“See, what's ruling all our lives See, who's pulling the strings […]”
Be Quick or Be Dead. Iron Maiden, 1992
Unstable atherosclerotic plaque was found to be the most important pathophysiologic substrate of acute coronary syndromes more than 3 decades ago,1 and since then, attempts have been made to find the best way to lower the risk of acute coronary occlusion and myocardial infarction. In most facilities, current practice usually includes hospitalization, rest, combination antithrombotic medication, and maximal anti-ischemic therapy. Over the years, our understanding of its pathophysiology and the available tools have greatly improved. On the one hand, it is known that a substantial number of patients with ischemic symptoms, electrocardiographic changes, and/or troponin elevation have no coronary obstruction and, therefore, will not benefit from the same treatment as patients with rupture of atherosclerotic plaques. On the other hand, catheterization is currently the safest and most successful technique. In the first group, catheterization no longer carries an extremely high risk of local bleeding complications or a threat of acute occlusion, as the vessel is dilated by balloon angioplasty alone. Regarding the effectiveness of percutaneous coronary intervention (PCI), there is no longer the same risk of requiring repeat revascularization due to restenosis, as this has been corrected by drug-eluting stent placement in practically all PCI procedures. Moreover, newer models of drug-eluting stents are safer than bare-metal stents2,3 and have dramatically reduced the likelihood of late occlusion.
In the context of non–ST-segment elevation acute coronary syndrome (NSTE-ACS), invasive management has been analyzed in several ways: comparison of revascularization vs a conservative strategy, comparison of an early invasive strategy vs a selective invasive strategy, and comparison of a very early vs less early invasive strategy.
In the early 1990s, the first evaluation was designed as a randomized clinical trial to investigate the potential benefits of an early invasive vs conservative strategy (TIMI IIIB trial).4 The 2 study arms showed no significant differences in mortality or spontaneous myocardial infarction outcomes, but the study revealed a situation that would later be clearly involved in clinical practice and in subsequent research: symptom control and rehospitalizations often failed to improve in the conservative group, with over 70% of these patients also eventually undergoing catheterization, leading to similar revascularization rates in the 2 groups. In view of advances made in drug therapies and PCI techniques, there is no longer any controversy concerning the need to perform coronary angiography in patients with symptoms at rest, electrocardiographic changes, and elevated biomarkers. The debate now focuses on whether it is appropriate to wait for the situation to subside with antithrombotic medication and on whether angioplasty is safe in patients with unstable stenosis.
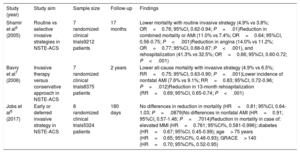
This issue is being addressed in several ongoing studies, each of which seem to report some equivalence between a very early strategy (with differing definitions of “very early”) and another, less expedited strategy. The prognostic difference between the 2 strategies proved to be significant only for patients at higher risk.5 Systematic reviews and meta-analyses of combined clinical trial outcomes6,7 tend to report that invasive therapy is beneficial (table 1). Consequently, clinical practice guidelines recommend cardiac catheterization within 24hours for patients with at least 1 high-risk criterion: elevated troponin levels consistent with infarction, dynamic ST/T changes, or GRACE (Global Registry of Acute Coronary Events) risk score> 140 (class IA, according to the 2018 Guidelines on Myocardial Revascularization of the European Society of Cardiology/European Association for Cardio-Thoracic Surgery).9 These recommendations are essentially based on the results of the TIMACS (Timing of Intervention in Acute Coronary Syndromes) study5 and the meta-analysis by Jobs et al.8 in 2017.
Meta-analyses comparing invasive strategies in non–ST-segment elevation acute coronary syndromes
| Study (year) | Study aim | Sample size | Follow-up | Findings |
|---|---|---|---|---|
| Shamir et al6 (2005) | Routine vs selective invasive strategies in NSTE-ACS | 7 randomized clinical trials9212 patients | 17 months | Lower mortality with routine invasive strategy (4.9% vs 3.8%; OR=0.76; 95%CI, 0.62-0.94; P=.01)Reduction in combined mortality or AMI (11.0% vs 7.4%; OR=0.64; 95%CI, 0.56-0.75; P<.001)Reduction in angina (14.0% vs 11.2%; OR=0.77; 95%CI, 0.68-0.87; P<.001), and rehospitalization (41.3% vs 32.5%; OR=0.66; 95%CI, 0.60-0.72; P<.001) |
| Bavry et al7 (2006) | Invasive therapy versus conservative approach in NSTE-ACS | 7 randomized clinical trials8375 patients | 2 years | Lower all-cause mortality with invasive strategy (4.9% vs 6.5%; RR=0.75; 95%CI, 0.63-0.90; P=.001)Lower incidence of nonfatal AMI (7.6% vs 9.1%; RR=0.83; 95%CI, 0.72-0.96; P=.012)Reduction in 13-month rehospitalization (RR=0.69; 95%CI, 0.65-0.74; P<.001) |
| Jobs et al8 (2017) | Early or deferred invasive strategy in NSTE-ACS | 8 randomized clinical trials5324 patients | 180 days | No differences in reduction in mortality (HR=0.81; 95%CI, 0.64-1.03; P=.0879)No differences in nonfatal AMI (HR=0.91; 95%CI, 0.57-1.46; P=.7014)Reduction in mortality in case of: elevated MMI (HR=0.761; 95%CI%, 0.581-0.996); diabetes (HR=0.67; 95%CI, 0.45-0.99); age> 75 years (HR=0.65; 95%CI%, 0.46-0.93); GRACE> 140 (HR=0.70; 95%CI%, 0.52-0.95) |
95%CI%, 95% confidence interval; AMI, acute myocardial infarction; HR, hazard ratio; MMI, markers of myocardial injury; NSTE-ACS, non–ST-segment elevation acute coronary syndrome; OR, odds ratio; RR, risk ratio.
