To evaluate the impact of 2 smoking bans enacted in 2006 (partial ban) and 2011 (comprehensive ban) on hospitalizations for cardiovascular disease in the Spanish adult population.
MethodsThe study was performed in 14 provinces in Spain. Hospital admission records were collected for acute myocardial infarction (AMI), ischemic heart disease (IHD), and cerebrovascular disease (CVD) in patients aged ≥ 18 years from 2003 through 2012. We estimated immediate and 1-year effects with segmented-linear models. The coefficients for each province were combined using random-effects multivariate meta-analysis models.
ResultsOverall, changes in admission rates immediately following the implementation of the partial ban and 1 year later were –1.8% and +1.2% for AMI, +0.1 and +0.4% for IHD, and +1.0% and +2.8% for CVD (P>.05). After the comprehensive ban, immediate changes were –2.3% for AMI, –2.6% for IHD, and –0.8% for CVD (P>.05), only to return to precomprehensive ban values 1 year later. For patients aged ≥ 65 years of age, immediate changes associated with the comprehensive ban were –5.0%, –3.9%, and –2.3% for AMI, IHD, and CVD, respectively (P<.05). Again, the 1-year changes were not statistically significant.
ConclusionsIn Spain, smoking bans failed to significantly reduce hospitalizations for AMI, IHD, or CVD among patients ≥ 18 years of age. In the population aged ≥ 65 years, hospital admissions due to these diseases showed significant decreases immediately after the implementation of the comprehensive ban, but these reductions disappeared at the 1-year evaluation.
Keywords
Considerable evidence shows that exposure to environmental tobacco smoke (ETS) has marked adverse effects on the cardiovascular system, inducing a rapid increase in risks, even with low levels of exposure.1
Numerous studies have examined the effects of smoke-free legislation on cardiovascular health, with their findings summarized in various meta-analyses.2–7 The most recent2 evaluated the impact of these laws on the incidence of ischemic heart disease (IHD) and acute myocardial infarction (AMI) in 43 studies performed in 21 countries and found a reduction in coronary heart disease in 33 of the studies. The evidence on cerebrovascular disease (CVD) is more limited, with reductions in its incidence detected in 4 of the 6 studies included in the review.2
Spain is one of the few countries to successively introduce laws regulating smoke-free spaces. On January 1st, 2006, a smoking ban (Law 28/2005) came into force that completely prohibited smoking at work, but not in hospitality venues, where partial restrictions were applied according to the size of the premises. This law markedly reduced ETS exposure in the workplace but had little impact on the hospitality sector.8–10 In January 2011, the previous legislation was reformed, and tobacco consumption was prohibited in practically all public spaces, which dramatically reduced ETS exposure in bars and restaurants.11
In Spain, 3 studies have analyzed the impact of the first law on admissions for AMI: 2 detected a significant decrease (in the province of Girona and in the city of Barcelona),12,13 whereas the third failed to find significant changes in the cities of Madrid and Barcelona.14 Regarding hospitalizations for CVD, 1 study performed in the cities of Madrid and Barcelona found no changes in Madrid but a significant decrease in Barcelona.14 This variability indicates the importance of analyzing all regions, or at least a large sample, when the objective is to evaluate the impact of smoking bans on an entire country.15
The aim of this study was to assess the impact of the 2 smoking bans on hospital admissions for coronary heart disease and CVD in a broad sample of the Spanish population.
METHODSStudy Population and Data SourcesThe study was performed in the 14 Spanish provinces with the largest number of inhabitants (Table 1), with a mean population of 28 326 480. Data were collected from the hospitalization records of the Minimum Basic Data Set from January 2003 to November 2012. The number of daily emergency admissions for AMI (International Classification of Diseases, Ninth Edition [ICD-9] 410.x.0 and 410.x.1), IHD (ICD-9 410-414), and CVD (ICD-9 430-438) were analyzed in persons ≥ 18 years.
