To update the information on mortality from cardiovascular diseases and assess recent trends in Spain.
MethodsDeaths from cardiovascular diseases (codes I20-I25, I50, I05-I09, I00-I02, I26-I49, I51, I52, I60-I69, I10-I15, and I70-I79 of the 10th revision of the International Classification of Diseases and Causes of Death) were obtained from the National Statistics Institute. Trends were analyzed using Joinpoint regression models. The results revealed the years (periods) composing each trend, as well as the annual percent change for each of them. The direction and magnitude of recent trends (last available 5-year period) were assessed by using the average annual percent change.
ResultsThe decline in mortality rates from cardiovascular diseases slowed from −3.7% and −4.0% in 1999-2013 to −1.7% and −2.2% since 2013 in men and women, respectively. During the study period (1999-2018) all the analyzed causes decreased significantly. Nevertheless, recent trends differed according to age, sex, and the cause analyzed. Truncated rates (35-64 years) slowed (cardiovascular disease and stroke in men and ischemic heart disease in both sexes), stabilized (cardiovascular disease, stroke, and other heart diseases in women, and blood vessel disease in men), or increased (other diseases of the heart in men and diseases of the blood vessels in women).
ConclusionsIn Spain, as in other countries, the reduction in mortality rates from cardiovascular diseases slowed (overall rates for both sexes and truncated in men) or stabilized (truncated rates in women) from 2014 to 2018.
Keywords
Although global cardiovascular disease (CVD) mortality rates have decreased in recent decades (1990-2017), there has been an increase in the absolute number of CVD-related deaths. In men, for example, the global CVD mortality rate fell from 379.4 deaths per 100 000 population in 1990 to 275.5 per 100 000 population in 2017, representing a decline of 27.4%. In the same period, however, the number of CVD-related deaths increased by 54% (from 5.9 million to 9.3 million). In women, the global CVD mortality rate fell from 297.4 deaths per 100 000 population in 1990 to 196.1 per 100 000 population in 2017 (a decline of 34%), but again, the number of absolute deaths rose (from 6 million to 8.4 million, a 40% increase).1
CVD is the leading cause of death in Europe, where it causes more than 4 million deaths every year (46% of all deaths).2 Declines in ischemic heart disease (IHD) mortality have slowed in recent years among men from at least 1 age group in 15 European countries and a similar trend has been identified for women in 12 countries.3 Cerebrovascular disease (CeVD) mortality rates, in turn, have been decreasing for decades in most of Europe. Although the downward trend has held constant in over half of the countries, a recent study showed a slowing or flattening of the decline in CeVD mortality in a number of countries from the 4 geographic subregions of Europe, and in some countries, there was even an uptick in rates.4
Declines in mortality rates have also been reported in the United States for CVD,5 IHD6 (mainly in young adults), and CeVD.7
Although recent trends in standardized mortality rates for CVD,8,9 IHD,10 and CeVD11 in Spain have been analyzed, it is difficult to compare findings due to methodological differences (in standard populations, methods for estimating trends, international disease classifications, causes of death, etc) and a lack of studies on certain causes.
Joinpoint regression analysis12 has been widely used for a number of years to describe trends in disease incidence and mortality rates.
The aim of this study was to provide updated information on mortality rates for CVD and CVD subtypes in Spain between 1999 and 2018 and to examine recent trends using joinpoint regression.
MethodsInformation on CVD deaths was obtained from the Spanish National Institute of Statistics (INE)13 using the following codes from the 10th revision of the International Classification of Diseases and Causes of Death (ICD): I00-I99 (diseases of the circulatory system), I20-I25 (ischemic heart diseases), I50 (heart failure), I05-I09 (chronic rheumatic heart diseases), I00-I02, I26-I49, I51, I52 (other heart diseases), I60-I69 (cerebrovascular diseases), I10-I15 (hypertensive diseases), and I70-I79 (diseases of arteries, arterioles, and capillaries [blood vessel diseases]). The denominators (population estimates by age group on July 1 of each year) were also obtained from the INE. We calculated direct standardized rates (standard European population in 2013) for individuals of all ages (overall rates) and those aged 35 to 64 years (truncated rates). Rates were expressed as the number of annual deaths per 100 000 men.14 The truncated rates were used for comparisons with other studies, as they provide evidence of premature CVD deaths.
