Keywords
INTRODUCTION
Balloon angioplasty of the left main coronary artery (LMCA) has been associated with elevated procedural mortality and with a poor long-term prognosis.1 Therefore, coronary artery bypass surgery has been the treatment of choice for unprotected LMCA lesions,2 while angioplasty has been reserved for patients with high surgical risk factors and when urgent revascularization is required.3-6 With the introduction of stents and improved antiplatelet agents,7 LMCA angioplasty is no longer strictly contraindicated as a possible alternative to surgical treatment in selected patients. The aims of the present study were to analyze the immediate and long-term results obtained at our center using LMCA angioplasty with stent implantation and to identify predictors of mortality.
PATIENTS AND METHOD
Patients
Between November 1997 and March 2003, out of 2790 patients stent implantation was carried out in 38 patients (33 men and 5 women) aged 69±8 years (range, 5085 years) with serious LMCA lesions (1.36%). Table 1 summarizes the clinical characteristics of the study group. At the time of diagnostic angiography, 28 patients (74%) were known to have ischemic heart disease, seven (18%) had early angina, and 3 had valvular heart disease with angina. The mean left ventricular ejection fraction in these patients was 49±8%. However, 3 patients had ejection fractions <30%. The stenotic LMCA lesions were diffuse in 9 patients (23.7%). They were located in the ostium in 3 (7.9%), in the central third of the vessel in 6 (15.8%), and distally in 20 (52.6%). In patients with distal disease, the lesion extended into the left anterior descending coronary artery in 8 cases, into the circumflex artery in 7, and into both in 5. Severe calcification was observed in 6 patients (15%).
Angioplasty was elective in 27 patients and urgent in the remaining 11. Elective revascularization was indicated for unstable angina in patients with defective distal vessels who were not able to undergo repeat surgical intervention or in whom the risk of surgery was high. According to Parsonnet's scale8 for assessing surgical risk, 16 patients were at a high risk (score, >18) and the remaining 11 were at a low-to-moderate risk (score, ≤18). In 4 patients (10%), the stent was implanted because of procedural dissection of the LMCA, without compromising blood flow. In the group of patients undergoing elective treatment, 1 patient exhibited clinical signs of mild heart failure. The group of patients undergoing urgent treatment included those with acute myocardial infarction (AMI); 5 (45%) were in Killip class I or II and the remaining 6 (55%) were in Killip class III or IV. The left coronary circulation was unprotected in 23 patients (60.5%): 12 (44.4%) in the elective treatment group and 11 (100%) in the urgent treatment group.
Description of Angioplasty
In all patients, the vessel was accessed via the femoral artery. Size 6 Fr angioplasty catheters were used. Before carrying out the procedure, heparin sodium, at a dose of 100 mg/kg, was administered. In 8 patients (21%), an abciximab bolus, 0.25 mg/kg, was given with subsequent continuous perfusion for 12 hours.
In 30 patients (79%), the lesions were predilated using a conventional balloon catheter whose diameter was less than that of the reference segment and which was inflated to the pressure needed to obtain the required degree of distention. In 7 patients (18%), the stent was implanted without predilatation. In 1 patient who had a severely calcified lesion, it was necessary to predilate using a cutting balloon. Then, the stent was placed in the lesion and, after its position had been confirmed by angiography, the balloon was inflated for <30 s. The maximum inflation pressure was 12±2 atm (range, 916 atm). In all cases, a tubular stent was implanted. The median diameter and length of the stents were 3.7±2.6 mm and 14±4 mm, respectively. After stent deployment, at least 2 orthogonal images were obtained to verify the result achieved. In cases in which results were considered to be suboptimal, further dilatation was carried out using the same balloon at a higher inflation pressure or using a larger diameter, less distensible balloon inflated at a high pressure. In the eight patients who had LMCA lesions that extended into the left anterior descending coronary artery, the stent was positioned from the LCA into the left anterior descending coronary artery. In 2 cases, after stent placement, it was necessary to dilate the root of the circumflex artery due to plaque shifting; in 1 patient, following dilatation, a stent had to be passed through the LMCA stent. Both the LMCA and the circumflex artery were affected in 7 patients. In 5 of them, the stent was implanted into the circumflex artery via the LMCA (with the proximal left anterior descending coronary artery occluded and distal vessel filling taking place via a bypass graft). In the other 2 patients, a double stent was used. In 3 of the 5 patients in whom the roots of both arterial branches were affected, a double stent was implanted after simultaneous predilatation of both arteries; in the other 2 patients, in whom there was diffuse disease and the circumflex artery was less important, only stents from the LMCA to the left anterior descending coronary artery were used.