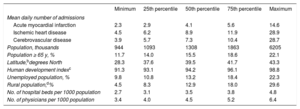
Description of the Daily Number of Emergency Admissions for Cardiovascular Disease and the Sociodemographic Characteristics of the 14 Included Provincesa From 2003 to 2012
| Minimum | 25th percentile | 50th percentile | 75th percentile | Maximum | |
|---|---|---|---|---|---|
| Mean daily number of admissions | |||||
| Acute myocardial infarction | 2.3 | 2.9 | 4.1 | 5.6 | 14.6 |
| Ischemic heart disease | 4.5 | 6.2 | 8.9 | 11.9 | 28.9 |
| Cerebrovascular disease | 3.9 | 5.7 | 7.3 | 10.4 | 28.7 |
| Population, thousands | 944 | 1093 | 1308 | 1863 | 6205 |
| Population ≥ 65 y, % | 11.7 | 14.0 | 15.5 | 18.6 | 22.1 |
| Latitude,bdegrees North | 28.3 | 37.6 | 39.5 | 41.7 | 43.3 |
| Human development indexc | 91.3 | 93.1 | 94.2 | 96.1 | 98.8 |
| Unemployed population, % | 9.8 | 10.8 | 13.2 | 18.4 | 22.3 |
| Rural population,d% | 4.5 | 8.3 | 12.9 | 18.0 | 29.6 |
| No. of hospital beds per 1000 population | 2.7 | 3.1 | 3.5 | 3.8 | 4.8 |
| No. of physicians per 1000 population | 3.4 | 4.0 | 4.5 | 5.2 | 6.4 |
In each of the provinces, changes in the hospital admission rates after implementation of the 2006 and 2011 laws were estimated using additive Poisson models with overdispersion, adjusted for the main covariates. To estimate both the immediate and gradual effects,16 the specific admission rates per province were analyzed using segmented log-linear models, with differentiation of the linear trends in the 2003 to 2005 (before the first law), 2006 to 2010 (partial ban), and 2011 to 2012 (comprehensive ban) periods. The associations were summarized for each province through an estimation of 4 coefficients: 2 representing the immediate changes in hospital admissions after implementation of the partial and comprehensive bans and 2 representing the changes in the slope of admissions during the partial ban period vs the period before the ban, and the change in the slope of the comprehensive ban period vs the partial ban period while calculating the percentages of the changes 1 year after the implementation of both regulations.
The adjustment variables were as follows: a) sine and cosine harmonic terms for seasonal variations with annual and semiannual periods17; b) indicators for days of the week; c) smoothed functions of the maximum temperature (from the Spanish State Meteorological Agency); d) influenza (from the Spanish Influenza Surveillance System); and e) acute respiratory infections (from the Minimum Basic Data Set), which were averaged for each day and the 2 previous days. The smoothed functions of these variables were estimated using thin plate splines penalized with a maximum of 3 degrees of freedom.18
To evaluate the potential heterogeneity of the effect of the bans according to age and sex, a separate analysis was performed at the provincial level for men and women, as well as for individuals aged 18 to 64 years and ≥ 65 years. All models were estimated using penalized “quasilikelihood” methods, implemented in the “gam” function of the “mgcv” package of R (R Foundation for Statistical Computing, Vienna, Austria).
Aggregate AnalysesThe coefficients estimated for each province were pooled using random-effects multivariate meta-analysis models for correlated outcomes.19,20 Subsequently, the pooled percentage changes were estimated to quantify the effect at the implementation of Law 28/2005 and 1 year later and the ratio of the pooled rates was calculated for these periods vs the projected rates from the period before the law.16 Similarly, the pooled associations between the implementation of Law 42/2010 and 1 year later were estimated as the ratio of the pooled rates for these periods vs the projected rates for the 2006 to 2010 period (Law 28/2005).
To explore potential differences in the association at the provincial level, the following predictive variables were analyzed: latitude, human development index (a synthetic index comprising life expectancy, education, and per capita income), the unemployment rate, percentage rural population (< 10 000 inhabitants), and number of hospital beds and physicians per 1000 population. In each province, these variables were included in specific random-effects multivariate metaregression models.19 Effect modifications of the pooled associations for the provincial characteristics were tested using a likelihood ratio and nested models were compared with and without the predictive variable.
Heterogeneity was estimated using the multivariate extension of the chi-square test and Cochran test and quantified with the I2 statistic.19,20 These analyses were performed using maximum likelihood methods with the “mvmeta” package of R (R Foundation for Statistical Computing).
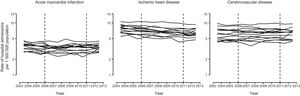
RESULTSIn the study period, there were 279 452 emergency hospital admissions for AMI, 574 302 for IHD, and 520 794 for CVD in the 14 provinces included in the study (Table 1). The daily admissions in each province during the study period can be seen in Figure 1.
Daily hospital admissions for cardiovascular disease in 14 Spanish provinces from 2003 to 2012. Mean daily admission rate for each year, estimated using additive Poisson models with overdispersion and adjusted for the main covariates. The vertical lines represent the implementation dates of the partial and comprehensive bans.
