Equal opportunities to access technical advances with recognized clinical value should be a priority of the publicly-funded health system. We analyzed variability among all the Spanish autonomous communities in the use of cardiovascular techniques with an established indication and its relationship with economic indicators, burden of disease, and hospital mortality.
MethodsThe activity registries of various Associations of the Spanish Society of Cardiology from 2011 to 2019 were analyzed for coronary angiography, overall percutaneous coronary intervention (PCI), primary PCI, implantable cardioverter-defibrillators (ICD), cardiac resynchronization therapy, and transcatheter aortic valve replacement (TAVR). Economic indices (gross domestic product and per capita health care expenditure) were obtained from public sources and data on attendance rates and mortality from the Resources and Quality in Cardiology (RECALCAR) reports of the Spanish Society of Cardiology. We analyzed the coefficient of variation for activity and the correlation of activity with regional economic indices, attendance rates, and risk-adjusted rates of in-hospital mortality.
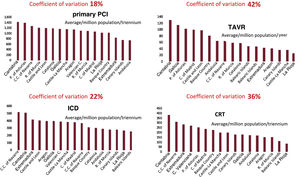
ResultsWe identified wide variability in the use of technologies, especially for primary PCI (18%), ICD (22%), cardiac resynchronization therapy (36%), and TAVR (42%). A certain correlation with attendance rates was seen only for overall PCI and ICD. In general, no significant correlation was found between the use of the techniques and the economic indices of wealth and expenditure. The correlation with in-hospital mortality showed no significant results, although this was the analysis with the greatest limitations because the impact of these techniques on survival is exerted more in the mid- and long-term.
ConclusionsThe results of this study, despite its inherent limitations, show marked variability between autonomous communities in the use of cardiovascular technologies, which is not explained by economic differences or by hospital attendance rates due to the corresponding diseases.
Keywords
Scientific and technical progress has led to considerable advances in cardiology and a notable reduction in cardiovascular mortality.1 In a publically-funded health care setting such as that of Spain, equal opportunities to access these advances should be a priority. However, a study published in 2006 with data from 2003 reported substantial differences between the Spanish autonomous communities (ACs) in the use of certain cardiovascular techniques. These differences were related in part to regional wealth, but not to the burden of disease.2,3 More than 15 years after publication of those results, the present study aimed to analyze use of the most important cardiology procedures in each AC over the last decade, when their indications are better established and the disparity in structural resources between territories is less marked. The study examines the extent to which inequalities between ACs are related to economic indicators of wealth and expenditure, the burden of disease, and in-hospital mortality.
METHODSYearly data on the use of cardiovascular techniques in the autonomous communitiesEach year, the Spanish Registry of Cardiac Catheterization and Interventional Cardiology, the Spanish Registry of Implantable Cardioverter-Defibrillators, and the Spanish Registry of Pacemakers, maintained by various associations within the Spanish Society of Cardiology (SEC),4–6 are published in the Revista Española de Cardiología.
The yearly activity related to the following techniques was analyzed for the 2011 to 2019 period: coronary angiography (CA), percutaneous coronary intervention (PCI), primary PCI (pPCI), implantable cardioverter-defibrillator (ICD), cardiac resynchronization therapy (CRT), and transcatheter aortic valve replacement (TAVR). The list of the annual registries reviewed is included in .
For TAVR, only the 2017, 2018, and 2019 registries were reviewed, as data from the previous years had not been broken down by AC. For the purposes of data analysis and presentation, all techniques except TAVR have been grouped into 3-year subperiods (2011-2013, 2014-2016, and 2017-2019).
Data from 2020, the year of the COVID-19 pandemic, were excluded from the analysis because of the huge change occurring in the activity related to these techniques, which was uneven between the ACs.