For the trend analysis, we used joinpoint regression models15 to identify periods marked by significant changes in mortality rates and to estimate the magnitude of the changes (increases or decreases) observed. The results show the beginning and end of each trend (first and last years) and the corresponding annual percent changes (APCs). To estimate the models, we entered the standardized rates and their standard errors and applied the default values in the Joinpoint program (minimum of 2 data points from the beginning to the end of a period, minimum of 2 data points between 2 inflection points (joinpoints), and maximum of 3 joinpoints). Geometrically weighted average APCs (AAPCs) were calculated from the APCs in the joinpoint model to quantify the trend for the whole period. An AAPC located entirely within a single joinpoint segment was considered to be equal to the APC for that segment. We also calculated AAPCs for the last 5 years of the study period to determine the direction and magnitude of recent trends. Results showing an increase or decrease in rates indicate statistically significant changes (P<.05), while those showing stabilization indicate nonsignificant changes.
All calculations and analyses were made in the Joinpoint Regression Program.16
ResultsCVD was the leading cause of death in Spain in 2018, accounting for 28.3% of all deaths registered (crude mortality rate, 258.6 deaths/100 000 population). It was followed by cancer (26.4%; 241.2 deaths/100 000 population) and respiratory diseases (12.6%; 114.9 deaths/100 000 population). When stratified by sex, CVD was the leading cause of death in women (crude mortality rate, 272.5 deaths/100 000 population) and the second leading cause in men (244.3 deaths/100 000 population).
Deaths attributed to the different subtypes of CVD for men and women in 1999 and 2018 are shown in table 1. The absolute number of deaths decreased in both sexes during the study period. On analyzing specific subtypes, we observed an increase in deaths due to heart failure, other heart diseases, and hypertensive diseases in men and to other heart diseases and hypertensive diseases in women.
Mortality due to cardiovascular disease in Spain, 1999-2018
| Men | Women | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1999 | 2018 | 1999 | 2018 | Change from 1999 to 2018 | ||||||
| No. | % | No. | % | No. | % | No. | % | Men | Women | |
| Coronary heart disease | 23.225 | 39% | 18.423 | 33% | 17.487 | 24% | 12.729 | 20% | –21% | –27% |
| Heart failure | 6.923 | 12% | 7.266 | 13% | 13.720 | 19% | 11.876 | 18% | 5% | –13% |
| Chronic rheumatic heart disease | 491 | 1% | 461 | 1% | 1.284 | 2% | 1.092 | 2% | –6% | –15% |
| Other heart diseases | 7.292 | 12% | 10.921 | 20% | 8.746 | 12% | 13.478 | 21% | 50% | 54% |
| Cerebrovascular disease | 16.074 | 27% | 11.435 | 20% | 22.656 | 32% | 14.985 | 23% | –29% | –34% |
| Hypertensive diseases | 1.547 | 3% | 4.108 | 7% | 3.364 | 5% | 8.388 | 13% | 166% | 149% |
| Blood vessel diseases | 4.430 | 7% | 3.348 | 6% | 4.535 | 6% | 2.349 | 4% | –24% | –48% |
| Cardiovascular disease | 59.982 | 55.962 | 71.792 | 64.897 | –7% | –10% | ||||
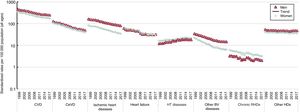
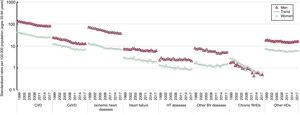
Sex-stratified CVD mortality rates for the period 1999 to 2018 are shown in figure 1 (overall rates) and figure 2 (truncated rates [35-64 years]), together with the trends estimated in the joinpoint analysis.