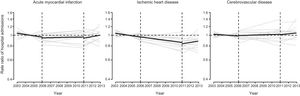
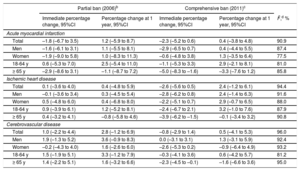
The segmented linear trends in the hospital admission rates during the period before the law, with the partial ban, and with the comprehensive ban varied widely among the 14 studied provinces (I2=90.9% for AMI, 94.4% for IHD, and 96.0% for CVD; all P < .001) (, ). The pooled segmented trends for all of the provinces are described in Figure 2, and the corresponding changes in the admission rates are summarized in Table 2. The pooled changes in the admission rates with the implementation of Law 28/2005 and 1 year later were –1.8% and+1.2% for AMI,+0.1% and 0.4% for IHD, and+1.0% and+2.8% for CVD (all P > .05). The comprehensive ban induced slight but nonsignificant immediate changes, with reductions of 2.3% in AMI, 2.6% in IHD, and 0.8% in CVD; these changes were no longer evident at 1 year (Table 2).
Segmented linear trends, pooled and at the provincial level, for the rate ratio of hospital admissions for cardiovascular diseases in 14 Spanish provinces from 2003 to 2012. The segmented linear trends at the provincial level (gray lines) were estimated using additive Poisson models with overdispersion and adjusted for the main covariates. The vertical lines represent the implementation dates of the partial and comprehensive bans. The pooled linear segments (black line) were estimated using random-effects multivariate meta-analysis models.
Changes in Hospital Admissions for Cardiovascular Diseases at Implementation and 1 Year After the Partial Ban of 2006 and the Comprehensive Ban of 2011 From 2003 to 2012a
| Partial ban (2006)b | Comprehensive ban (2011)c | ||||
|---|---|---|---|---|---|
| Immediate percentage change, 95%CI | Percentage change at 1 year, 95%CI | Immediate percentage change, 95%CI | Percentage change at 1 year, 95%CI | I2,d % | |
| Acute myocardial infarction | |||||
| Total | –1.8 (–6.7 to 3.5) | 1.2 (–5.9 to 8.7) | –2.3 (–5.2 to 0.6) | 0.4 (–3.8 to 4.8) | 90.9 |
| Men | –1.6 (–6.1 to 3.1) | 1.1 (–5.5 to 8.1) | –2.9 (–6.5 to 0.7) | 0.4 (–4.4 to 5.5) | 87.4 |
| Women | –1.9 (–9.0 to 5.8) | 1.0 (–8.3 to 11.3) | –0.6 (–4.8 to 3.8) | 1.3 (–3.5 to 6.4) | 77.5 |
| 18-64 y | 0.6 (–5.3 to 7.0) | 2.5 (–5.4 to 11.0) | –1.1 (–5.3 to 3.3) | 2.9 (–2.1 to 8.1) | 81.0 |
| ≥ 65 y | –2.9 (–8.6 to 3.1) | –1.1 (–8.7 to 7.2) | –5.0 (–8.3 to –1.6) | –3.3 (–7.6 to 1.2) | 85.8 |
| Ischemic heart disease | |||||
| Total | 0.1 (–3.6 to 4.0) | 0.4 (–4.8 to 5.9) | –2.6 (–5.6 to 0.5) | 2.4 (–1.2 to 6.1) | 94.4 |
| Men | –0.1 (–3.6 to 3.4) | 0.3 (–4.5 to 5.4) | –2.8 (–6.2 to 0.8) | 2.4 (–1.4 to 6.3) | 91.6 |
| Women | 0.5 (–4.8 to 6.0) | 0.4 (–6.8 to 8.0) | –2.2 (–5.1 to 0.7) | 2.9 (–0.7 to 6.5) | 88.0 |
| 18-64 y | 0.9 (–3.9 to 6.1) | 1.2 (–5.2 to 8.1) | –2.4 (–6.7 to 2.1) | 3.2 (–1.0 to 7.6) | 87.9 |
| ≥ 65 y | 0.4 (–3.2 to 4.1) | –0.8 (–5.8 to 4.6) | –3.9 (–6.2 to –1.5) | –0.1 (–3.4 to 3.2) | 90.8 |
| Cerebrovascular disease | |||||
| Total | 1.0 (–2.2 to 4.4) | 2.8 (–1.2 to 6.9) | –0.8 (–2.9 to 1.4) | 0.5 (–4.1 to 5.3) | 96.0 |
| Men | 1.9 (–1.3 to 5.2) | 3.6 (–0.9 to 8.3) | 0.0 (–3.1 to 3.1) | 1.3 (–3.1 to 5.9) | 92.4 |
| Women | –0.2 (–4.3 to 4.0) | 1.6 (–2.6 to 6.0) | –2.6 (–5.3 to 0.2) | –0.9 (–6.4 to 4.9) | 93.2 |
| 18-64 y | 1.5 (–1.9 to 5.1) | 3.3 (–1.2 to 7.9) | –0.3 (–4.1 to 3.6) | 0.6 (–4.2 to 5.7) | 81.2 |
| ≥ 65 y | 1.4 (–2.2 to 5.1) | 1.6 (–3.2 to 6.6) | –2.3 (–4.5 to –0.1) | –1.6 (–6.6 to 3.6) | 95.0 |
95%CI, 95% confidence interval.