Clinical evidence for the techniques analyzedTo estimate the strength of the clinical evidence supporting indications for the techniques included, we consulted the European Society of Cardiology clinical practice guidelines, reviewing the classes of recommendation and levels of evidence in force at the study start and the modifications occurring over the study period for each technique.7–14
Economic and demographic dataThe population size, per capita gross domestic product (GDP), and per capita health expenditure (HE) values for each AC and each year were obtained from official sources.15,16
Data on the cardiovascular disease burden and mortalitySerial incidence data for the various cardiovascular diseases in each community are lacking. Hence, we used a source that can provide an estimated incidence of infarction and heart failure based on hospital admissions: the Resources and Quality in Cardiology (RECALCAR) reports of the SEC.17 The hospital admission rate (HAR) refers to the number of admissions per 100,000 population per year for cardiology in general and specifically, for infarction and heart failure. Through this variable, the activity of each AC for each technique can be contextualized by adjusting values by admissions, which would account for the disease incidence and effects of population mobility.
Data from the RECALCAR reports were used to relate (although in a relative manner) the use of the techniques studied to cardiovascular mortality. These reports describe the risk-standardized mortality ratio (RSMR), with multilevel adjustment for overall cardiovascular disease, myocardial infarction, and heart failure. The RSMR is the ratio of the predicted mortality (which considers the operation of each hospital attending a patient individually) to the expected mortality (which considers the standard operation according to the mean of all hospitals), multiplied by the crude mortality rate.
With regard to aortic stenosis, there is no available information on incidence by year and AC. Therefore, we used the national Registry of Interventions of the Spanish Society of Cardiovascular and Endovascular Surgery, which has provided the number of surgical aortic valve replacements (SAVR) by AC in some of its recent yearly editions. This information is available for 2017 and 2018,18,19 but not for 2019.
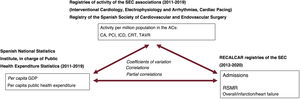
The information sources, variables analyzed, and types of analyses carried out are summarized in figure 1.
Study design, and information sources and analysis. ACs, autonomous communities; CA, coronary angiography; CRT, cardiac resynchronization therapy; GDP, gross domestic product; ICD, implantable cardioverter-defibrillator; PCI, percutaneous coronary intervention; pPCI, primary PCI; RECALCAR: Resources and Quality in Cardiology reports; RSMR, risk-standardized mortality rate; SEC, Spanish Society of Cardiology; TAVR, transcatheter aortic valve replacement.
Data set distribution was analyzed with the Shapiro-Wilk test. The coefficient of variation, determined as an indicator of variability between the ACs in technique use, is presented as the ratio of the standard deviation to the mean, multiplied by 100. Coefficients of variation were compared using the Forkman test. Associations between the volume of activity of ACs for each technique and the HAR, GDP, HE, and RSMR were assessed using the correlation coefficient and the partial correlation (adjusted by variables with a potential impact). Correlations between technique use and economic variables were adjusted taking into account hospital admissions related to each technique analyzed. A similar partial correlation was made by determining the correlation between technique use and RSMR rates. For TAVR analysis, correlations between the activity and economic variables were adjusted by the total number of aortic valve procedures and the number of surgical procedures alone. A P value of <.05 was considered statistically significant. All statistical analyses were carried out using the MEDCALC V19 and SPSS V25 software packages.
RESULTSActivity rates for the techniques analyzed by AC and period are shown in . GDP values and per capita HE are described in HAR-overall, HAR-infarction and HAR-heart failure in figure 8, and RSMR-overall, RSMR-infarction, and RSMR-heart failure in . Of note, data sets followed a normal distribution for the purpose of analysis. The classes of recommendations in the clinical practice guidelines over the study period are shown in .
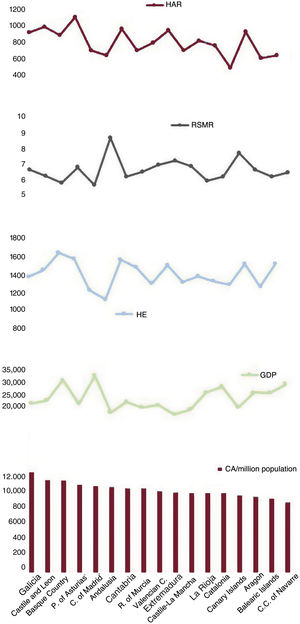
The mean number of CA procedures performed per million inhabitants/triennium in each AC during the 2011 to 2019 period, per capita GDP, per capita HE, and the overall cardiology HAR and RSMR are shown in figure 2.
