballoon, endoscopic ablation).
Nurses working in pacemaker, implantable cardioverter-defibrillator, or cardiac resynchronization therapy clinics require specific expertise in the mode of operation of devices and programming units as well as a thorough understanding of specific arrhythmias and therapy options. This in turn will allow nursing staff to perform device interrogation and, whenever necessary, device programming under supervision by an attending physician.
Furthermore, the initiation and guidance of clinical research studies is facilitated by well-trained nurses with special expertise in EP. They may organize selection and enrollment of patients, collect patient and procedural data, and perform patient follow-up.
Technical RequirementsAn arrhythmia unit specialized in invasive clinical EP is dependent on specific structural requirements as well as on sophisticated and cost-intensive technical equipment. Prior to setting up a new EP laboratory, one needs to consider the full spectrum of arrhythmias to be treated, the quantity of procedures to be performed, and whether the lab will predominantly be used for catheter ablation procedures or device implantation or both. What spectrum of arrhythmias is expected? Will robotic navigation systems like StereotaxisTM (Stereotaxis Inc., St. Louis, United States) or Hansen (SenseiTM; Hansen Medical Inc., Mountain View, California, United States) be installed, necessitating specific construction requirements?
The basic equipment for an EP laboratory consists of a fluoroscopy unit with either one or two C-arms (monoplane or biplane). Several EP recording systems are available on the market that allow both surface and intracardiac ECG recordings. Importantly, EP recording systems may differ in signal quality, handling, and initial and maintenance costs. While it is very important to install the most recent technology, it is equally important to select equipment physicians are acquainted with.
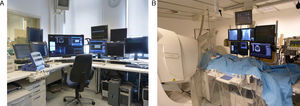
Electroanatomic mapping systems for 3-dimensional reconstruction of the cardiac chambers are one of the prerequisites to perform complex procedures such as catheter ablation of atrial fibrillation, atrial tachycardia, or ventricular tachycardia. Two different 3-dimensional mapping systems are commercially available. The CARTOTM (Biosense Webster Inc., Diamond Bar, California, United States) system utilizes a static magnetic field to allow virtual recording of the mapping catheter position, while the Ensite NavXTM (St. Jude Medical, Inc., St. Paul, Minnesota, United States) system relies on impedance measurements. Robotic navigation like the magnetic navigation system (StereotaxisTM) and the electromechanical navigation system (SenseiTM; Hansen Medical) was introduced to facilitate mapping and ablation of complex arrhythmias. The StereotaxisTM system uses 2 permanent magnets (Figure 1) installed in parallel to the operating table, requiring special reinforcement of the floor and shielding of the operating room. The Hansen system consists of a robotic arm attached to the operating table and a control unit installed in the control room (Figure 2). Both systems allow for remote-controlled manipulation and navigation of the ablation catheter and significantly reduce the physician's fluoroscopy exposure since catheters are manipulated from within the control room.2, 3
Figure 1. A. The control room of an electrophysiology lab equipped with a StereotaxisTM system, allowing for remote controlled navigation, mapping, and ablation of complex arrhythmias. B. In the fluoroscopy unit two permanent magnets are installed in parallel to the operating table, requiring special reinforcement of the floor and shielding of the operating room.
Figure 2. The Hansen system consists of a robotic arm attached to the operating table (A) and a control unit installed in the control room (B). It allows for remote-controlled manipulation and navigation of the ablation catheter and may significantly reduce the physician's fluoroscopy exposure since catheters are manipulated from within the control room via a 3-dimensional mouse.
Device implantation is commonly performed in the EP laboratory, in a dedicated device laboratory, or in the operating room. If devices are implanted in the operating room, dedicated space and availability will need to be ensured, which may pose a logistics problem if use interferes with normal surgical workflow.
Following complex ablation procedures or device implantations patients may need monitoring in the recovery unit or intensive care unit. Specially trained cardiologists and nurses work in recovery units and intensive care units, equipped with monitoring systems allowing for permanent noninvasive electrocardiographic, hemodynamic, and respiratory assessment.4 In case of emergency situations, external defibrillators and pacemakers as well as transthoracic echocardiography must be available.