Pooled estimates from the 14 included provinces. The specific estimates from each province were obtained from additive Poisson models with overdispersion while differentiating linear segments for the periods before the first ban (2003-2005), the partial ban (2006-2010), and the comprehensive ban (2011-2012). The specific estimates for each province were pooled using random-effects multivariate meta-analysis models.
Pooled estimates and 95%CI values at the time of implementation of the partial ban and 1 year later vs the trend estimated during the period prior to the law (2003-2005).
There were no significant differences according to sex. The reductions in admissions associated with the comprehensive ban were higher in the population aged ≥ 65 years, with immediate decreases of 5.0% in AMI, 3.9% in IHD, and 2.3% in CVD (all P < .05), although these changes were no longer significant at 1 year (Table 2).
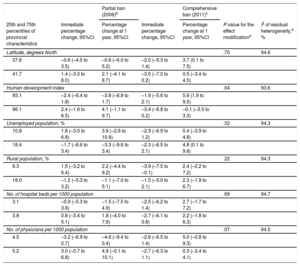
Aggregate Effects According to Provincial CharacteristicsThe aggregate changes in hospital admission rates according to the characteristics of the provinces are shown in Table 3, Table 4, and Table 5. Significant effect modifications of the bans on admissions for IHD were seen according to the human development index (P=.04). In provinces with a lower human development index, the rates decreased by 2.4% and 3.8% at implementation of the partial law and 1 year later, whereas those with a higher development index showed increases of 2.4% and 4.1%, respectively.
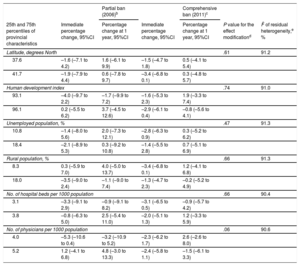
Percentage Changes in Hospital Admissions for Acute Myocardial Infarction at Implementation of the Partial Ban of 2006 and the Comprehensive Ban of 2011 and 1 Year Later According to the Characteristics of the 14 Included Provinces for the 2003 to 2012 perioda
| Partial ban (2006)b | Comprehensive ban (2011)c | |||||
|---|---|---|---|---|---|---|
| 25th and 75th percentiles of provincial characteristics | Immediate percentage change, 95%CI | Percentage change at 1 year, 95%CI | Immediate percentage change, 95%CI | Percentage change at 1 year, 95%CI | P value for the effect modificationd | I2 of residual heterogeneity,e % |
| Latitude, degrees North | .61 | 91.2 | ||||
| 37.6 | –1.6 (–7.1 to 4.2) | 1.6 (–6.1 to 9.9) | –1.5 (–4.7 to 1.8) | 0.5 (–4.1 to 5.4) | ||
| 41.7 | –1.9 (–7.9 to 4.4) | 0.6 (–7.8 to 9.7) | –3.4 (–6.8 to 0.1) | 0.3 (–4.8 to 5.7) | ||
| Human development index | .74 | 91.0 | ||||
| 93.1 | –4.0 (–9.7 to 2.2) | –1.7 (–9.9 to 7.2) | –1.6 (–5.3 to 2.3) | 1.9 (–3.3 to 7.4) | ||
| 96.1 | 0.2 (–5.5 to 6.2) | 3.7 (–4.5 to 12.6) | –2.9 (–6.1 to 0.4) | –0.8 (–5.6 to 4.1) | ||
| Unemployed population, % | .47 | 91.3 | ||||
| 10.8 | –1.4 (–8.0 to 5.6) | 2.0 (–7.3 to 12.1) | –2.8 (–6.3 to 0.9) | 0.3 (–5.2 to 6.2) | ||
| 18.4 | –2.1 (–8.9 to 5.3) | 0.3 (–9.2 to 10.8) | –1.4 (–5.5 to 2.8) | 0.7 (–5.1 to 6.9) | ||
| Rural population, % | .66 | 91.3 | ||||
| 8.3 | 0.3 (–5.9 to 7.0) | 4.0 (–5.0 to 13.7) | –3.4 (–6.8 to 0.1) | 1.2 (–4.1 to 6.8) | ||
| 18.0 | –3.5 (–9.0 to 2.4) | –1.1 (–9.0 to 7.4) | –1.3 (–4.7 to 2.3) | –0.2 (–5.2 to 4.9) | ||
| No. of hospital beds per 1000 population | .66 | 90.4 | ||||
| 3.1 | –3.3 (–9.1 to 2.9) | –0.9 (–9.1 to 8.2) | –3.1 (–6.5 to 0.5) | –0.9 (–5.7 to 4.2) | ||
| 3.8 | –0.8 (–6.3 to 5.0) | 2.5 (–5.4 to 11.0) | –2.0 (–5.1 to 1.3) | 1.2 (–3.3 to 5.9) | ||
| No. of physicians per 1000 population | .06 | 90.6 | ||||
| 4.0 | –5.3 (–10.6 to 0.4) | –3.2 (–10.9 to 5.2) | –2.3 (–6.2 to 1.7) | 2.6 (–2.6 to 8.0) | ||
| 5.2 | 1.2 (–4.1 to 6.8) | 4.8 (–3.0 to 13.3) | –2.4 (–5.8 to 1.1) | –1.5 (–6.1 to 3.3) | ||
95%CI, 95% confidence interval.