After angioplasty, 35 patients were treated with 2 antiplatelet agents (i.e., acetylsalicylic acid with ticlopidine or clopidogrel). Three patients who had valve prostheses were treated with an antiplatelet agent and acenocoumarol. In 9 patients, intra-aortic balloon counterpulsation was used.
Follow-up
All patients were followed up clinically for a mean of 25±20 months (range, 468 months) after the procedure by undergoing detailed questioning in a cardiology clinic.
Definitions
Angioplasty was considered completed successfully when the residual lesion was <20%. Deaths were classified as cardiac or non-cardiac. The following were considered as serious complications: death, the need for urgent surgery, and AMI, including non-transmural AMI. Non-transmural AMI were defined when the total creatine kinase level was double the reference level, with positive MB fraction and absence of pathological Q waves. Recurrent angina, AMI, death, and the need for revascularization were considered as major clinical events at follow-up. When the cause of death was unknown, it was assumed to be cardiac.
Angiographic Analysis
The reference diameter, the minimum lumen diameter, and the percentage of diameter stenosis were quantified before and after stent implantation using an automated digital angiographic analysis system employing edge-detection (Integris HM3000. Philips Medical Systems, the Netherlands).
Statistical Analysis
Statistical analysis was carried out using the following computer programs: SPSS version 10 and STATISTICA version 5. Results are expressed as means ± standard deviations. Comparisons of categorical variables were made using the χ² test. Kaplan-Meier analysis was used to calculate the accumulated survival probability and the accumulated cardiac event-free survival probability.
RESULTS
Angioplasty was successful in all patients. However, 1 patient who was admitted with a myocardial infarction in Killip class IV and in whom a stent had already been implanted died in the catherization laboratory as a result of the no-reflow phenomenon and heart failure. In addition to being placed in the LMCA, stents were also implanted in the left anterior descending coronary artery in 8 patients (21%), in the circumflex artery in 6 (15%), in both epicardial arteries in 5 (13%), and in the right coronary artery in 1 (2%). No patient was referred for coronary revascularization surgery.
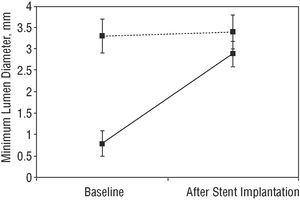
Before angioplasty, the mean percentage of diameter stenosis of the LMCA was 84%±15%; after stent implantation, it had been reduced to 17%±11% (P<.005). Figure 1 shows the mean reference and minimum lumen diameters before and after treatment.
Fig. 1. The dashed line above shows the reference diameter. The solid line below illustrates the increase in minimum lumen diameter produced by stent implantation.
Four patients (10%) suffered major complications, which comprised non-transmural AMIs without hemodynamic sequelae.
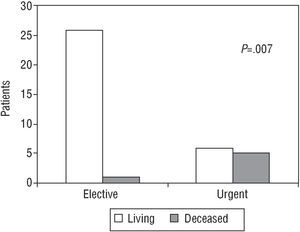
Mortality during hospitalization was 15.8% (i.e., 6 of 38 patients). In the urgent-treatment group, 5 of 11 patients (45.4%) who presented with an AMI complicated by severe heart failure (Killip class III or IV) died in the hospital, compared with 1 of 27 patients (3.7%) in the elective-treatment group (P=.007) (Figure 2). This last patient, who was at a low risk according to Parsonnet's classification, died because of a pulmonary hemorrhage that was attributed to treatment with platelet glycoprotein IIb/IIIa receptor inhibitors. There was no correlation between mortality and age, sex, or the presence of diabetes, probably because the sample size was small (Table 2). No patient died in the hospital from a malignant arrhythmia or from subacute stent thrombosis.