Mean CA values per million population/triennium by autonomous community (2011-2019), per capita GDP, per capita HE, and overall cardiology HAR and RSMR. CA, coronary angiography; HAR, hospital admission rate; HE, health expenditure; GDP, gross domestic product; RSMR, risk-standardized mortality rate.
The coefficients of variation and partial correlations obtained for the total study period and each triennium are shown in table 1. There were no changes in coefficients of variation, and the overall value was 9%. Correlations with the HAR were significant in the total period and in the last triennium. HAR-adjusted partial correlations of activity with economic indices and RSMR were nonsignificant.
Analysis of variation and correlation results for activity between the autonomous communities
| Periods | Total | |||
|---|---|---|---|---|
| 2011-13 | 2014-16 | 2017-19 | 2011-2019 | |
| Coronary angiography | ||||
| Coefficient of variation | 13% | 11% | 12%* | 9% |
| Correlation with HAR-overall | 0.03 (P=.9) | 0.4 (P=.08) | 0.6 (P=.004) | 0.5 (P=.03) |
| Correlation with GDP (HAR-overall) | 0.09 (P=.7) | 0.01 (P=.9) | −0.3 (P=.2) | −0.08(P=.7) |
| Correlation with HE (HAR-overall) | –0.08 (P=.7) | −0.18 (P=.5) | –0.2 (P=.4) | –0.3 (P=.2) |
| Correlation with RSMR-overall (HAR-overall) | –0.2 (P=.4) | –0.2 (P=.5) | 0.3 (P=.2) | 0.06 (P=.8) |
| overall PCI | ||||
| Coefficient of variation | 14% | 12% | 11%* | 11% |
| Correlation with HAR-overall | 0.6 (P=.01) | 0.7 (P=.002) | 0.7 (P=.001) | 0.7 (P=.001) |
| Correlation with CA | 0. 4 (P=.08) | 0. 7 (P=.003) | 0. 8 (P=.0007) | 0.7 (P=.002) |
| Correlation with GDP (HAR-overall) | 0.2 (P=.5) | 0.3 (P=.3) | –0.17 (P=.5) | 0.14 (P=.6) |
| Correlation with HE (HAR-overall) | 0.3 (P=.3) | 0.2 (P=.4) | 0.28 (P=.3) | 0.36 (P=.2) |
| Correlation with RSMR-overall (HAR-overall) | –0.25 (P=.3) | –0.4 (P=.1) | 0.21 (P=.4) | –0.19 (P=.5) |
| primary PCI | ||||
| Coefficient of variation | 36% | 22% | 17%* | 18% |
| Correlation with HAR inf. | –0.1 (P=.6) | 0.26 (P=.3) | 0.3 (P=.2) | 0.17 (P=.5) |
| Correlation with GDP (HAR inf.) | 0.15 (P=.6) | 0.5 (P=.04) | 0.05 (P=.8) | 0.37 (P=.1) |
| Correlation with HE (HAR inf.) | 0.4 (P=.1) | 0.2 (P=.3) | 0.4 (P=.08) | 0.5 (P=.04) |
| Correlation with RSMR inf. (HAR inf.) | –0.5 (P=.04) | –0.05 (P=.8) | 0.16 (P=.5) | –0.05 (P=.8) |
| ICD | ||||
| Coefficient of variation | 26% | 22% | 23%* | 22% |
| Correlation with HAR inf. | 0.5 (P=.05) | 0.3 (P=.2) | –0.1 (P=.7) | 0.3 (P=.2) |
| Correlation with GDP (HAR inf.) | 0.2 (P=.4) | –0.28 (P=.3) | –0.06 (P=.8) | –0.02 (P=.9) |
| Correlation with HE (HAR inf.) | 0.4 (P=.07) | 0.14 (P=.6) | 0.47 (P=.06) | 0.44 (P=.08) |
| Correlation with HAR HF | 0.4 (P=.06) | 0.6 (P=.02) | 0.5 (P=.03) | 0.6 (P=.01) |
| Correlation with GDP (HAR HF) | –0.2 (P=.4) | –0.4 (P=.06) | –0.05 (P=.8) | –0.27 (P=.3) |
| Correlation with HE (HAR HF) | 0.37 (P=.1) | –0.2 (P=.5) | 0.3 (P=.3) | 0.26 (P=.3) |
| [0,1-5]CRT | ||||
| Coefficient of variation | 43% | 36% | 37%* | 36% |