Sex-stratified CVD mortality rates in Spain for the period 1999 to 2018 showing overall standardized rates per 100 000 population for each year (all ages) and trends estimated using joinpoint analysis. BV, blood vessel; CeVD, cerebrovascular disease; CVD, cardiovascular disease; HDs, heart diseases; HT, hypertensive diseases; RHDs, rheumatic heart diseases.
AAPCs for men and women for the whole period (1999-2018) and the last 5 years (2014-2018) are given in table 2, together with the results of the joinpoint analysis for the different causes of death.
Sex-specific mortality due to cardiovascular disease in individuals of all ages in Spain (1999-2018) with AAPCs estimated by joinpoint analysis for the whole period and the last 5 years
| AACP | Trend 1 | Trend 2 | Trend 3 | |||||
|---|---|---|---|---|---|---|---|---|
| 1999/2018 | 2014/2018 | Period | APC | Period | APC | Period | APC | |
| Men | ||||||||
| Coronary heart disease | –3.8* | –3.8* | 1999-2018 | –3.8* | ||||
| Heart failure | –3.3* | –0.2 | 1999-2013 | –4.4* | 2013-2018 | –0.2 | ||
| Chronic rheumatic heart disease | –2.3* | –2.3* | 1999-2018 | –2.3* | ||||
| Other heart diseases | –0.3 | 1.0 | 1999-2013 | –0.8* | 2013-2018 | 1.0 | ||
| Cerebrovascular disease | –4.6* | –2.9* | 1999-2005 | –4.3* | 2005-2013 | –5.9* | 2013-2018 | –2.9* |
| Hypertensive diseases | 2.3* | –0.7 | 1999-2013 | 3.4* | 2013-2018 | –0.7 | ||
| Blood vessel diseases | –4.5* | –0.9 | 1999-2011 | –5.7* | 2011-2014 | –4* | 2014-2018 | –0.9 |
| Cardiovascular disease | –3.2* | –1.7* | 1999-2013 | –3.7* | 2013-2018 | –1.7* | ||
| Women | ||||||||
| Coronary heart disease | –4.5* | –5.0* | 1999-2003 | –2.5* | 2003-2018 | –5.0* | ||
| Heart failure | –4.0* | –0.9 | 1999-2014 | –4.9* | 2014-2018 | –0.9 | ||
| Chronic rheumatic heart disease | –3.0* | –3.0* | 1999-2018 | –3.0* | ||||
| Other heart diseases | –0.6* | –0.6* | 1999-2018 | –0.6* | ||||
| Cerebrovascular disease | –5.0* | –4.1* | 1999-2003 | –3.9* | 2003-2011 | –6.2* | 2011-2018 | –4.1* |
| Hypertensive diseases | 1.6* | –0.9 | 1999-2015 | 2.3* | 2015-2018 | –1.9 | ||
| Blood vessel diseases | –6.3* | –3.6* | 1999-2011 | –7.9* | 2011-2018 | –3.6* | ||
| Cardiovascular disease | –3.5* | –2.2* | 1999-2013 | –4.0* | 2013-2018 | –2.2* | ||
AAPC, average annual percent change for standardized rates (all ages); APC, annual percent change.
Standardized mortality rates in both sexes decreased significantly over the study period for all CVD subtypes except hypertensive and other heart diseases, although the decrease was slightly more pronounced in women. Hypertension-related mortality rates increased in both men and women while rates associated with other heart diseases remained stable.
The joinpoint analysis detected no significant downward trends in mortality rates for chronic rheumatic heart diseases in men or women, IHD in men, or other heart diseases in women. For men, it identified a slowing or flattening of the decline in mortality due to blood vessel diseases, hypertensive diseases, IHD, and other heart diseases in the period 2013 to 2014. For women, it detected a final period characterized by an increasing decline in mortality rates for IHD, a flattening of rates for heart failure, and a slowing of rates for CVD and CeVD.
The AAPCs calculated for men and women for the periods 1999 to 2018 and 2014 to 2018 are shown in table 3, together with the results of the joinpoint analysis for the different causes of death.
