The guidelines of the American College of Cardiology/American Heart Association and the British National Institute for Health and Clinical Excellence on the management and treatment of dyslipidemia recommend significant changes, such as the abolition of therapeutic targets and the use of new risk tables. This study aimed to evaluate the impact of the use of these new guidelines compared with the application of European guidelines.
MethodsObservational study conducted among Spanish workers. We included all workers registered with the Sociedad de Prevención de Ibermutuamur in 2011 whose cardiovascular risk could be evaluated. Cardiovascular risk was calculated for each worker using the Systematic Coronary Risk Evaluation cardiovascular risk tables for low-risk countries, as well as the tables recommended by the American and British guidelines.
ResultsA total of 258 676 workers were included (68.2% men; mean age, 39.3 years). High risk was found in 3.74% of the population according to the Systematic Coronary Risk Evaluation tables and in 6.85% and 20.83% according to the British and American tables, respectively. Treatment would be needed in 20 558 workers according to the American guidelines and in 13 222 according to the British guidelines, but in only 2612 according to the European guidelines. By following the American guidelines, the cost of statins would increase by a factor of 8.
ConclusionsThe new recommendations would result in identifying more high-risk patients and in treating a larger fraction of the population with lipid-lowering drugs than with the European recommendations, which would result in increased costs.
Keywords
The European guidelines on the management of dyslipidemia and on cardiovascular prevention published in 2011 and 2012, respectively, by a joint committee from distinct European scientific societies1,2 have been translated, debated and adapted, with broad circulation in Spain3,4. The guidelines of the ACC/AHA (American College of Cardiology/American Heart Association)5 on the management and treatment of dyslipidemias were published at the end of 2013, and immediately gave rise to intense debate, both in the United States and in the European Union and other countries. Specifically, the American guidelines, focused their recommendations on the use of statins, and defined 3 treatment levels: high-, moderate-, and low-intensity, depending on the statin and its dosage. These guidelines abandon low-density lipoprotein cholesterol (LDL-C) targets and implicitly assume that, for each treatment level, there will be a specific percentage reduction in LDL-C.
Another new, and also controversial, aspect of these guidelines is the publication of new risk tables that measure the risk of atherosclerotic cardiovascular disease (ASCVD tables) based on different American cohorts and make specific recommendations on statin therapy for primary prevention in people with cardiovascular risk ≥ 7.5%.
The British National Institute for Health and Clinical Excellence (NICE) is another internationally prestigious group that has recently published a draft document on the management of dyslipidemias, which is similar to the American guidelines in that it does not recommend therapeutic targets and also defines treatment intensity. This document recommends the use of the QRISK2 risk tables, which are derived from primary care databases in England,6 and statin therapy in primary prevention among people with cardiovascular risk ≥ 10% (≥ 20% in the previous guidelines).
If the new American guidelines in the United States, with the risk factor profile of the NHANES-III (Third National Health and Nutrition Examination Survey) 2005-2010 cohort (3773 participants) were extrapolated to the entire US population aged between 40 years and 75 years (115.4 million people), the number of individuals to be treated with statins would increase from 43.2 million (37.5%) to 56 million (48.6%), and most of this difference (10.4 million/12.8 million) would consist of individuals without cardiovascular disease.7 In the subgroup aged 60 years to 75 years (primary prevention), this fraction would increase from 30.4% to 87.4% among men and from 21.2% to 53.6% among women. Another Swiss study, in a sample of 3297 people aged 50 years to 75 years, estimated that the use of the new American tables rather than the European guidelines would double the number of persons eligible for lipid-lowering therapy, a difference that was much higher in the group aged 50 years to 60 years.8 Extrapolating these data to the Swiss population, the application of the American guidelines would increase the annual cost of cardiovascular prevention treatment by €333.7 million.
Studies have recently been published that evaluate LDL-C control in patients with a prior coronary event according to the recommendations of secondary prevention guidelines.9,10
The aim of this study was to evaluate the impact of using the American and British guidelines versus the European guidelines on the percentage of patients requiring statin therapy in a Spanish working population in primary prevention.