A high-volume EP center will depend on close collaboration between the arrhythmia unit and the cardiac surgery unit. In select EP patients referral to cardiac surgery may be warranted while surgical procedures may benefit from input of an experienced electrophysiologist. Finally, surgical backup may prove indispensable in case of emergency.
Organizing an Arrhythmia UnitEstablishing a new and up-coming arrhythmia unit requires not only experienced and well-trained EP specialists and sophisticated equipment but also a contemporary, practical, and efficient organizational infrastructure. The first step is to recruit patients and assemble a network of referring and cooperating physicians and hospitals in a competitive marketplace.
In patients scheduled and admitted for an EP procedure or device implantation the projected therapy has to be performed in a cost- and time-efficient manner adhering to highest quality standards. Finally, all patients require in- and outpatient follow-up care, including periodic or emergency clinic visits.
Outpatient ClinicThe outpatient clinic often is separated into a dedicated pacemaker unit and an arrhythmia clinic. Patients may present as self-referrals or by outside physician referrals for further diagnosis, therapeutic recommendations, and treatment. The arrhythmia clinic operates during normal working hours. Patients are evaluated depending on their individual presenting symptoms. Thorough discussion of interventional treatment options including procedural success rates, possible procedure-related risks and expected duration of in-hospital stay are integral parts of the outpatient consultation. In patients without definite diagnosis further diagnostic steps are discussed and initiated. Noninvasive imaging such as transthoracic and transesophageal echocardiography as well as analysis and documentation of arrhythmia burden via surface-ECG, Holter-ECG, internal or external event recorder, and exercise-testing are immediately available. Additional investigations, eg, cardiac magnetic resonance imaging, cardiac computed tomography scans, or coronary angiography may be scheduled if necessary. Based on diagnostic results, further treatment strategies may be developed. Since close cooperation is essential, referring physicians and hospitals need to be closely involved in the decision-making process. This includes expedited exchange of results from additional testing.
Patients undergoing device implantation are seen in the outpatient pacemaker clinic, allowing for similar consultation as described for the general arrhythmia clinic.
All patients scheduled for device implantation or an ablation procedure are seen at an outpatient clinic at least one day prior to hospital admission. Informed consent is obtained and all patients undergo screening for possible inclusion in ongoing research studies.
Essential to the concept of an outpatient clinic is the regular follow-up of patients after device implantation or catheter ablation. Patients are scheduled at regular intervals to assess their current status, to perform rhythm analysis and device interrogation, or to discuss further treatment options. To ensure close cooperation with the referring physician, a written assessment of each visit is to be forwarded.
Inpatient StayPatients admitted to the inpatient wards are either undergoing a scheduled EP procedure or device implantation or are directly admitted through the emergency department for further diagnosis and treatment.
Scheduled patients are treated on the day of hospital admission, since preprocedural work-up and patient informed consent is to be obtained during a previous outpatient clinic visit.
Immediately after the invasive EP procedure, patients are transferred to the recovery unit. Noninvasive monitoring as well as transthoracic echocardiography is performed in all patients to rule out a pericardial effusion. Once the patient is completely awake and hemodynamically stable, transfer to the ward is initiated. After complex ventricular tachycardia ablations or procedures performed in general anesthesia, patients generally will be admitted to the intensive care unit for further observation and treatment.
The day after the EP procedure patients undergo echocardiographic screening to rule out a pericardial effusion. Depending on the site of venous access during ablation and routinely in all patients following device implantation, thoracic fluoroscopy is performed to assess for pneumothorax and/or proper lead positioning. Patients are equipped with a Holter monitor to document acute success following pulmonary vein isolation, catheter ablation of ventricular tachycardia, or ventricular or supraventricular premature beats. Duplex echocardiography is performed in cases of suspected groin hematoma, pseudoaneurysm, or arterial-venous fistula. Following device implantation patients will have a final device check prior to discharge.
Generally, patients are discharged the second day after the procedure. The discharge letter includes the operative report, final treatment recommendations including a list of medications, and a scheduled follow-up appointment at the outpatient clinic.