Pooled estimates for the provincial characteristics were obtained via random-effects multivariate meta-analysis models relating provincial segmented regression coefficients with the values of their corresponding characteristics as a continuous individual covariate.
Pooled estimates and 95%CI values at the time of implementation of the partial ban and 1 year later vs the trend estimated during the period prior to the law (2003-2005) for the 25th and 75th percentiles of the provincial characteristics.
Pooled estimates and 95%CI values at the time of implementation of the comprehensive ban and 1 year later vs the trend estimated during the partial ban period (2006-2010) for the 25th and 75th percentiles of the provincial characteristics.
Percentage Changes in Hospital Admissions for Ischemic Heart Disease at Implementation of the Partial Ban of 2006 and the Comprehensive Ban of 2011 and 1 Year Later According to the Characteristics of the 14 Included Provinces From 2003 to 2012a
| Partial ban (2006)b | Comprehensive ban (2011)c | |||||
|---|---|---|---|---|---|---|
| 25th and 75th percentiles of provincial characteristics | Immediate percentage change, 95%CI | Percentage change at 1 year, 95%CI | Immediate percentage change, 95%CI | Percentage change at 1 year, 95%CI | P value for the effect modificationd | I2 of residual heterogeneity,e % |
| Latitude, degrees North | .70 | 94.6 | ||||
| 37.6 | –0.6 (–4.5 to 3.5) | –0.6 (–6.0 to 5.2) | –2.0 (–5.3 to 1.4) | 3.7 (0.1 to 7.5) | ||
| 41.7 | 1.4 (–3.0 to 6.0) | 2.1 (–4.1 to 8.7) | –3.5 (–7.0 to 0.2) | 0.5 (–3.4 to 4.5) | ||
| Human development index | .04 | 93.6 | ||||
| 93.1 | –2.4 (–6.4 to 1.8) | –3.8 (–8.9 to 1.7) | –1.9 (–5.6 to 2.1) | 5.6 (1.9 to 9.5) | ||
| 96.1 | 2.4 (–1.6 to 6.5) | 4.1 (–1.1 to 9.7) | –3.4 (–6.8 to 0.2) | –0.1 (–3.5 to 3.3) | ||
| Unemployed population, % | .32 | 94.3 | ||||
| 10.8 | 1.8 (–3.0 to 6.8) | 3.9 (–2.6 to 10.8) | –2.9 (–6.9 to 1.2) | 0.4 (–3.9 to 4.8) | ||
| 18.4 | –1.7 (–6.6 to 3.4) | –3.3 (–9.6 to 3.4) | –2.3 (–6.5 to 2.1) | 4.8 (0.1 to 9.8) | ||
| Rural population, % | .22 | 94.3 | ||||
| 8.3 | 1.5 (–3.2 to 6.4) | 2.2 (–4.4 to 9.2) | –3.9 (–7.5 to –0.1) | 2.4 (–2.2 to 7.2) | ||
| 18.0 | –1.2 (–5.3 to 3.2) | –1.1 (–7.0 to 5.1) | –1.5 (–5.0 to 2.1) | 2.3 (–1.9 to 6.7) | ||
| No. of hospital beds per 1000 population | .69 | 94.7 | ||||
| 3.1 | –0.9 (–5.3 to 3.8) | –1.5 (–7.5 to 4.9) | –2.5 (–6.2 to 1.4) | 2.7 (–1.7 to 7.2) | ||
| 3.8 | 0.8 (–3.4 to 5.1) | 1.8 (–4.0 to 7.9) | –2.7 (–6.1 to 0.8) | 2.2 (–1.8 to 6.3) | ||
| No. of physicians per 1000 population | .07 | 94.0 | ||||
| 4.0 | –3.2 (–6.9 to 0.7) | –4.6 (–9.4 to 0.4) | –2.6 (–6.5 to 1.4) | 5.0 (–0.8 to 9.3) | ||
| 5.2 | 3.0 (–0.7 to 6.8) | 4.9 (–0.1 to 10.1) | –2.7 (–6.3 to 1.1) | 0.3 (–3.4 to 4.1) | ||
95%CI, 95% confidence interval.