| Correlation with HAR HF | –0.18 (P=.5) | 0.1 (P=.7) | 0.3 (P=.2) | 0.09 (P=.7) |
| Correlation with GDP (HAR HF) | 0.1 (P=.7) | –0.08 (P=.7) | –0.07 (P=.8) | –0.04 (P=.8) |
| Correlation with HE (HAR HF) | 0.38 (P=.1) | 0.28 (P=.3) | 0.15 (P=.5) | 0.42 (P=.09) |
| Correlation with RSMR (HAR HF) | 0.27 (P=.3) | 0.32 (P=.2) | 0.13 (P=.6) | 0.32 (P=.2) |
| TAVR | ||||
| Coefficient of variation | 42% | |||
| Correlation with SAVR | 0.5 (P=.04) | |||
| Correlation with GDP | 0.2 (P=.5) | |||
| Correlation with HE | 0.15 (P=.6) | |||
| Correlation with GDP (SAVR) | 0.14 (P=.6) | |||
| Correlation with HE (SAVR) | 0.09 (P=.7) | |||
| Correlation with GDP (TAVR+SAVR) | 0.05 (P=.8) | |||
| Correlation with HE (TAVR+SAVR) | 0.,01 (P=.9) | |||
CA, coronary angiography CRT, cardiac resynchronization therapy; GDP, per capita gross domestic product; HAR-overall: hospital admittance rate for overall conditions; HAR HF, hospital admittance rate for heart failure; HAR inf., hospital admittance rate for infarction; HE, per capita health expenditure; ICD, implantable cardioverter-defibrillator; PCI, percutaneous coronary intervention; RSMR-overall, risk-standardized mortality ratio for overall conditions; RSMR inf., risk-standardized mortality ratio for infarction; SAVR, surgical aortic valve replacement; TAVR, transcatheter aortic valve replacement.
Correlation values are expressed as the r (p). Partial correlations were adjusted by the variable in parentheses. The coefficient of variation for the overall study period was calculated using the mean activity rate for each autonomic community over the total period.
The mean number of PCIs performed per million inhabitants/triennium in each AC during the 2011 to 2019 period, per capita GDP, per capita HE, and the overall cardiology HAR and RSMR are shown in figure 3.
Mean PCI values per million population/triennium by autonomous community (2011-2019), per capita GDP, per capita HE, and overall cardiology HAR and RSMR.
HAR, hospital admission rate; HE, health expenditure; GDP, gross domestic product; PCI, percutaneous coronary intervention; RSMR, risk-standardized mortality rate.
The coefficients of variation obtained were all comparable, and that of the total period was 11%. Correlations with the HAR were significant in all periods, as were correlations with the CA results. Partial correlations of activity with the economic indices and RSMR were nonsignificant (table 1).
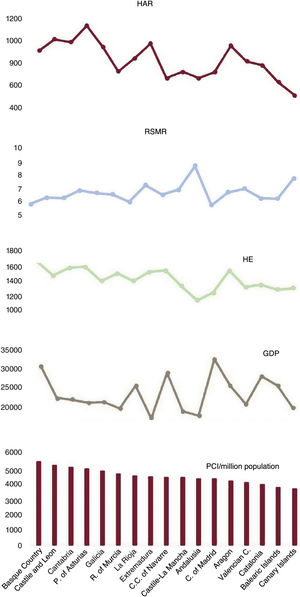
Primary percutaneous coronary interventionsThe mean number of pPCIs performed per million inhabitants/triennium in each AC during the 2011-2019 period, per capita GDP, per capita HE, and the HAR and RSMR, both for infarction, are depicted in figure 4.
Mean pPCI values per million population/triennium by autonomous community (2011-2019), per capita GDP, per capita HE, and HAR and RSMR, both for infarction.
GDP, gross domestic product; HAR, hospital admission rate; HE, health expenditure; pPCI: primary percutaneous coronary intervention; RSMR, risk-standardized mortality rate.