METHODSThe methodology of this study has been previously described as part of the ICARIA (Ibermutuamur CArdiovascular RIsk Assessment)11 study. For this particular study, we included all workers whose companies had contracted health monitoring services from the Sociedad de Prevención de Ibermutuamur, who underwent a medical review between January 4th and December 30th 2011, and who had complete information in all fields required for cardiovascular risk assessment. All autonomous regions of Spain were represented in the study sample, including Ceuta and Melilla. Incomplete cases, ie, those with unverified outliers, and previously diagnosed cases of cardiovascular disease were excluded. For each worker, the risk of cardiovascular disease was calculated using the SCORE (Systematic Coronary Risk Evaluation) tables for low-risk countries,12 and using the QRISK213 and ASCV14 tables. The risk functions were developed from the original formulas, and the workers’ cardiovascular risk was calculated using StataSE 12. To calculate risk according to the QRISK2 formula, a number of assumptions were made: by default, race was considered to be “WHITE”; UK postcode was not applicable; and the responses to questions on atrial fibrillation, rheumatoid arthritis, and history of cardiovascular disease before 60 years of age in first-degree relatives were considered negative, since this information was not recorded.
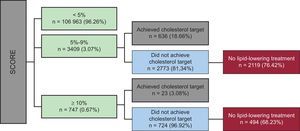
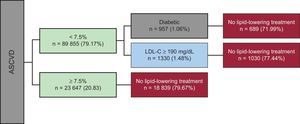
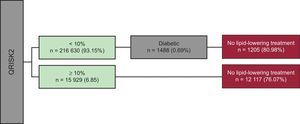
Depending on the risk estimation obtained from the various tables, we calculated the percentage of patients who achieved the therapeutic goals, and who were undergoing lipid-lowering therapy according to SCORE. Specifically, following the recommendations of the Fourth Joint Document of the European Guidelines on Cardiovascular Prevention,2 LDL-C treatment targets for patients at high or very high risk according to SCORE are as follows: for a risk of 5%-9% and ≥ 10%, an LDL-C concentration of<100mg/dL and <70mg/dL is recommended, respectively. For the QRISK2 and ASCV tables, since the NICE and ACC/AHA recommendations do not stipulate therapeutic targets for LDL-C, all patients at high risk were considered to be candidates for lipid-lowering therapy.
To estimate the additional costs associated with statin therapy in high-risk individuals according to the various tables, the following statins were considered: 40mg simvastatin, €2.17; 20mg atorvastatin, €9.21; and 10mg rosuvastatin, €25.95; all these drugs were offered in packs of 28 tablets.
All analyses were carried out using StataSE 12.
RESULTSTable 1 shows the clinical and demographic characteristics of the selected workers. A total of 258 676 workers (68.2% men; mean age, 39.3 [16-75] years) were included in the analysis. We excluded 162 workers without age data and 996 with a prior cardiovascular event.
General Characteristics of Evaluated Patients
| Men(n=176 369) | Women(n=82 307) | Total(n=258 676) | |
| Age, mean (SD) y | 39.72 (10.30) | 38.42 (9.75) | 39.31 (10.14) |
| Smoking | |||
| Nonsmoker | 82 587 (46.83) | 44 474 (54.03) | 127 061 (49.12) |
| Ex-smoker | 26 794 (15.19) | 10 281 (12.49) | 37 075 (14.33) |
| Smoker | |||
| < 10 cigarettes | 25 071 (14.22) | 15 157 (18.42) | 40 228 (15.55) |
| 11-20 cigarettes | 27 354 (15.51) | 7839 (9.52) | 35 193 (13.61) |
| > 20 cigarettes | 10 747 (6.09) | 2846 (3.46) | 13 593 (5.25) |
| Not recorded | 3816 (2.16) | 1710 (2.08) | 5526 (2.14) |
| Hypertensiona | 14 087 (7.99) | 3197 (3.88) | 17 284(6.68) |
| Hypercholesterolemiab | 14 650 (8.31) | 3903 (4.74) | 18 553 (7.17) |
| T1DM | 514 (0.29) | 144 (0.17) | 658 (0.25) |
| T2DM | 2733 (1.55) | 395 (0.48) | 3128 (1.21) |
| Systolic blood pressure (mmHg), mean (SD) | 126.55 (15.30) [175 401] | 113.81 (15.02) [81 804] | 122.50 (16.33) [257 205] |
| Diastolic blood pressure (mmHg) mean (SD) | 77.81 (10.89) [175 355] | 72.28 (10.27) [81 763] | 76.05 (11.00) [257 118] |
| Total cholesterol (mg/dL) mean (SD) | 191.02 (36.02) [175 152] | 185.74 (33.01) [81 691] | 189.34 (35.18) [256 843] |
| HDL-C (mg/dL), mean (SD) | 50.98 (12.88) [174 843] | 65.11 (15.21) [81 608] | 55.47 (15.16) [256 451] |
| LDL-C (mg/dL), mean (SD) | 118.30 (31.86) [174 469] | 105.08 (29.45) [81 342] | 114.10 (31.72) [255 811] |
| BMI, mean (SD) | 26.91 (4.06) [174 659] | 24.24 (4.40) [81 363] | 26.06 (4.36) [256 022] |
HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus; BMI, body mass index.