Sex-specific mortality due to cardiovascular disease in individuals aged 35 to 64 years in Spain (1999-2018) with AAPCs estimated by joinpoint analysis for the whole period and the last 5 years
| AACP | Trend 1 | Trend 2 | Trend 3 | |||||
|---|---|---|---|---|---|---|---|---|
| 1999/2018 | 2014/2018 | Period | APC | Period | APC | Period | APC | |
| Men | ||||||||
| Coronary heart disease | –3.4* | –1.9* | 1999-2011 | –4.3* | 2011-2018 | –1.9* | ||
| Heart failure | –1.3* | –1.3* | 1999-2018 | –1.3* | ||||
| Chronic rheumatic heart disease | –7.1* | –7.1* | 1999-2018 | –7.1* | ||||
| Other heart diseases | –0.6* | 2.2* | 1999-2013 | –1.6* | 2013-2018 | 2.2* | ||
| Cerebrovascular disease | –3.4* | –1.4* | 1999-2007 | –3.4* | 2007-2011 | –6.9* | 2011-2018 | –1.4* |
| Hypertensive diseases | –0.6* | –0.6* | 1999-2018 | –0.6* | ||||
| Blood vessel diseases | –2.3* | 2.3 | 1999-2014 | –3.5* | 2014-2018 | 2.3 | ||
| Cardiovascular disease | –2.7* | –0.8* | 1999-2008 | –3.3* | 2008-2011 | –5.3* | 2011-2018 | –0.8* |
| Women | ||||||||
| Coronary heart disease | –3.2* | –1.3* | 1999-2010 | –4.6* | 2010-2018 | –1.3* | ||
| Heart failure | –2.3* | –2.3* | 1999-2018 | –2.3* | ||||
| Chronic rheumatic heart disease | –8.7* | –8.7* | 1999-2018 | –8.7* | ||||
| Other heart diseases | –0.8* | 1.5 | 1999-2012 | –1.9* | 2012-2018 | 1.5 | ||
| Cerebrovascular disease | –3.2* | 0.2 | 1999-2014 | –4.1* | 2014-2018 | 0.2 | ||
| Hypertensive diseases | –2.2* | –2.2* | 1999-2018 | –2.2* | ||||
| Blood vessel diseases | –0.6 | 3.0* | 1999-2010 | –3.2* | 2010-2018 | 3.0* | ||
| Cardiovascular disease | –2.7* | –0.7 | 1999-2011 | –3.9* | 2011-2018 | –0.7 | ||
AAPC, average annual percent change for standardized rates (all individuals aged 35-64 years); APC, annual percent change.
Mortality rates for all CVD causes decreased significantly between 1999 and 2018. Nonetheless, analysis of more recent trends (2014-2018), showed a plateauing of truncated mortality rates for CVD, CeVD, and other heart diseases in women and blood vessel diseases in men and a significant increase in rates for other heart diseases in men and blood vessel diseases in women.
No changes in declining mortality rates were observed in the joinpoint analysis for either men or women for chronic rheumatic heart diseases, hypertensive diseases, or heart failure. In men, the analysis detected a slowing of the decline in mortality for CVD, CeVD, and IHD in the period 2011 to 2018 and an increase in mortality rates associated with other heart diseases for the period 2013 to 2018. In women, we observed a final period characterized by a slowing of the decline in mortality rates for heart failure, a flattening of rates for CVD and CeVD disease, and an increase in rates for blood vessel diseases.
DiscussionCVD deaths are increasing worldwide due to population growth and aging, as well as changes in the epidemiology of the disease. Determining how each of these 3 factors affects mortality trends is important for informing policy choices and tracking progress toward reducing CVD.17 Although Spain's population is also growing and aging, the country has seen a slight decrease in total CVD deaths, mainly attributable to the reduction in CeVD deaths, which has offset the increase in hypertension-related deaths and deaths due to other heart diseases.