The coefficients of variation showed a significant decrease from 36% to 17% (P=.007). Correlations with the HAR for infarction were nonsignificant. Partial correlations between volume of activity and economic indicators were moderate and individually significant in 1 triennium for the GDP and in the total period for the HE. The partial correlation with the RSMR for infarction was significant and negative only in the first triennium (table 1).
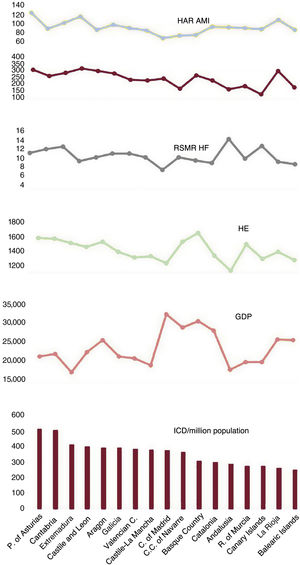
Implantable cardioverter-defibrillatorThe mean number of ICD procedures performed per million population/triennium in each AC during the 2011 to 2019 period, per capita GDP, per capita HE, HAR for infarction and heart failure, and RSMR for heart failure are depicted in figure 5.
Mean ICD values per million population/triennium by autonomous community (2011-2019), per capita GDP, per capita HE, HAR for infarction and heart failure, and RSMR for heart failure. AMI, acute myocardial infarction; GDP, gross domestic product; HAR, hospital admission rate; HE, health expenditure; HF, heart failure; ICD, implantable cardioverter-defibrillator; RSMR, risk-standardized mortality rate.
The coefficients of variation showed no significant changes, and yielded a value of 22% for the total study period. Correlations were nonsignificant with the HAR for infarction, but were significant with the HAR for heart failure. Partial correlations between volume of activity and economic indicators were nonsignificant (table 1). A correlation analysis between RSMR values for infarction and acute in-hospital mortality was considered inappropriate for ICD procedures.
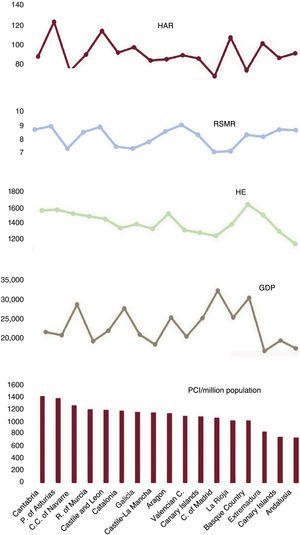
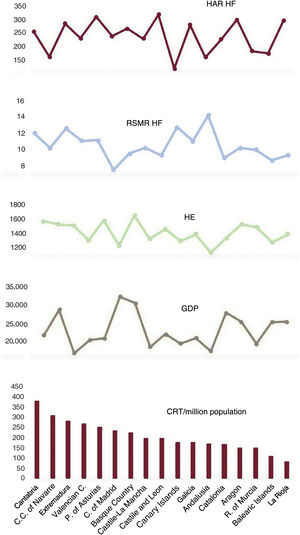
Cardiac resynchronization therapyThe mean number of CRT procedures performed per million population/triennium in each AC during the 2011 to 2019 period, per capita GDP, per capita HE, and the HAR and RSMR, both for heart failure, are shown in figure 6.
Mean CRT values per million population/triennium by autonomous community (2011-2019), per capita GDP, per capita HE, and HAR and RSMR, both for heart failure. AC, autonomous community; HAR, hospital admission rate; HE, health expenditure; HF, heart failure; GDP, gross domestic product; RSMR, risk-standardized mortality rate; CRT, cardiac resynchronization therapy.
Changes in the coefficients of variation were nonsignificant, with a decrease from 43% to 37%. Correlations with the HAR for heart failure were nonsignificant. All partial correlations between volume of activity and economic indicators, as well as the partial correlation with the RSMR for heart failure, were nonsignificant (table 1).
