In young patients with severe aortic stenosis, it is unknown whether their life expectancy restored after aortic valve replacement (AVR) is unknown.
MethodsWe analyzed all patients aged between 50 and 65 years who underwent isolated AVR in 27 Spanish centers during an 18-year period. We compared observed and expected survival at 15 years of follow-up. We repeated all analyses for patients without complications in the postoperative period.
ResultsA total of 5084 patients were analyzed. For the overall sample, observed survival at 10 and 15 years was 85.3% (95%CI, 84.1%-86.4%) and 73.7% (95%CI, 71.6%-75.6%), respectively. Expected survival was 90.1% and 82.1%. Cumulative relative survival for 1, 5, 10 and 15 years of follow-up was 97.4% (95%CI, 96.9%-97.9%), 96.5% (95%CI, 95.7%-97.3%), 94.7% (95%CI, 93.3%-95.9%), and 89.8% (95%CI, 87.3%-92.1%). For patients without complications, cumulative relative survival for 1, 5, 10 and 15 years was 100.3% (95%CI, 99.8%-100.5%), 98.9% (95%CI 97.6% -99.9%), 97.3% (95%CI, 94.9%-99.4%), and 91.9% (95%CI, 86.5%-96.8%).
ConclusionsLife expectancy in young patients who have severe aortic stenosis and undergo AVR is lower than that of the general population. Life expectancy of individuals without complications during the postoperative period is also reduced. Therefore, baseline characteristics are likely the main factors that explain the reduction in life expectancy.
Keywords
Aortic valve replacement (AVR) has been shown to modify the natural history of symptomatic severe aortic stenosis (SAS). After this procedure, life expectancy has been historically considered similar to that of the general population. However, some studies have recently observed a loss in life expectancy after this procedure, suggesting that surgery is not completely effective in resolving the problem.1–3 The observed life expectancy was slightly lower than expected in elderly patients but was much lower than expected in young individuals. Because SAS is a disease of the elderly, the reported samples of young patients were small. Other studies, however, showed an excellent long-term prognosis after AVR, especially in elderly patients surviving the postoperative period.4,5 Many studies have analyzed the long-term survival of patients undergoing AVR, but without comparison with the survival data of the general population, these survival data provide little information.3,5
Determining whether patients with SAS can enjoy a life expectancy similar to that of the general population after AVR is of utmost importance for patient information, informed consent, and medical decision making. Physicians, surgeons, patients and experts have recently requested the analysis of larger cohorts in other nations to decide if there really is a reduction in life expectancy and to investigate possible reasons.1,2
We used a nationwide cohort to analyze the excess mortality in young patients (50-65 years) who underwent isolated AVR and compared their long-term survival with that of the general population of the same age, sex, year of surgery, and nation. To further understand the phenomenon, we calculated these measures in patients without complications.
METHODSSelection of the sampleWe used a national multicenter registry including all patients aged from 50 to 65 years who underwent isolated AVR in 27 Spanish centers during January 2000 and September 2018. We excluded dndocarditis, nonelective interventions and surgery due to isolated aortic regurgitation. Each center had 2 researchers responsible for collecting pre-, intra-, postoperative data and follow-up in all patients. The variables collected in this registry were reported for another study at ClinicalTrials.gov: NCT03595423. Follow-up was collected from February to July 2019. Telephone contacts with the patient/family, contacts with their physicians and information based on medical reports were used. Only 3 patients were lost to follow-up. For these patients, we considered the last date they were known to be alive.
We compared the long-term observed survival of these patients who underwent isolated AVR with the expected survival of the general population from Spain matched by age, sex, and year of surgery. To match for these factors, we used the data freely available and provided by the National Institute of Statistics.6 This method has been previously used.1
In an attempt to expand knowledge, we selected another sample and repeated all analyses. This sample was formed by patients who survived the postoperative period, did not suffer major postoperative complications and who were able to have a straightforward postoperative course. These individuals did not have a permanent pacemaker, aortic regurgitation (mild or more severe), stroke, new-onset atrial fibrillation, and their ventricular function did not worsen more than 10% compared with previous function and the total hospital stay was less than 10 days.
This study complies with the Declaration of Helsinki, was approved by the IRB (Comité de Ética de Investigación de Málaga, reference: 2806/2018, informed consent was not needed due to the retrospective nature of the study) and the design, aims and main estimates were registered online.7
Primary endpointsTo compare observed with expected survival in patients aged 50 to 65 years who underwent isolated AVR.
To determine whether the long-term survival of patients aged 50 to 65 years who underwent isolated AVR, survived the postoperative period and had no postoperative complications was similar to that of the general population.
Secondary endpointsTo Identify the main risk factors for long-term mortality in this population.
Statistical analysisCategorical and quantitative variables are described as No. (%) and mean±SD, respectively. We compared observed survival, calculated by the usual actuarial estimate (intervals of 0.1 years), with expected survival, calculated by the Ederer II method. This method, considered the best for this purpose,8 is able to estimate the expected survival of the sample in the theorical assumption that they did not have the disease. This method was previously used in other works.1,9,10 If the 95% confidence interval (95%CI) of the observed survival included the expected survival, no difference can be shown. For the calculations, we used the data provided by the National Institute of Statistics.6 With these data, we created a database with the annual risk of death by sex, year (2000-2019), and age (50-84 years).