Values are expressed as No. (%) or mean (standard deviation) [n].
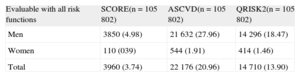
Cardiovascular risk according to the SCORE, ASCVD, and QRISK2 tables could be evaluated in 42.96%, 43.88% and 89.9% of participants, respectively, with a mean age of 48.46 years, 48.47 years and 40.24 years. Table 2 shows risk classification according to the different tables, and highlights the marked differences between the methods used, with the number of high-risk patients varying from 20.83% according to the ASCVD tables to 3.74% according to the SCORE tables for low-risk countries. When we evaluated cardiovascular risk among individuals whose risk could be calculated according to all 3 tables, the percentage of patients at high risk in the SCORE and ASCVD tables remained stable, whereas that in the QRISK2 tables increased to 13.9% from the 6.85% observed for all individuals (Table 3).
Comparison of the 3 Risk Tables
| Patients with high risk | SCORE (n=111 119) | ASCVD (n=113 502) | QRISK2 (n=232 559) |
| ≥ 5% | ≥ 7.5% | ≥ 10% | |
| Men | 4036 (5.03) | 22 991 (28.46) | 15 423 (9.50) |
| Women | 120 (0.39) | 656 (2.00) | 506 (0.72) |
| Total | 4156 (3.74) | 23 647 (20.83) | 15 929 (6.85) |
ASCVD, atherosclerotic cardiovascular disease; SCORE, Systematic Coronary Risk Evaluation.
Values are expressed as No. (%).
Comparison of the 3 Risk Tables in Patients Suitable for Application of the 3 Guidelines
| Evaluable with all risk functions | SCORE(n=105802) | ASCVD(n=105802) | QRISK2(n=105802) |
| Men | 3850 (4.98) | 21632 (27.96) | 14296 (18.47) |
| Women | 110 (039) | 544 (1.91) | 414 (1.46) |
| Total | 3960 (3.74) | 22176 (20.96) | 14710 (13.90) |
ASCVD, atherosclerotic cardiovascular disease; SCORE, Systematic Coronary Risk Evaluation.
Values are expressed as No. (%).
Figures 1-3 show the percentage of patients with high or very high risk according to the 3 different scales, who should be treated with statins according to the recommendations that accompany the 3 risk tables. Marked differences were observed, in that it would be necessary to treat 20 558 workers (18.11% of the total population whose risk could be calculated) according to the ACC/AHA guidelines, 13 322 (5.73%) according to the NICE guidelines, and 2613 (2.35%) according to the current recommendations of the European societies. In terms of costs, the daily cost of 40mg simvastatin would be €1593 according to the ACC/AHA guidelines, €1032 according to the NICE guidelines, and €202 according to the European guidelines. Similarly, the daily cost of 20mg atorvastatin would be €6762, €4382 and €859, respectively, and that of 10mg rosuvastatin would be €19053, €12347, and €2422, respectively.
The publication of the American guidelines on the management of dyslipidemia has provoked significant international scientific debate as a result of the substantial changes introduced with respect to the previous American and European guidelines. These new American guidelines propose a paradigm shift regarding the usefulness of statins, and recommend treating cardiovascular disease itself, rather than treating the cause of cardiovascular disease (reducing LDL-C to a target level, as recommended by the European guidelines).
