It is widely accepted that echocardiography has been one of the most dramatic revolutions in the field of cardiology in the last 100 years. Among the noninvasive diagnostic procedures, the impact of this technique has been as profound as the revolution that occurred when Einthoven introduced the electrocardiogram, another foundation on which clinical diagnosis is based, and to which computed tomography and cardiac magnetic resonance imaging can be added.
The great advances in this technique in its different forms have spread to other areas within cardiac care units: the cardiac catheterization laboratory, coronary intensive care unit, cardiac surgery unit, emergency cardiac unit, and electrophysiology laboratory. In all these areas, when an echocardiogram is performed by a cardiologist with expertise in this technique and according to the clinical practice guidelines, the patient's condition is better understood, with important prognostic and therapeutic implications.
After the initial development of the technique in the field of cardiology in the 1990s, echocardiography became part of the arsenal of other specialties, mainly in the settings of anesthesia, resuscitation, and pediatric cardiology. In recent years, with the advent of portable and pocket-sized ultrasound devices, the technique has spread to other areas of medicine, leading to the current situation in which physicians without complete medical training in cardiology have the possibility of using these devices in their daily practice.1,2 Among other organizational problems, growth in the use of this technique requires the establishment of rational criteria and training to improve competency and quality in the exercise of our profession.
TRAINING AND ACCREDITATION IN ECHOCARDIOGRAPHY FOR CARDIOLOGISTSMany years ago, the Spanish Society of Cardiology specified accreditation standards and recommendations for appropriate training in echocardiography. Different skill levels were defined, with the aim of improving quality when performing echocardiographic studies.3
Thus, 3 levels of training were established:
- •
Level I is a requirement for all physicians who have specialized in cardiology and involves performing a minimum of 200 echo-Doppler studies under supervision. This training level allows the physician to perform and interpret studies under supervision.
- •
Level II extends the previous training by 3 months, involving an additional 200 echo-Doppler studies (totaling 400) as well as performing and interpreting 30 transesophageal echocardiography studies and 30 stress echo studies under supervision. This training level fully qualifies physicians to indicate, perform, and interpret echocardiographic studies.
- •
Finally, level III involves a further 6 months of training and qualifies the physician to manage an echocardiography laboratory and train others in the previous levels.
Similarly, the Cardiac Imaging Section has an established accreditation committee composed of experts in advanced echocardiography4 that sets out the minimum requirements and the procedures tested by written examinations to obtain this level of accreditation. The European Association of Cardiovascular Imaging has established not only an accreditation program for cardiologists,5 but an accreditation system for echocardiography laboratories with the aim of improving the quality of care.6 Among other aspects, these regulations and recommendations attempt to prevent organizational or resource availability problems from being the cause of misdiagnosis.
The aim of all these mechanisms to regulate the training and accreditation of cardiologists and echocardiography laboratories is to ensure that the physician is fully competent to perform these studies. Accreditation in any activity, and specifically in echocardiography, is a process that is often under-rated; nevertheless, it is of extreme importance, since it is designed to protect individuals against substandard practices or from personnel who lack the knowledge or skills to perform such studies.7
TRAINING AND ACCREDITATION IN ECHOCARDIOGRAPHY FOR OTHER SPECIALISTSAfter the initial development of echocardiography in the 1990s, use of the technique spread to other medical specialties and in particular to anesthesia. At the beginning, cardiologists who practiced this technique went to the operating room to resolve specific problems confronted by anesthetists during the induction of anesthesia or in the immediate postoperative period. Given the increasingly frequent requests for our presence in the operating room, this extra workload became difficult to sustain, leading us to train anesthesia teams which, after a training period supervised by cardiologists, began to perform the technique without our support or with our support only in specific cases. Given evidence of the need to regulate training, the Spanish Society of Cardiology and the Spanish Society of Anesthesiology published a set of norms to ensure that the training offered met the criteria and recommendations presented by both medical societies.8,9 This provides an excellent example of collaboration between scientific societies in their attempt to establish a consensus on appropriate training for anesthesiologists such that they can perform this technique safely and effectively.
Recently, the Cardiac Imaging Section of the Spanish Society of Cardiology, in collaboration with intensive care physicians, has defined the criteria for training in echography for this specialty, establishing a set of recommendations and proposals on the establishment of standardized training programs specific to echocardiography in intensive care units.3
MINIATURIZATION IN ECHOCARDIOGRAPHY: THE TECHNIQUE SPREADS BEYOND CARDIOLOGYIn recent years, the miniaturization of echocardiography devices has led to the emergence of 2 types of systems, with important implications for the training and practice of echocardiography:
- •
Portable devices: these are complete echocardiography systems that can be easily transported and operated in all echocardiography modalities: M mode, 2-dimensional echo, pulsed Doppler, continuous wave Doppler, tissue Doppler, and even myocardial deformation. Some have ports to accept transesophageal echocardiography probes. Obviously, the management of these machines requires the same level of training and qualification as the accreditation levels set by the Spanish Society of Cardiology, described above.