The mortality in a sample may be due to the disease under study or to other unrelated causes. Consequently, usual Kaplan-Meier survival curves, without comparison with the general population, provide little information. One method that estimates the proportion of patients who die only due to the disease is the relative survival (RS). An RS of 100% indicates that there are no deaths related to the disease (all patients survive). An RS of 60% would indicate that 40% of the patients died because of the disease.1,11–13 We calculated the RS with its 95%CI. If the CI includes the value 100%, no excess of mortality can be shown. RS results from the division between the observed and the expected survival and therefore it can exceed 100%.
Risk factors for long-term mortality were identified using a multivariate Cox-regression analysis. All baseline characteristics were included in the model and the proportion hazards assumption was tested.
All analyses were performed with STATA v.15 (StataCorp, United States) and the strs12 command was used to calculate these estimates.
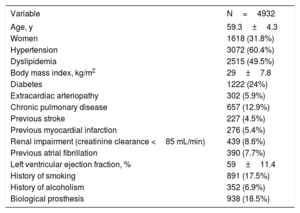
RESULTSOverall sampleA total of 5084 patients underwent isolated AVR during the study period. The mean age was 59.3±4.3 years and 1618 (31.8%) were women. Baseline characteristics are described in table 1. In all, 152 (2.99%) patients died during the postoperative period with a logistic EuroSCORE of 3.1±7.5.
Patient characteristics
| Variable | N=4932 |
|---|---|
| Age, y | 59.3±4.3 |
| Women | 1618 (31.8%) |
| Hypertension | 3072 (60.4%) |
| Dyslipidemia | 2515 (49.5%) |
| Body mass index, kg/m2 | 29±7.8 |
| Diabetes | 1222 (24%) |
| Extracardiac arteriopathy | 302 (5.9%) |
| Chronic pulmonary disease | 657 (12.9%) |
| Previous stroke | 227 (4.5%) |
| Previous myocardial infarction | 276 (5.4%) |
| Renal impairment (creatinine clearance <85 mL/min) | 439 (8.6%) |
| Previous atrial fibrillation | 390 (7.7%) |
| Left ventricular ejection fraction, % | 59±11.4 |
| History of smoking | 891 (17.5%) |
| History of alcoholism | 352 (6.9%) |
| Biological prosthesis | 938 (18.5%) |
The data are expressed as No. (%) or mean±standard deviation.
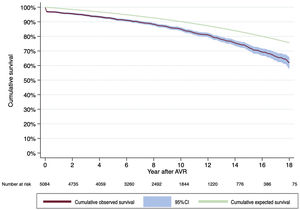
Median follow-up of the censored observations was 97.6 months. Observed survival at 1, 5, 10 and 15 years of follow-up was 96.7% (95%CI, 96.2%-97.2%), 92.5% (95%CI, 91.7%-93.2%), 85.3% (95%CI, 84.1%-86.4%), and 73.7% (95%CI, 71.6%-75.6%). Expected survival for these years was 99.3%, 95.9%, 90.1%, and 82.1%. Observed and expected survival curves are represented in figure 1.
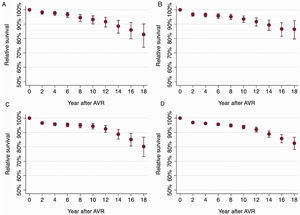
The cumulative RS for 1, 5, 10 and 15 years of follow-up was 97.4% (95%CI, 96.9%-97.9%), 96.5% (95%CI, 95.7%-97.3%), 94.7% (95%CI, 93.3%-95.9%), and 89.8% (95%CI, 87.3%-92.1%). The cumulative RS for different years of follow-up and stratified by age ranges can be observed in figure 2A-D.
The same analyses were performed for patients who survived the postoperative period (Results and ). Stratified analyses by sex and type of prosthesis were also calculated (). In addition, the main risk factors for long-term mortality are shown in Results of the supplementary data.
Patients who survived the postoperative period without complicationsA total of 1657 fulfilled the criteria. The mean age was 59.4±4.4 years and 517 (31.2%) were women.
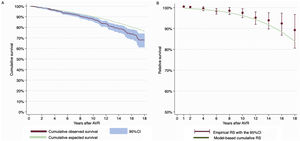
Observed survival at 1, 5, 10 and 15 years was 99.6% (95%CI, 99.1%-99.8%), 94.8% (95%CI, 93.5%-95.8%), 87.8% (95%CI, 85.6%-89.7%), and 75.7% (95%CI, 71.1%-79.6%). Expected survival at 1, 5, 10 and 15 years was 99.3%, 95.9%, 90.2%, and 82.2%. Observed and expected survival curves are shown in figure 3A.
Cumulative RS for 1, 5, 10 and 15 years was 100.3% (95%CI, 99.8%-100.5%), 98.9% (95%CI, 97.6%-99.9%), 97.3% (95%CI, 94.9%-99.4%), and 91.9% (95%CI, 86.5%-96.8%). Cumulative RS during the follow-up is presented in figure 3B.