One of the most controversial issues is the elimination of therapeutic targets for both primary and secondary prevention, and the use of the risk profile alone to indicate high-, moderate- or low-intensity statin therapy. In this regard, the NICE guidelines are in line with the American guidelines. We observed marked differences between the numbers of individuals to whom the tables can be applied, from 232 559 with QRISK2 to 111 119 with SCORE, mainly due to differences in the age ranges to which the tables can be applied: QRISK2, 25 years to 84 years, ASCVD, 40 years to 79 years, and SCORE 40 years to 65 years.
It is also important to note that the different risk scores estimate the incidence of distinct cardiovascular complications (SCORE measures risk of cardiovascular death, QRISK2 measures risk of cardiovascular morbidity and mortality due to coronary heart disease and stroke, and ASCVD measures risk of cardiovascular morbidity and mortality due to arteriosclerotic disease).
In addition to the differences among populations to which each of the tables can be applied, it is clear that the new American tables identify many more patients at high risk and, therefore, many more patients need to be treated with lipid-lowering drugs, particularly statins. The use of the new American tables in this Spanish working population, compared with the European tables, multiplies the percentage of participants with an indication for statin therapy by 3, ie, 1.5 times the absolute number of individuals to be treated. The results of our study corroborate those of Pencina et al7 in the United States and Vaucher et al8 in Switzerland, who concluded that the use of the new American guidelines would substantially increase the population to be treated with statins. Furthermore, application of the American guidelines to the working population in this study multiplied medical spending on statins by a factor of 6. No information is available on the implications of using the new NICE guidelines, but it seems quite likely that the high-risk population and the potential number of patients to be treated would increase, since patients with ≥ 10% risk are considered as high-risk (this figure was ≥ 20% in previous guidelines). However, to truly determine medium to long-term economic consequences, a detailed cost-opportunity and cost-effectiveness analysis is required, taking into account the number and cost of events avoided.
Recently, an expert group has reviewed and compared the American and European guidelines,15 and concluded that the European guidelines use a broader and more pragmatic approach and are more suitable for use in European countries.
The sample used in this study is clearly a selected population (Spanish working population). Thus, the results cannot be extrapolated to the general population, although they provide an accurate view of the impact of these new guidelines on the management and treatment of a common problem, dyslipidemia, in a very large group of mostly young people, in which there is significant opportunity for intervention.
Strengths and LimitationsIt should be noted that the cholesterol target was met by only 16% of workers classified as having high or very high cardiovascular risk by the most conservative of the approaches we have compared (SCORE). This finding highlights the importance of these preventive medical examinations for stratifying cardiovascular risk and controlling modifiable cardiovascular risk factors, even though a larger number of workers may be included depending on the method used, and the additional treatment costs that this would imply.
However, only workers who were not on leave (active workers) attended these medical examinations, and therefore we cannot rule out a selection bias known as the healthy worker effect.16 If this selection bias occurred, we would expect to underestimate the percentage of workers with high cardiovascular risk. However, this study has allowed us to improve our understanding of the largest group of workers (those without disease and who do not require sick leave), in which there is the greatest potential for prevention. In contrast, the effects of healthy worker bias on the differences between the different risk assessment methods are less clear, since it is assumed that selection bias will affect the groups to the same extent. Another possible limitation of the study is that in patients at high or very high risk, we only considered those who were treated with statins, but we do not know if this treatment involved high-intensity statins (20mg/day rosuvastatin, or 40-80mg/day atorvastatin), as recommended by the American guidelines.
In addition to these potential limitations, it is also important to note some of the strengths of our study. The most important feature of this study is that, for the first time, the impact of these new guidelines on the management and treatment of dyslipidemia has been compared in a large sample of the Spanish working population, and our results could assist health professionals to better understand the possible consequences of using one set of guidelines or another. The sample size of the study is much larger than that used in similar studies and the available data are of high quality, given the high level of completeness and comprehensiveness in recording the data from the medical examinations.
CONCLUSIONSThe application of new American and British recommendations to the Spanish working population would identify more high-risk patients and would indicate lipid-lowering therapy in a larger population than the European guidelines, which would increase the daily cost of statins by a factor of almost 8.
CONFLICTS OF INTERESTNone declared.