Pooled estimates for the provincial characteristics were obtained via random-effects multivariate meta-analysis models relating provincial segmented regression coefficients with the values of their corresponding characteristics as a continuous individual covariate.
Pooled estimates and 95%CI values at the time of implementation of the partial ban and 1 year later vs the trend estimated during the period prior to the law (2003-2005) for the 25th and 75th percentiles of the provincial characteristics.
Pooled estimates and 95%CI values at the time of implementation of the comprehensive ban and 1 year later vs the trend estimated during the partial ban period (2006-2010) for the 25th and 75th percentiles of the provincial characteristics.
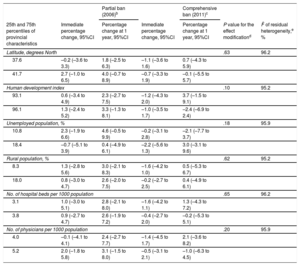
Percentage Changes in Hospital Admissions for Cerebrovascular Disease at Implementation of the Partial Ban of 2006 and the Comprehensive Ban of 2011 and 1 Year Later According to the Characteristics of the 14 Included Provinces From 2003 to 2012a
| Partial ban (2006)b | Comprehensive ban (2011)c | |||||
|---|---|---|---|---|---|---|
| 25th and 75th percentiles of provincial characteristics | Immediate percentage change, 95%CI | Percentage change at 1 year, 95%CI | Immediate percentage change, 95%CI | Percentage change at 1 year, 95%CI | P value for the effect modificationd | I2 of residual heterogeneity,e % |
| Latitude, degrees North | .63 | 96.2 | ||||
| 37.6 | –0.2 (–3.6 to 3.3) | 1.8 (–2.5 to 6.3) | –1.1 (–3.6 to 1.6) | 0.7 (–4.3 to 5.9) | ||
| 41.7 | 2.7 (–1.0 to 6.5) | 4.0 (–0.7 to 8.9) | –0.7 (–3.3 to 1.9) | –0.1 (–5.5 to 5.7) | ||
| Human development index | .10 | 95.2 | ||||
| 93.1 | 0.6 (–3.4 to 4.9) | 2.3 (–2.7 to 7.5) | –1.2 (–4.3 to 2.0) | 3.7 (–1.5 to 9.1) | ||
| 96.1 | 1.3 (–2.4 to 5.2) | 3.3 (–1.3 to 8.1) | –1.0 (–3.5 to 1.7) | –2.4 (–6.9 to 2.4) | ||
| Unemployed population, % | .18 | 95.9 | ||||
| 10.8 | 2.3 (–1.9 to 6.6) | 4.6 (–0.5 to 9.9) | –0.2 (–3.1 to 2.8) | –2.1 (–7.7 to 3.7) | ||
| 18.4 | –0.7 (–5.1 to 3.9) | 0.4 (–4.9 to 6.1) | –2.2 (–5.6 to 1.3) | 3.0 (–3.1 to 9.6) | ||
| Rural population, % | .62 | 95.2 | ||||
| 8.3 | 1.3 (–2.8 to 5.6) | 3.0 (–2.1 to 8.3) | –1.6 (–4.2 to 1.0) | 0.5 (–5.3 to 6.7) | ||
| 18.0 | 0.8 (–3.0 to 4.7) | 2.6 (–2.0 to 7.5) | –0.2 (–2.7 to 2.5) | 0.4 (–4.9 to 6.1) | ||
| No. of hospital beds per 1000 population | .65 | 96.2 | ||||
| 3.1 | 1.0 (–3.0 to 5.1) | 2.8 (–2.1 to 8.0) | –1.6 (–4.2 to 1.1) | 1.3 (–4.3 to 7.2) | ||
| 3.8 | 0.9 (–2.7 to 4.7) | 2.6 (–1.9 to 7.2) | –0.4 (–2.7 to 2.0) | –0.2 (–5.3 to 5.1) | ||
| No. of physicians per 1000 population | .20 | 95.9 | ||||
| 4.0 | –0.1 (–4.1 to 4.1) | 2.4 (–2.7 to 7.7) | –1.4 (–4.5 to 1.7) | 2.1 (–3.6 to 8.2) | ||
| 5.2 | 2.0 (–1.8 to 5.8) | 3.1 (–1.5 to 8.0) | –0.5 (–3.1 to 2.1) | –1.0 (–6.3 to 4.5) | ||
95%CI, 95% confidence interval.