Fig. 2. Mortality during hospitalization in the elective-treatment and urgent-treatment groups.
During follow-up, 5 patients (13%) presented with major clinical events. Three patients who had unprotected LMCA died: 2 had an AMI in the first few months following angioplasty and 1 experienced sudden death. The other 2 of the 5 patients presented with recurrent angina and were successfully redilated. No patient was referred for surgery. One other patient died from an ischemic stroke 2 months after angioplasty.
After analyzing how the presence of a patent left coronary artery bypass graft affected overall cardiac mortality, we found that 9 of the 23 patients (39.1%) who had an unprotected LMCA died (6 during hospitalization and 3 during follow-up). In contrast, none of the 15 patient with a protected LMCA died (P=.01).
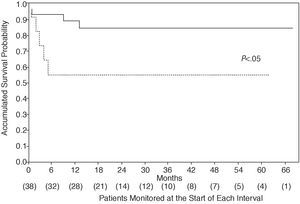
Total mortality in the elective-treatment group was 15% and in the urgent-treatment group, 45%. The accumulated survival probability in the elective-treatment group was 92%±0.5%, 88%±0.6%, and 86%±0.7% at 6 months, 1 year and 3 years, respectively. In contrast, at 6 months the probability in the urgent-treatment group was 54%±0.2% (P<.05) (Figure 3).
Fig. 3. Accumulated survival probability in the elective-treatment group (solid line) compared with the urgent-treatment group (dotted line). Urgent treatment was associated with greater mortality, which generally occurred during the first 6 months following angioplasty.
DISCUSSION
Conventional balloon angioplasty of the LMCA is associated with increased medium and long term mortality. In O'Keefe et al's series,1 mortality during treatment in patients undergoing elective angioplasty who did or did not have a protected LMCA was 4.3% and 9.1% in the 2 subgroups, respectively. Mortality at 20 months was 65%. Traditionally, therefore, conventional LMCA angioplasty has been restricted to patients for whom surgery is a high-risk procedure and to those who need urgent treatment. In addition, the phenomenon of elastic recoil occurs more frequently with LMCA angioplasty because of the preponderance of elastic fibers in arterial walls.5 The introduction of stents has revolutionized the treatment of coronary artery disease and has increased the number of indications for LMCA angioplasty. The main beneficial effects of stents are that they reduce the risk of acute occlusion, inhibit elastic recoil of the arterial wall, and decrease the rate of restenosis.9 In the present study, we found that LMCA angioplasty with stent implantation was a safe and effective procedure in selected patients with protected LMCA undergoing elective treatment. However, mortality was elevated in those with unprotected LMCA who were undergoing urgent procedures and who had an AMI with signs of left ventricular dysfunction.
As observed in other studies,1013 in the present study the angiographic success rate during angioplasty was 100%. Nevertheless, 1 patient died from an AMI and cardiogenic shock despite the artery being made patent again. In the present series, we found that elective angioplasty was associated with good immediate and long-term results. In our group, only 1 patient died. Death was due to pulmonary hemorrhage that was attributed to treatment with platelet glycoprotein IIb/IIIa receptor inhibitors. Total mortality in the elective-treatment group was 15%. In Park et al's series,10 composed of 42 patients with similar characteristics, the recurrence rate of angina and restenosis was 17% and 22%, respectively. Only 1 patient died during coronary artery bypass surgery carried out because of in-stent restenosis. These favorable results were obtained because the study involved selected patients with protected LMCA and preserved ventricular function.