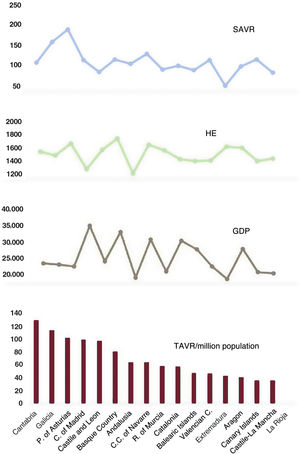
Transcatheter aortic valve replacementThe mean number of TAVRs performed per million population/y in each AC during the 2017 to 2018 period, SAVRs per million population/y, per capita GDP, and per capita HE are shown in figure 7.
Mean TAVR values per million population/y by autonomous community (2017-2018), SAVR per million inhabitants/y, per capita GDP, and per capita HE. GDP, gross domestic product; HE, health expenditure; SAVR, surgical aortic valve replacement; TAVR, transcatheter aortic valve replacement.
The coefficient of variation for TAVR activity was 42%. TAVR showed a modest correlation with SAVR activity, which was surprisingly positive, as it was expected to be negative. Correlations between TAVR activity and economic variables, presented as crude values and following adjustment for the total number of aortic valve procedures or surgical procedures alone, were nonsignificant (table 1).
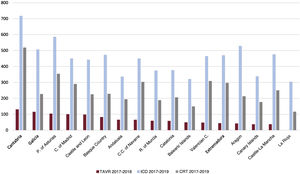
Relationship between transcatheter aortic valve replacement and implantable cardioverter-defibrillator or cardiac resynchronization therapyAn analysis was performed to examine possible relationships between TAVR activity and ICD/CRT activity in the various ACs during the most recent period (figure 8). A coefficient of 0.57 (P=.02) was obtained for the TAVR/CRT correlation, and 0.61 (P=.01) for the TAVR/ICD correlation. However, after adjusting for the overall HAR of the period, these correlations lost significance: 0.36 (P=.2) and 0.28 (P=.3), respectively.
Relationships between the health care activity studied and total populations of the autonomous communitiesA correlation analysis was performed between the practice of each technique in the total study period and the total population of each autonomous community, which yielded nonsignificant results in all cases: CA, r=0.18, P=.4; overall PCI, r=−0.27, P=.28; pPCI, r=−0.35, P=.2; ICD, r=−0.2, P=.3; CRT, r=−0.1, P=.7; and TAVR, r=−0.04, P=.8.
DISCUSSIONThe main findings of this study can be summarized as follows: a) although the cardiology techniques analyzed are well consolidated, there was considerable variation in their use between ACs, and this was very evident in pPCI, ICD, CRT, and TAVR procedures; b) correlations between the volume of activity and disease burden were only observed for ICD and overall PCI procedures; c) analysis of the economic indicators detected a modest correlation only with pPCI practice; d) in all cases, correlations with in-hospital mortality were nonsignificant, although this analysis has limitations, as the impact of these techniques on survival occurs mainly at mid- and long-term, and e) heterogeneity was observed in the technologies used in each AC.
Among all the techniques studied, variation in use was lowest for CA procedures. This finding supports the notion that the incidence of coronary disease does not differ greatly between ACs, and it contrasts with the marked variation in the use of other techniques, which are more costly and require greater resources.
Activity in the ACs related to techniques showing the highest degree of variation is shown in figure 9.
Central figure. Activity in the autonomous communities related to the techniques with highest degree of variation. CRT, cardiac resynchronization therapy; ICD, implantable cardioverter-defibrillator; PCI, percutaneous coronary intervention; TAVR, transcatheter aortic valve replacement.
Certain cardiovascular procedures in the available therapeutic arsenal stand out because of their significant impact on the patients’ prognosis. PCI (particularly, pPCI in infarction), ICD procedures, and CRT have had indications based on solid clinical evidence for the last 10 to 15 years or more.7–14 TAVR has been implemented more recently, but was quite established in the 2017 to 2019 period analyzed, after favorable results in comparative trials with surgery had been obtained in inoperable patients at high or moderate surgical risk.13
Acceptance of innovations in medical technology should be guided by scientific evidence and cost-benefit economic analyses. Their incorporation into clinical practice should follow a similar rhythm in all parts of a national health system, especially when recommendations for their use are evidence-based and endorsed by international scientific societies. Hence, major variations in technique use between regions after adjusting for the burden of disease can only be understood if there are sizable differences in health care spending due to diverse economic and political reasons.