Pooled estimates for the provincial characteristics were obtained via random-effects multivariate meta-analysis models relating provincial segmented regression coefficients with the values of their corresponding characteristics as a continuous individual covariate.
Pooled estimates and 95%CI values at the time of implementation of the partial ban and 1 year later vs the trend estimated during the period prior to the law (2003-2005) for the 25th and 75th percentiles of the provincial characteristics.
Pooled estimates and 95%CI values at the time of implementation of the comprehensive ban and 1 year later vs the trend estimated during the partial ban period (2006-2010) for the 25th and 75th percentiles of the provincial characteristics.
The annual numbers of deaths from AMI, IHD, and CVD in the 2003 to 2013 period, disaggregated according to whether the death occurred in the in-hospital or out-of-hospital setting, are shown in . The fraction of out-of-hospital deaths from AMI and IHD was largely constant during the entire period, whereas death from CVD showed a progressive reduction in out-of-hospital mortality that did not appear to be related to the smoking bans.
DISCUSSIONThis study failed to identify significant reductions in hospital admissions for AMI, IHD, or CVD in individuals aged ≥ 18 years after the successive introduction of the 2 smoking bans in Spain and found considerable variation in estimated rates among the included provinces.
Coronary Heart DiseaseIn Europe, excluding those performed in Spain, various studies have detected positive effects, such as in Italy,21–24 Ireland,25,26 England,27 Scotland,28 and Germany.29 The reduction in acute coronary events varies greatly: 2.4% in Scotland (AMI),27 3% to 5% in Italy (IHD),21 8.6% and 13.3% in Germany (AMI and unstable angina),29 and 17% in Scotland (IHD).28 In the Netherlands, a local study estimated a 6.8% reduction in sudden cardiac death events after the introduction of a partial ban prohibiting smoking at work.30 In contrast, no benefits were found in France31 and Denmark32 or in the region of Geneva (Switzerland).33 Discrepancies were also seen in the United States: although multiple local studies found clear benefits after the implementation of tobacco regulations, analyses of the country as a whole failed to find significant associations for either mortality or admissions for AMI.15
In Spain, 3 studies have assessed the impact of the first law (Law 28/2005). The first, performed in the city of Barcelona,13 showed a boost to the annual decrease in admissions for AMI of about 5% in men and 2% in women. A study performed in the province of Girona–Registre Gironí del Cor (REGICOR)12–found an 11% decreased risk of hospitalization for AMI. The most recent study compared the changes in admissions for AMI in the cities of Madrid and Barcelona and detected a nonsignificant increase in admissions of 6.6% in Madrid but a nonsignificant decrease of 6.3% in Barcelona.14
Cerebrovascular DiseaseThe causal association between ETS exposure and CVD is a much more recent finding34 and the evidence of the impact of smoking bans on CVD is less stronger and less consistent.26,33,35–42 In the United States, 2 studies found a fall in CVD in Texas and Arizona,36,37 as well as in Florida, but not in New York or Oregon.38,39 In Canada, the results were also conflicting, with 2 local studies finding either no effect35 or partially positive associations.42 No effects were detected in China.41 Finally, 2 studies performed in Europe (Ireland26 and Switzerland33) found no association. In contrast, in Scotland, MacKay et al.40 observed a reduction in stroke but no associations for other CVDs. In Spain, no changes were detected in the city of Madrid, whereas Barcelona showed a significant decrease of 10.2%.14
The benefits in countries that have introduced comprehensive bans appear to be higher than in those regions with partial bans.7 The present study seemed to detect a major immediate effect with the comprehensive ban, although the findings were only significant in individuals aged ≥ 65 years, with significant changes seen immediately after ban implementation.
Although the immediate associations seen in the population aged ≥ 65 years with the implementation of the comprehensive ban disappeared over time, the effect seemed to be higher than in younger people. Multiple studies have also observed protective effects in older people.12,23,27,28,43 In the REGICOR study, the association between the partial ban and AMI was only seen in individuals aged 65 to 74 years, which could be related to the higher prevalence of other risk factors in older people and due to their greater contribution to the total number of infarction events.12
The wide heterogeneity seen among the included provinces is in line with the high variability found in other studies. This study is one of the first to investigate the possible sources of the interregional variability, although the explanatory variables barely managed to reduce the heterogeneity. One possible explanation could be related to differences in ban implementation, although it was not possible to examine this hypothesis because there is no information disaggregated at the provincial level on the degree of adherence. The only significant interaction detected in the study was a stronger impact of the laws in provinces with a lower human development index. These results are in accordance with the work done by Barnett et al.43 in New Zealand and by Cesaroni et al.23 in Italy, where there was a greater tendency for a decrease in admissions for AMI43 and acute coronary heart disease23 in people living in areas with a lower socioeconomic level. Future studies should investigate other sources of variability, including the degree of implementation of cardiovascular disease prevention measures.