In our series, total mortality in the urgent-treatment group was 45%. This high rate occurred because our group principally comprised patients who were admitted with an AMI and who were in a precarious clinical condition. It is important to note that, in all cases, the LMCA was unprotected. This factor determines both short-term and long-term prognosis, irrespective of whether patients are undergoing elective or urgent treatment.13-15 In our series, all the patients who died had an unprotected LMCA. In contrast, not one patient who had a protected LMCA died. In the ULTIMA multicenter registry,14 which included 17 patients who underwent stent implantation in an unprotected LMCA because of an AMI, the in-hospital mortality rate was 53% and the 12-month rate of either mortality or the need for surgery was 58%. In our study, the majority of patients with an AMI and severe ventricular dysfunction (i.e., Killip class III or IV) who underwent angioplasty died during hospitalization despite successful revascularization. In these patients, the cause of death was progressively deteriorating heart failure. In a multicenter study carried out by Ellis et al in patients with unprotected LMCA, ventricular dysfunction was found to be the most important predictor of mortality.15 In agreement with other authors,14,15 we observed that the incidence of death in this subgroup of patients was highest over the short term (i.e., <6 months). These findings clearly demonstrate that the ventricle cannot tolerate extensive acute myocardial ischemia, even for a short time. In this situation, the early application of techniques such as intra-aortic balloon counterpulsation and, especially, cardiopulmonary support could help increase the survival rate. However, these techniques are not always available and specialized qualified personnel are required, as is optimal coordination with the catherization laboratory.
The present study did not include angiographic follow-up. The repeat percutaneous revascularization rate was 7% (i.e., in 2 of 29 patients). In contrast to reports of other series,13 no patient was referred for surgery in the present study. However, it is important to stress that restenosis manifested as sudden death and fatal AMI in 3 patients, all of whom were undergoing elective treatment and had unprotected LMCA. Consequently, in patients with LMCA stents, it is advisable to monitor their clinical condition regularly during the first few months after angioplasty. In addition, it has been suggested that angiographi c studies should be carried out early, between 6 and 16 weeks following angioplasty, to detect rapidly developing restenosis.15,16 However, the actual benefit of angiography in this context has not been established. The use of stents coated with antiproliferative agents, which have recently become available on the market, could help reduce cardiac event and revascularization rates during follow-up.17,18
The main limitations of the present series are that it was a non-randomized study and that there was no angiographic follow-up. In addition, the small size of the patient sample could have contributed to our inability to identify factors indicating a poor prognosis, such as advanced age, the presence of diabetes mellitus, low ejection fraction, or extensive coronary disease.9,19 Although findings published in the medical literature, especially in patients undergoing elective treatment, have encouraged an increase in indications for LMCA angioplasty, randomized controlled studies are needed before the technique can be recommended as an alternative treatment for those without contraindications to surgery. It should be emphasized that patients who are good candidates for revascularization surgery are usually also good candidates for angioplasty. Therefore, those for whom angioplasty is appropriate must be carefully selected. In patients undergoing elective angioplasty, results are more favorable when the lesion is not bifurcated and the LMCA is relatively long than when the lesion affects a short LMCA and involves the bifurcation.20 In patients with AMI in cardiogenic shock, angioplasty is probably the only therapeutic option despite the poor results.
In conclusion, LMCA angioplasty with stent implantation is a safe procedure in selected patients. Elective angioplasty in individuals with a protected LMCA is associated with a relatively low incidence of major cardiac events. The principal risk factors associated with a poor prognosis in patients undergoing urgent treatment are AMI, clinical signs of ventricular dysfunction, and an unprotected LMCA.
See editorial on pages 1009-13
Correspondence: Dr. V. Martí.
Unidad de Hemodinámica y Cardiología Intervencionista.
Hospital de la Santa Creu i Sant Pau
Avda. Sant Antoni Maria Claret, 167. 08025 Barcelona. España.
E-mail: 18461vmc@comb.es