The latest major clinical trial to contribute to the debate has been the VERDICT study.10 A total of 2147 patients from 9 hospitals were randomized to a revascularization strategy within the first 12hours of hospitalization or to standard care, with angiography performed within 48 to 72hours after admission. Both groups were given maximal anti-ischemic therapy, including early dual antiplatelet therapy with aspirin and ticagrelor. After a mean follow-up of 4.3 years, no differences were observed in the primary combined endpoint of all-cause mortality, recurrent myocardial infarction, or rehospitalization due to ischemia or heart failure. However, in the high-risk subgroup, predefined as GRACE risk score>140, the very early strategy (median time from diagnosis to revascularization, 4.7hours) achieved a 19% improvement, favoring patients who underwent almost immediate revascularization.
Consistent with this finding, a recent article published in Revista Española de Cardiología by the CARDIOCHUS-HUSJ group reports and discusses the results of a study between 2005 and 2016 that included 5673 patients with NSTE-ACS, performing propensity score matching to assign a total of 1890 to each group and then comparing the results of an invasive strategy within 24hours with the results for a strategy undertaken > 24hours after hospital arrival.11 In each group, matching resulted in 40% of patients with GRACE score> 140. Despite the initial adjustment for baseline characteristics, the 2 study groups exhibited relevant differences, such as a higher revascularization rate, both overall and with drug-eluting stents, and greater use of ticagrelor or prasugrel in the invasive therapy group <24hours The thorough analysis of the CARDIOCHUS-HUSJ investigators yielded similar conclusions on the benefit of the early invasive strategy in terms of all-cause mortality and cardiovascular mortality, after a mean follow-up of nearly 5 years, of 16.1% vs 21.5% (P<.001) and 10.9% vs 14.1% (P=.002), respectively. The benefit was mainly seen in the high-risk group (GRACE> 140). Following an adjustment for confounding variables, statistical significance was maintained in terms of the reduction in cardiovascular mortality (hazard ratio [HR]=0.79; 95% confidence interval [95%CI], 0.63-0.97), but not in all-cause mortality (HR=0.86; 95%CI, 0.71-1.05).
The limitations of this study have been accurately described by the authors. The observational nature implies inclusion biases that are impossible to control, even when using the detailed collection of baseline characteristics and propensity score matching described. For example, it would be difficult to control for situations where an expert cardiologist's initial diagnostic impression is severe diffuse ischemia or for situations where very frail or dependent elderly patients are being treated, or even for weekends when no interventional team is available and logistic difficulties could affect outcomes. Another aspect is the inclusion of patients since 2005, a time when the antithrombotic strategy used differed considerably from the current approach. An additional limitation is that only 8.4% of patients with coronary angiography performed within 24hours were treated with ticagrelor in this series.
A practical and important takeaway from the CARDIOCHUS-HUSJ registry is that it is certainly valid to apply the latest recommendations of the myocardial revascularization guidelines to real-world clinical practice. The evidence from this registry is consistent with the most recent randomized trials and suggests benefits of rapid management in very high risk patients that extend beyond the hospital phase.
What would be the optimal protocol design for patients with NSTE-ACS? At one end of the spectrum, there are very high-risk patients with hemodynamic or electric instability, refractory ischemia, or very extensive or recurrent ST-segment changes, who undoubtedly require emergency catheterization. A significant number of hospitalized patients have some evidence of high risk, such as elevated troponin levels or dynamic ST/T changes, age> 75 years, and GRACE risk score> 140. In such patients, the overall data, including those of the present study, indicate the clear benefit of prompt angiographic study, as early as within 12hours of arrival. At the other end of the spectrum, there are patients at intermediate risk who would probably not benefit in terms of “dismal” outcomes such as mortality or reinfarction but who would be helped by coronary angiography performed to determine the prognosis and therapeutic aggressiveness more precisely. In these patients, angiography as early as possible could at least shorten the hospital stay or prevent excessive antithrombotic therapy when clinical symptoms are not attributable to plaque rupture.
Several major points remain to be established when defining the protocol for the diagnostic strategy taken with NSTE-ACS. In low-risk patients consulting an emergency department with chest pain but with no clear electrical changes or definitive enzymatic changes indicating acute ischemia, prognostic stratification based on coronary computed tomography (CT) has been proven to have high negative predictive value in excluding acute coronary syndrome12 and has been shown to be safe (no differences in infarction or rehospitalizations).13 It remains to be seen whether or not coronary CT imaging is helpful in reclassifying patients with an intermediate risk profile, a topic under investigation by the VERDICT trial but with no results to date.10
Another unknown aspect is the impact of a routine early invasive strategy in frail elderly patients. This patient profile accounts for an increasing number of individuals known to be at higher ischemic and hemorrhagic risk.14 The MOSCA-FRAIL study,15 still in the recruitment phase, aims to elucidate whether or not the invasive approach is beneficial in patients with frailty defined as a Clinical Frailty Score ≥ 4.
The role of pretreatment with P2Y inhibitors12 in situations where catheterization is virtually an emergency vs situations where it can be deferred is another controversial point. Until new data are available to help clarify these questions, the therapy offered to patients will be based on large clinical trials and meta-analyses that, with studies such as this one, confirm the benefit, safety, and applicability of an invasive strategy undertaken as soon as possible.
CONFLICTS OF INTERESTNone declared.