Postdischarge CareClose follow-up of patients who underwent complex ablation procedures or device implantations is necessary and should be provided by the arrhythmia unit. After complex ablation procedures the clinical status must be reassessed and essential follow-up tests such as ECG and Holter monitoring or transthoracic echocardiography have to be performed at regular intervals. Depending on the patient's current clinical status, recommendations regarding antiarrhythmic drug therapy or potential need for a repeat ablation procedure need to be addressed. Adequate postdischarge care guarantees that recent guidelines will be integrated into the treatment concept.
Monitoring the patient after device implantation should not only be restricted to outpatient clinic visits. New technologies like telemonitoring allow for daily and if necessary immediate rhythm analysis. Telemonitoring has the potential to provide an infrastructure that allows for immediate response to patient problems. As soon as serious arrhythmic events occur and are transmitted, the patient and/or physician on call are contacted and further steps can be initiated. This service should be available anytime, including nights, weekends, and public holidays. In addition, patients with implanted devices without telemonitoring capabilities need an immediate contact person always available. Less complex cases may be solved by phone without the need for a clinic visit. In the setting of serious events, eg, multiple implantable cardioverter-defibrillator shocks, patients need to be transferred to the emergency department in order to pursue further diagnosis and treatment. Patients may be monitored and treated on the ward or the intensive care unit. Furthermore, the infrastructure for immediate interventional treatment such as catheter ablation of incessant ventricular tachycardia should be available. To cope with these demands a sophisticated high-quality infrastructure needs to be in place.
CONCLUSIONSCardiac EP is a fast-growing subspecialty of general cardiology. A modern and successful arrhythmia unit relies on highly specialized physicians and nurses and a flexible infrastructure equipped with organizational and technical standards that allow treatment of the full spectrum of cardiac arrhythmias. Physicians should seek training in qualified centers with well-established arrhythmia units and expertise in this complex field of cardiology. Following completion of training as an arrhythmia specialist, it is expected that individuals continue to pursue regular medical education to ensure updated theoretical and practical competency. Sophisticated technical equipment meeting current standards is essential to the treatment of the full spectrum of arrhythmias. While it is crucial to install the most recent technology it is also important to select equipment physicians are acquainted with. A contemporary and practical organizational infrastructure should adhere to highest quality standards. That implies a solid network of referring and cooperating physicians and hospitals, an efficient outpatient clinic as well as wards and intermediate and intensive care units to monitor patients after complex EP procedures. An integral part of a modern arrhythmia unit is appropriate postdischarge care including outpatient clinic visits at regular intervals as well as telemonitoring. Telemonitoring will necessitate an immediate response system in place if acute treatment is indicated.
Future PerspectivesCardiac EP has seen numerous innovative developments over the last decade. New technologies will evolve and further extend the interventional as well as noninterventional armamentarium in EP.
Besides sophisticated technology, modern organizational structures will be essential to run an efficient arrhythmia unit. In addition, its organization depends on a close network of EP laboratories and hospital wards that also includes the recovery room, intensive care unit, and outpatient clinic as well as close collaboration with a cardiac surgery department. This cooperation is facilitated by optimizing accessibility between different organizational sub-units to provide efficient workflows.
In addition to novel mapping and ablation systems aiming to simplify and automate the ablation procedure, technology may allow the use of video transmission to improve quality of care. For example, EP procedures may be performed and transmitted to other centers online. This will enable even less experienced EP centers to perform ablation procedures under the guidance of EP experts. Upcoming questions or peri-interventional challenges could be discussed and solved online.
Telemonitoring will further gain in importance. Regular visits in outpatient clinics may not be required if patients are free of events, and conversely visits may be arranged promptly in case of acute change in symptoms. Additional research in this area is needed and will guide its role in the organizational structure of an arrhythmia unit.
CONFLICTS OF INTERESTNone declared.
Corresponding author: Abteilung für Kardiologie, Lohmühlenstr. 5, 20099 Hamburg, Germany. AndreasMetzner1@web.de