Spain has lagged behind other countries in terms of reducing CVD mortality and risk factors, as it took longer for smoking and obesity to reach epidemic levels.18 Unfortunately, little is known about trends in the incidence and prevalence of the main cardiovascular risk factors in Spain,19,20 although smoking–followed by hypertension, obesity, and diabetes—is by far the main factor.21
In the United States, the rate of decline in IHD mortality among young adults (35-54 years) has been slowing since the early 1980s, and in the overall population it began to level off in both men and women in early 2000.22 Similar patterns, starting in the mid 1990s, have been reported for England and Wales,23 Scotland,24 and Australia.25 The patterns for Spain are similar, but with a time lag of 1 to 2 decades. Our findings show that the decline in truncated mortality rates are slowing for both sexes (table 3 and figure 2).
Sex-stratified CVD mortality rates in Spain for the period 1999 to 2018 showing truncated standardized rates per 100 000 population for each year (individuals aged 35-64 years) and trends estimated using joinpoint analysis. BV, blood vessel; CeVD, cerebrovascular disease; CVD, cardiovascular disease; HDs, heart diseases; HT, hypertensive diseases; RHDs, rheumatic heart diseases.
Our findings show that Spain, like other countries, has experienced a slowing of the decline in overall CVD mortality in both men and women. The decline in truncated rates, in turn, has slowed for men and reached a plateau for women. These findings concur with those of a recent study showing an overall decline in CVD mortality for men and women in Spain as a whole, but a slowing in the decline for women in Andalusia, a plateauing for men and women in Murcia, men in Castile-La Mancha, and women in Extremadura, and an increase for men and women in the Canary Islands.26
Slowing and halting declines in IHD and CeVD mortality have been attributed to an increase in risk factors among young adults in recent years.27 About 50% of the decrease in IHD mortality in Spain has been attributed to a reduction in risk factors while the other 50% has been attributed to improved treatments.10
The hypertensive diseases analyzed in our study included essential (primary) hypertension (ICD code I10), hypertensive heart disease (I11), hypertensive chronic kidney disease (I12), hypertensive heart and chronic kidney disease (I13), and secondary hypertension (I15).
Several countries have reported a recent increase in hypertension-related mortality attributed to increases in the prevalence of hyperhypertension.28,29 In the United States, for example, hypertension-related mortality increased by 36.5% from 1999 to 2016, with an AAPC of 1.8% for individuals aged more than over 35 years. The increase, with an AAPC of 2.7%, was even higher for the period 2011-2017.30 In our series, overall mortality due to hypertensive diseases plateaued after an initial period of decline in both men and women, while truncated rates decreased significantly throughout the study period, although more so in women than in men. The favorable trend observed in individuals aged 35 to 64 years may largely be due to the improved treatment of hypertension. Nonetheless, the absolute number of hypertension-related deaths showed a sharp increase in both sexes between 1999 and 2018 (table 1).
Chronic rheumatic heart disease has traditionally been a major cause of CVD morbidity and mortality in Spain, particularly in younger individuals (aged 5-30 years).31 Nowadays, however, it accounts for just 1% of all CVD deaths in both sexes. We also observed a downward trend in mortality attributed to chronic rheumatic heart disease over the study period for men and women overall and for individuals aged 35 to 64 years. This decrease is probably a reflection of improvements in living standards, diagnosis, and treatment.
Heart failure is a serious medical and economic public health problem,32 affecting 1% to 2% of people in Europe and 5% to 7% of those in Spain.33 Its prevalence has increased in recent decades and is expected to increase even further due to aging populations in Western societies and longer survival of patients with coronary events.