LimitationsVarious limitations need to be considered when interpreting the results of this study. The main limitation is due to its ecological design, which meant that causal relationships could not be established. In addition, individual information was unavailable on certain covariates that could have confounded the association. This is important because the fall in the incidence of AMI in Europe in the last 25 years probably reflects the primary and secondary prevention of this disease and its effects on various risk factors and treatments.44 This is the case with tobacco consumption, although a sensitivity analysis performed with the introduction of ecological smoking prevalence failed to alter the estimates, expected results given that in Spain, as in other countries, smoking prevalence was unaffected by the introduction of these regulations.2 However, those studies that differentiated the effects of bans on smokers and nonsmokers in terms of cardiovascular diseases found a greater effect in nonsmokers.2 These results were also recorded in the REGICOR study, carried out in Spain,12 where implementation of Law 28/2005 reduced AMI events by 18% in nonsmokers vs 9% in smokers. In agreement with these findings, it is likely that if we had been able to distinguish between the smoking and nonsmoking populations, the slight reduction seen in coronary heart disease would have been somewhat larger in the nonsmoking population. Other variables showing variations during the study period–such as use of statins, antidiabetic agents, and blood pressure-lowering medication–could not have been included in the analysis because the linear or exponential growth in these drugs destabilized variable trend parameters. Their effects were probably indirectly considered with the introduction of the trend in the time series.
Most of the studies of laws against smoking evaluated their short- or midterm impact because the effects of ETS exposure rapidly appear at low exposure levels.1 Nonetheless, the meta-analysis by Meyers et al.6 suggested that the magnitude of the association could be higher the longer the observation period after implementation of the ban. This could be because, if the protective effect of the law is gradual and sustained over time, the simple comparison of global rates before and after the law would result in greater impact estimates the longer the period analyzed after law implementation. However, this study used segmented models permitting estimation of both immediate jumps in the rates upon introduction of each law as well as gradual changes in trends (distinct slopes) in each legislation period and, consequently, these results are robust vs distinct impact types and variations in the observation period.
Despite the strong heterogeneity among provinces, we decided to calculate a pooled estimate, given that the variability was not due to the use of different information sources or analysis methods. Nonetheless, these pooled estimates should not be interpreted as the only impact in the entire country, but as the mean of the various underlying impacts in each province.
The selection of Minimum Basic Data Set codes retaining a greater relationship with chronic cardiovascular disease could have allowed an underestimation of the short-term effect. However, the results showed similar estimates when a specific acute process was analyzed, such as myocardial infarction, as when the entire group of IHDs was considered.
Finally, we cannot rule out the influence of administrative factors related to the Minimum Basic Data Set registry that may have affected admissions for these diseases. In addition, the changes in out-of-hospital mortality occurring during this period could have influenced the estimates; however, for the 3 diseases analyzed, there was a decrease in in-hospital and out-of-hospital mortality rates, without changes related to the introduction of the 2 regulations on mortality fractions.
CONCLUSIONSThe results of this study fail to show that the 2 tobacco consumption laws implemented in Spain significantly decreased hospital admissions for AMI, IHD, or CVD, with the exception of an immediate fall for these 3 diseases in the population aged ≥ 65 years, a reduction that was no longer evident 1 year later. However, our findings do not detract from the considerable contribution of these laws to public health, given that they have managed to reduce ETS exposure in all enclosed public spaces included in the legislation, as well as the benefits on the cardiovascular system due to prevention of ETS exposure.
FUNDINGGrant FIS PI11/01276 to the Instituto de Salud Carlos III from the Spanish Ministerio de Economía y Competitividad.
CONFLICTS OF INTERESTNone declared.
- –
Numerous studies evaluating the effect of smoking bans in enclosed public spaces have found benefits in terms of cardiovascular disease incidence, mortality, and admissions. However, there are discrepancies regarding the magnitude of the associations and the variability of estimates within the same country. Spain has implemented 2 public health measures concerning smoking, a partial ban (2006) and a comprehensive ban (2011), which have markedly decreased ETS exposure. However, there has been no overall evaluation of their impact on cardiovascular admissions.
- –
There were no significant reductions in admissions for AMI, IHD, and CVD in persons aged ≥ 18 years after implementation of the smoking bans. For the population aged ≥ 65 years, the comprehensive ban was associated with an immediate fall in admissions for these diseases, although the reduction was no longer evident at 1 year. There was considerable variability among the 14 included provinces that was not substantially reduced upon analysis of diverse explanatory variables.
.
The authors wish to express their thanks to Amparo Larrauri for the data provided on influenza (Spanish Sistema Centinela de Vigilancia de la Gripe).