The Spanish League of Clinical Cases,1 an educational activity of the Spanish Society of Cardiology that has been running for more than 10 years has been an undoubted success. With a format the mimics a football tournament, combining an entertaining but competitive atmosphere with clear rules and high-quality content, the League has clearly stimulated the training of many of our youngest cardiologists. Revista Española de Cardiología wanted to contribute to this recognition by publishing the case, “Exertional dyspnea following lumbar microdiscectomy2”. In line with the sporting spirit of the League, I wish to begin by congratulating Dr Rojas Brito and her colleagues in the Hospital Insular de Gran Canaria for the value of the case and the multiple lessons that it highlights, some already noted by the authors and others that I will attempt to illustrate here.
HIGH-OUTPUT HEART FAILUREOne of the advantages of this case is that it calls attention to an uncommon heart failure (HF) phenotype that should nonetheless be recognized and remembered by all cardiologists, given that we will surely encounter more than one of these patients during our careers. In a series of 16 462 patients with HF who underwent a hemodynamic assessment over a 15-year period in the Mayo Clinic,3 almost 3% had indicators of high-output HF (HOHF). Strikingly, these patients exhibit clinical data typical of HF (eg, in this case, dyspnea, orthopnea, crackles, jugular venous distension, edemas) but have few electrocardiographic and echocardiographic abnormalities.
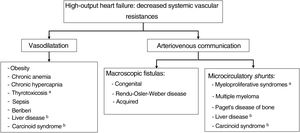
This is undoubtedly due to the pathophysiological peculiarities of HOHF, which are distinct from those of other HF types: the fundamental problem lies in the presence of decreased systemic vascular resistances, which can coexist with a normal heart during the initial stages of the disease.4 These resistances can be due to arteriovenous communications (whether macroscopic fistulas or microvascular shunts) or generalized vasodilation. All of this culminates in a hypotensive state that activates the neurohormonal mechanisms found in all types of HF, which include the sympathetic system and the renin-angiotensin-aldosterone system. This triggers various processes, including water and sodium retention, interstitial fibrosis, myocardial toxicity, relative vasoconstriction, and ventricular remodeling, which lead to clinically relevant HF. Another mechanism possibly contributing to HOHF is a state of hypermetabolism, as reflected by hyperthyroidism and myeloproliferative syndromes.
The schematic shown in figure 1 helps to explain and highlight the most frequent causes of HOHF. The etiological profile of HOHF has changed over time, given that conditions such as beriberi, anemias, and hyperthyroidism, common in the previous century, have given way to obesity, congenital or acquired fistulas, and liver disease as the most common current causes of the condition.3–5 Recent publications distinguish 2 phenotypes of HOHF, that is, with and without cardiac cavity dilatation, which can be phases of the disease in the same patient, independently of the symptom etiology.
HOHF has distinctive features that must be known to avoid it being overlooked: as mentioned above, patients have a similar clinical picture and natriuretic peptide elevation to other HF phenotypes but the results of other complementary tests can be misleading if this entity is not considered. The electrocardiogram may be normal, which is exceptional in other forms of HF, and the echocardiogram usually shows normal left ventricular systolic function, which can suggest other more frequent causes of HF with preserved ejection fraction (HFpEF), as indicated by Obokata et al.5 in their excellent review. In addition, patients with HOHF usually have an elevated E/e’ ratio, reflecting their diastolic dysfunction, and their estimated pulmonary artery systolic pressure is invariably elevated, findings common in HFpEF.3,5 The difficulty is extreme in patients without cavity dilatation, which is frequent in the initial stages of the disease.6 The key to diagnosis is estimation of the cardiac output on echocardiography, as performed by the authors of the case discussed here. According to Reddy et al.,3 an estimated cardiac index on echocardiography > 3.5 L/min/m2 should lead to disease confirmation via direct measurement of pressures, oximetry, and cardiac output on right heart catheterization. Notably, the authors’ reasoning, namely, that the elevated venous saturation had to be explained by an atrioventricular fistula, is not always correct (although it was in this case); in the context of high cardiac output not due to a fistula, it is typical to encounter venous oxygen levels > 75% due to lower oxygen extraction from tissue due to vasodilation or microvascular shunts.
We must also underline the huge impact of HOHF diagnosis: in the Mayo Clinic series, the 3-year mortality was 38%, much higher than that of the control group without heart disease.3 Curative treatment requires correction of the disease causing the high output, as in the present case. Regarding drug therapy, it seems that only diuretic agents ameliorate the symptoms. Renin-angiotensin-aldosterone system inhibitors and beta-blockers with vasodilatory effects should be avoided because a reduction in vascular resistance can worsen the symptoms.
THE OLD VS THE NEW CARDIOLOGYI believe that the case also permits a reflection on the current diagnostic process in cardiology. After a quick description of the patient's history and symptoms, the authors report various exploratory findings, some typical of HF and others highly unusual in this context, such as tachycardia and abdominal murmur, which are not described any further. They rapidly move to reporting the blood test, electrocardiogram, and cardiac ultrasound results. The findings of the latter modality led to more detailed echocardiographic studies, including indication of an elevated cardiac output, which gave the cardiologists the clue to the correct diagnosis.
I doubt that any of the fantastic clinical cardiologists with whom I have had the luck of learning from (eg, Drs Luis Alonso-Pulpón, Francisco Javier Ortigosa, and Pedro Zarco) would have considered an abdominal murmur with such striking systolic and diastolic components as being anything other than a fistula. Moreover, in Dr Pulpón's case, there is even evidence (figure 2) of how he identified a fistula murmur by exploring the splenic area of a patient with HOHF and major visceromegaly in the context of myeloproliferative syndrome and myelofibrosis. Returning to our case, HF symptoms together with a fistula murmur appearing shortly after an intervention in this region would surely have led our maestros to deduce the true origin of the disease long before the performance of complementary tests. The worth of the clinician giants does not lie in their particular “skill” in auscultation (which they had), but in their use of the most powerful weapon available to cardiologists for diagnosis: clinical reasoning based on a solid understanding of pathophysiology.
Do not misunderstand—this does not constitute a naïve request to return to the old way of cardiology based on patient examination: we have never been so able to diagnose heart diseases with such speed and accuracy as now, with different echocardiogram modes giving us access to accurate and quantitative data on the anatomy and function of all cardiac structures. But this should not discourage or impede clinical reasoning based on all available data. The phonendoscope, that instrument whose main function is now to differentiate the cardiologists who wear it around their neck from the other species who populate the hospital ecosystem, can still provide immediate and highly valuable information when it is correctly used at the bedside.
When, within a few short years, all cardiologists have replaced the phonendoscope with an ultrasound transducer connected to their smartphones, the aphorism that separates the classic masters will still be valid, and I like to repeat it to our residents: “To become a good cardiologist, you must master one or more of the diagnostic and therapeutic techniques of our specialty, but you can only become one of the best if you keep an alert mind that combines knowledge with clinical reasoning”.
FUNDINGThis work did not receive funding.
CONFLICTS OF INTERESTThe author has no conflict of interest to declare.