A study of trends in deaths attributed to heart failure in 7 European countries between 1987 and 2008 found that the greatest decrease in mortality (≥ 40%) occurred in the 4 countries with the highest initial rates (≥ 40 deaths/100 000 population in 1987): France, Germany, Greece, and Spain. The decrease was accompanied by a rise in the mean age at death, and one of the possible reasons identified by the authors of the study was improved management of heart failure in recent years. Nonetheless, heart failure mortality rates remained stable in England, Wales, Finland, and Sweden, which all had an initial rate of fewer than 25 deaths per 100 000 population.34
In the United States, mortality rates for heart failure and other heart diseases fell between 2000 and 2011, but after this point, they showed respective increases of 3.7% and 1.9%.35
Our results for Spain show that overall mortality rates for heart failure leveled off after an initial period of marked decline (1999-2013/2014). The decline in truncated rates, by contrast, held constant during the study period. This observation is consistent with the results of a recent study showing a decrease in mortality rates associated with premature heart failure (0-75 years) between 1999 and 2013 in certain regions of Spain and in the country as a whole. Moreover, the decrease was more pronounced in women than in men.36 Our analysis also showed that overall mortality rates for other heart diseases reached a plateau in men in 2013, while truncated rates showed a significant uptick, starting in 2012. Overall, however, mortality due to heart failure decreased slightly over the study period.
Few studies have analyzed the incidence and trends of CVD in Spain. Among these is a population-based study that analyzed trends in acute myocardial infarction incidence and mortality in the province of Girona.37 Mortality data thus are the only source of nationwide data that can be compared over periods of time.
We have analyzed trends in mortality rates for CVD and CVD subtypes (eg, CeVD, CHD, heart failure, hypertensive diseases) over a long period (20 years) using joinpoint regression analysis. This method allows objective analysis of trends as it eliminates the need to establish predefined periods, thereby reducing the risk of bias.
Our study has some limitations, including potentially inaccurate estimation of trends due to the inaccuracy of death certificates or changes to systems used to classify causes of death. Nonetheless, the quality of cause-specific mortality statistics in Spain has improved over the years and is now rated as generically high.38 Moreover, statistics for certain CVDs have been demonstrated to be highly reliable.39
Heart failure is, to a certain extent, a poorly defined cause and is listed as such in the updated ICD-10 instructions manual.40 Although the World Health Organization advises against listing heart failure as a basic cause of death, a considerable proportion of all CVD deaths in Spain (16% in our series) are attributed to this condition. Our findings show that deaths due to heart failure decreased over the study period for both men and women aged 35 to 64 years (table 3). This suggests that the slowing of the decline observed overall is largely due to higher mortality rates in older people, who have more comorbidities and are more likely to have less accurate death certificates. While death records have shortcomings as a source of data, they are used in Spain36 and other countries.34
Identifying the causes of heart failure is not always easy.41 In future studies on heart failure mortality, it would be interesting to revise individual death certificates listing multiple causes to identify other plausible causes.42
To avoid possible discrepancies caused by the use of different classification systems, we limited our analyses to the period 1999 to 2018, when only the ICD-10 was in use.
A final limitation of our study is that it was designed to describe trends in CVD mortality and not to explain reasons for any trends identified. Given the ecological design of our study (aggregate-level data), any inferences suggested by the data are also at the aggregate level. Individual-level interferences would result in an ecological fallacy. Based on our data, we can make hypotheses, not inferences, but these will need to be demonstrated in future studies. Accordingly, it is not possible to claim that any of the trends detected are associated (or not associated) with given factors.
Further studies are needed to gain a better understanding of the causes underlying the trends detected in our study in order to optimize health care interventions.
ConclusionsSpain, like other countries, experienced a slowing of the decline in overall CVD mortality rates for men and women and in truncated rates for men and a leveling off of truncated rates for women between 2014 and 2018.
FundingNo funding was received for this study.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
- -
Recent changes have been observed in declining CVD mortality rates, namely a) a slowing of the rate of decline in CHD mortality and b) a slowing, leveling off, and even reversal of the decline in CeVD mortality.
- -
Although trends in mortality rates for CVD and CVD subtypes have been analyzed, results are difficult to compare because of methodological differences and a lack of information on certain diseases (eg, hypertensive diseases) and more recent trends.
- -
This study provides updated information on age- and sex-stratified mortality rates associated with CVD and CVD subtypes (including causes not yet analyzed in the literature) in Spain over a long (20-year) period. The use of rates standardized to a standard European population will facilitate comparisons with other studies. Spain, like other countries, experienced a slowing of the decline in overall CVD mortality rates for men and women and in truncated rates for men and a leveling off of truncated rates for women between 2014 and 2018.