The study analysis revealed a broad gradient of wealth between ACs that, fortunately, did not lead to wide diversity in health spending. In general, the variations in technology use did not correlate with economic indices, even after adjusting for the burden of disease.
Therefore, the variation would depend on other factors, such as the demands cardiology services make on health administrators, and the sensitivity that each executive and hospital management department shows in response to those demands. These factors operated asymmetrically in the various techniques in each community. In this sense, the distribution of health expenditure would be an important element, with each AC setting its strategic priorities.
It is likely that there would be variation between the provinces and hospitals within each AC, as some techniques would be performed only in referral centers. Centralizing activity in referral hospitals within a regional system can optimize resources and promote better results. However, this would not apply to the variability between ACs, as there is no transferal between communities for the techniques described, except in certain very exceptional cases already indicated for a technique.
Within the existing variation, it is difficult to determine the optimal point of use; that is, the activity yielding the best results in terms of effectiveness and efficiency. This aspect is beyond the scope of the present study. Nonetheless, we believe that optimal use has occurred to a greater degree on the side of higher activity rates, as the clinical guideline recommendations in force during the study period indicate, and above all, the figures showing mean activity rates clearly lower that those reported in western European countries during the same period.20,21
The absence of correlations with mortality should not serve to trivialize the variation observed, as this was the least robust analysis performed. The RSMR only refers to in-hospital mortality and not that occurring at follow-up, when the techniques analyzed have a greater impact. The correlations with hospital mortality should be taken with caution. In addition, even assuming that some techniques did not affect mortality, they could have a positive effect on other factors, such as symptoms, readmissions, pharmacological expenditure, or social impact, which we were unable to analyze, but should be considered.
The above-mentioned study evaluating variation in PCI, ICD, and CRT use was based on data recorded in registries from 2003.2 The significant variation found was explained only to some extent (20%-40%) by differences in economic indices, and there was no impact of the disease burden. The analysis was limited to activity in a single year at a time when the techniques were not as strongly consolidated or supported by clinical evidence as they are now, and there were still marked differences in structural resources between the ACs. These factors may explain the dissimilar results compared with those of our study.
More recently, a report on ischemic coronary disease hospitalizations and procedures covering the 2003 to 2015 period was created within the Atlas of Variations in Medical Practice in Spain.22 The study described variations in several quality and use indicators, with an analysis of mortality and catheterization, overall PCI, coronary surgery, and pacemaker procedures. The present study covers a more recent period, includes a larger number of techniques, and adjusts for the HAR and regional economic indices. Therefore, our aim has been to determine whether variation exists, but also to find its explanation.
The main limitation of this study is related to the accuracy of the data. The data sources, which are registries of activity and quality, contain information provided by the centers, but are not patient databases. These are only available for hospitals, not for entire autonomic regions. Furthermore, they may not include all the techniques of interest and, in any case, are created using heterogeneous systems.
Many voices in Spain have advocated for the creation of country-wide registries documenting procedures and practice with patient data, similar to the SWEDEHEART model in Sweden,23 but this would be an enormously complex undertaking in light of the sociopolitical conditions in Spain. Nonetheless, it could be a valuable source of insight and control that might ultimately improve health outcomes.
This study has found country-wide deficiencies in equitable access to cardiovascular interventions of proven clinical effectiveness. It should be a priority for the national health system and regional health services to undertake actions to correct these shortcomings to the greatest possible extent.3
LimitationsThe activity and quality registries used as information sources for the study are based on data provided by the hospitals. Data collection was retrospective, through a standardized form. Submission was voluntary and was not audited; hence, quality assurance was dependent on the reliability of the professionals providing data. It would have been optimal to have strict monitoring and auditing, but in reality, these controls are applied very little. All these registries record volume of activity, not patient information; hence, it was not possible to adjust for age and sex or other variables.
The techniques analyzed were available in all Spanish ACs during the study period, with a few exceptions. These infrequent cases were attributed to the population of the region accepting the transfer. In addition, because of vacation travelling and stays in temporary residences, some patients underwent interventions in ACs other than their own (particularly pPCI, which is not an elective procedure). Although this implies smaller volume with respect to the total activity, application of the HAR enabled a more realistic adjustment regarding use of the various techniques.