- •
Pocket-sized devices: these offer the basic modalities (usually 2D and color Doppler imaging),10,11 and their high portability and low cost has led to their widespread use outside the specific field of cardiology. Although technologically simple devices, they have proven useful as a complement to physical examination and may serve as a screening tool in different settings including anesthesiology, emergencies, family medicine, internal medicine, or even for training medical students.12,13 It should be obvious that this type of simple device will be used by a doctor who is not a specialist in cardiology and who also lacks the training needed to correctly perform echocardiography, with the risks that may be entailed. In fact, numerous studies have confirmed that although these devices are valuable in making a diagnosis, their sensitivity, and particularly their specificity, is strongly influenced by the level of training and experience of the operator, which may increase the risk of misdiagnosis.14 The position of the European Association of Cardiovascular Imaging is that this new generation of devices should be regarded as a tool to complement the initial examination of the patient and therefore no reimbursement to physicians should be warranted for their use.15
It is essential that scientific societies set and recommend norms of competence and provide information on the contexts in which these new devices can be used as well as their limits. Thus, the European Association of Cardiovascular Imaging,15 in response to concerns regarding the misuse and potential abuse of pocket-sized ultrasound devices, has promoted the idea of establishing specific training for this type of device. In addition, such training would include a refresher course in basic cardiac physiology and pathology and complete and accurate information on what the device is capable of and the limits beyond which it should not be used.
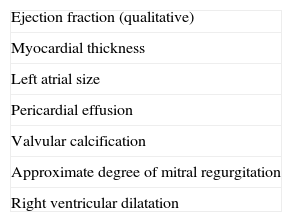
The user should be given a clear idea of the purpose and limitations of studies performed by a nonspecialist using a pocket-sized ultrasound device (Table 1). Similarly, it should be established what information the nonspecialist can obtain from these devices (Table 2). On the other hand, it is important to clarify that this type of study cannot replace a standard echocardiogram, which should be performed by an experienced cardiologist.
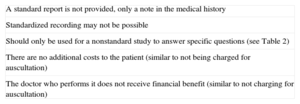
Description of a Study With a Pocket-sized Ultrasound Device Performed by Non-cardiologists
| A standard report is not provided, only a note in the medical history |
| Standardized recording may not be possible |
| Should only be used for a nonstandard study to answer specific questions (see Table 2) |
| There are no additional costs to the patient (similar to not being charged for auscultation) |
| The doctor who performs it does not receive financial benefit (similar to not charging for auscultation) |
Norms must be established regarding suitable training and skills to ensure that these devices can be reliably used by nonspecialists. In this respect, a proposal already exists that could serve as a starting point for regulation.14 A period of 3 days of basic theoretical training has been suggested (ultrasound physics, normal and pathological cardiac anatomy, normal and pathological fluid dynamics) followed by 60 days (3 days per week) in an echocardiography laboratory to complete the visual assessment of at least 150 studies. In addition, the European Association of Cardiovascular Imaging has recently created an online training course specifically for users of pocket-sized ultrasound devices; after training and an examination, students must submit proof of hands-on training in a hospital echography department.16
Clearly, we cannot stem the tide; pocket-sized ultrasound devices are here to stay and those who have participated in this technique becoming widespread have a moral obligation to regulate the training of those who use them. It is important to be able to convey, in practical terms, the limitations and benefits of this technique when these simple devices are used by physicians without specialized training.
There are a number of questions to be answered, and I suggest that this scientific society should be the one to respond:
- •
Who will provide non-cardiologists with regulated training in echocardiography using a pocket-sized ultrasound device?
- •
Who will provide training on the level of information that can be reliably obtained from these devices and which limits should not be exceeded?
- •
Will the trained physicians be able to stay within the limits of caution when using these devices?
- •
Who will teach them that they are not cardiologists or performing echocardiography and that what they do is not standard echocardiography, but an “echoscopy”?
- •
Should cardiologists be in charge of the training and set the boundaries?
- •
To what extent can primary care be improved and overload in tertiary-care echography laboratories be alleviated by the use of pocket-sized ultrasound devices by non-cardiologists?
- •
How serious will any diagnostic errors be if the guidelines are not adhered to?
- •
Can the tide be stemmed?
Reviewing these questions, I only have a clear answer to the last one: it is completely impossible to stem the tide. But I would like to add the following: limits can be set to regulate their use, thus leading to better medical practice, to the correct rather than incorrect use of the technology, and to improved patient outcomes.
CONFLICTS OF INTERESTNone declared.