The burden of disease could not be precisely estimated, as incidence and prevalence data on cardiovascular diseases by AC and specific periods are not available. The closest approximation is the HAR data provided in the RECALCAR reports, which are quite reliable. Irrespective of this consideration, the Spanish population is not as diverse epidemiologically as larger countries having a highly mixed ethnic composition and greater economic inequalities between regions. In the ICD analysis, the adjustment used only the HAR for infarction and heart failure. Obviously, a percentage of patients with an ICD indication other than these conditions would be left out, but the proportion would be small and comparable between ACs. The analysis of aortic stenosis, in which estimation of disease burden included the SAVR plus TAVR, has a relative value. It would depend on the percentage of patients with treated severe aortic stenosis, and the surgery data also included cases of aortic regurgitation. Nonetheless, considerable disparity between ACs in these variables would not be expected.
The correlation analysis with mortality is the least robust of those studied, as the RSMR refers only to in-hospital mortality, not that occurring at follow-up, which is when the techniques analyzed have the greatest impact. Hence, the correlations with in-hospital mortality should be viewed with caution. Even assuming that mortality was not affected by some techniques, there could be other potentially positive effects on symptoms, rehospitalizations, medication expenditure, and social impact, which we were unable to analyze, but should be taken into consideration.
CONCLUSIONSThis study, which covers the period of 2011 to 2019, showed considerable variation between ACs in use of the cardiology techniques analyzed that was not explained by economic differences or by hospital admission rates due to the corresponding diseases. There was no significant correlation with in-hospital mortality, although this was the most questionable analysis because the impact of these techniques on survival is greatest at mid- and long-term. These results must be viewed with caution due to the limitations affecting the study. It should be a priority of the health system to reduce the variation observed to guarantee equitable access to these techniques.
FUNDINGThis study received no funding.
AUTHORS’ CONTRIBUTIONSConception, general design, and writing of the manuscript: J.M. de la Torre Hernández. Contributions to the study design and data collection: D. Cantarero Prieto, B. Cid, S. Ojeda, P. Jiménez Quevedo, A. Serrador, B. García del Blanco, J.F. Díaz, R. Moreno, I. Cruz, A. Pérez de Prado, I. Fernández Lozano and Ó. Cano Pérez. Data analysis: J.M. de la Torre Hernández, M. Lozano González, T. García Camarero, D. Serrano Lozano and D. Cantarero Prieto. Critical review of the manuscript: J.M. de la Torre Hernández, D. Cantarero Prieto, B. Cid, S. Ojeda, P. Jiménez Quevedo, A. Serrador, B. García del Blanco, J.F. Díaz, R. Moreno, I. Cruz, A. Pérez de Prado, I. Fernández Lozano and O. Cano Pérez. Final approval of the manuscript: J.M. de la Torre Hernández, D. Cantarero Prieto, B. Cid, S. Ojeda, P. Jiménez Quevedo, A. Serrador, B. García del Blanco, J.F. Díaz, R. Moreno, I. Cruz, A. Pérez de Prado, I. Fernández Lozano, Ó. Cano Pérez, M. Lozano González, T. García Camarero and D. Serrano Lozano.
CONFLICTS DE INTERESTNo conflicts of interest to declare.
- –
In a setting such as Spain, where publically-funded health care predominates, equal opportunities to access technical advances with recognized clinical value should be a health system priority. However, in a study of health care data from 2003, considerable differences, partially related to regional wealth but not to the burden of disease, were detected between CAs in the use of some cardiovascular technologies.
- –
In this study, which covers the period from 2011 to 2019, substantial variation was seen between ACs in the use of common cardiology techniques with recognized clinical value that was not explained by economic differences or hospital admission rates. We are thus faced with significant country-wide deficiencies in equitable access to cardiovascular interventions of proven clinical effectiveness. It should be a priority of the public health system and all regional health departments to undertake actions to correct these shortcomings to the greatest extent possible, including reinforcement of the current Healthcare Cohesion Funds.
We thank all the professionals involved in creating the health care activity registries analyzed in the present study.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2022.02.016