Stratified analyses by sex and type of prosthesis were also calculated. These results can be consulted in . The number of complications by patient can be consulted in the .
DISCUSSIONThe main finding of this work is that survival of patients who undergo AVR was lower than that of the general population of the same age and sex. Interestingly, this finding was repeated for patients without postoperative complications.
Glaser et al.1 analyzed the life expectancy of 2000 patients aged between 50 and 60 years who underwent AVR (isolated or concomitant with coronary surgery). Using the same methodology as ours, they showed that these patients did not have their life expectancy restored. Almost 5000 patients aged between 50 and 65 years who underwent isolated AVR in Spain were analyzed for this work. We observed that around 10% of our patients had died due to the SAS or related factors 15 years after the problem was supposedly solved. Consistent with other studies, the excess mortality was higher in younger patients and decreased with age (figure 2).
To determine whether this excess mortality was due to the surgery, we selected another group. This group was formed by patients who underwent AVR, survived the operation and had a short hospital stay and a postoperative course without complications. The observed survival of patients in this group was lower than expected survival for the same age and sex. Similar to the results of the overall sample, the excess mortality in this group was around 10%. This means that an easy, successful and straightforward intervention cannot provide a life expectancy similar to that of the general population. The reasons are unknown but patients with SAS may have comorbidities that reduce life expectancy compared with that in the general population.
In young patients, biological prostheses are usually selected in those with comorbidities or reduced life expectancy. Compared with patients with mechanical prosthesis, those with biological valves had greater loss in life expectancy.
The RS is a regular measure in the setting of cancer and requires the assumption that the survival of patients with cancer would be the same as that of the general population if they did not have cancer. For many types of cancer, this is a reasonable assumption, but SAS is associated with several risk factors.11 Risk factors associated with the development of aortic stenosis are older age, male sex, elevated levels of serum low-density lipoprotein cholesterol, smoking, renal failure, and diabetes.14 The first 2 are usually controlled for in studies comparing the life expectancy of a sample with the general population.1,3,9,10,15 However, the remaining possible risk factors are not taken into account in the data of the different institutes of statistics.
Patients undergoing AVR frequently enquire about their life expectancy after surgery. According to the results of our study, compared with the general population, most patients will have a reduced life expectancy, even though the surgery goes well and their postoperative course is without complications.
Strengths and limitationsIn this study, we present the largest sample of relatively young patients undergoing AVR and compared their long-term survival with that of the general population matched by age, sex, year of surgery, and nation. Our sample was formed only by isolated AVR and therefore it is more homogeneous than that presented in other samples with concomitant coronary surgery.
However, this study has several limitations. This is a retrospective work and is therefore subject to intrinsic biases of this type of study. There was no objective way to know whether patients’ surgery was easy and straightforward. We selected this group of patients based on the available postoperative variables. Nevertheless, we acknowledge that the selection of these factors was substantially subjective. Some important postoperative complications such as reoperation due to severe bleeding were not present in the registry so we could not take them into account. Finally, different centers may lead to different surgical results and our conclusions are only an average of the observed and expected survival at the national level.
CONCLUSIONSIn conclusion, life expectancy in patients with SAS who undergo AVR is not similar to that of the general population. Patients without postoperative complications also have excess mortality during long-term follow-up. The cause for this excess mortality does not seem to be complications related to the surgery. Medical efforts should be directed at controlling cardiovascular risk factors and the comorbidities that accompany this disease.
- -
Aortic valve replacement is able to change the natural history of severe aortic stenosis. However, it is not known whether the intervention is able to restore patients’ life expectancy.
- -
Life expectancy in young patients undergoing aortic valve replacement is not similar to that of the general population of the same age, sex, year, and nation. Life expectancy is not restored in patients who survive the postoperative course and who do not have complications. This study suggests that the possible complications during the postoperative course are not the main cause for this reduction in life expectancy.
None
AUTHORS’ CONTRIBUTIONSD. Hernandez-Vaquero: design and analysis of the work, drafting the manuscript. E. Rodríguez-Caulo: design and analysis of the work, drafting the manuscript. C. Vigil-Escalera: design, data acquisition, drafting the manuscript. Ó. Blanco-Herrera: data acquisition, review of the manuscript E. Berastegui: Data acquisition, review of the manuscript. J. Arias-Dachary: data acquisition, review of the manuscript. S. Souaf: data acquisition, review of the manuscript. G. Parody: data acquisition, review of the manuscript. G. Laguna: data acquisition, review of the manuscript. A. Adsuar: data acquisition, review of the manuscript. M. Castellá: data acquisition, review of the manuscript. J. Valderrama: data acquisition, review of the manuscript. I. Pulitani: data acquisition, review of the manuscript. S. Cánovas: data acquisition, review of the manuscript. A. Ferreiro: data acquisition, review of the manuscript. A. García-Valentín: data acquisition, review of the manuscript. M. Carnero: data acquisition, review of the manuscript. P. Pareja: data acquisition, review of the manuscript. J.A. Corrales: data acquisition, review of the manuscript. J.A. Blázquez: data acquisition, review of the manuscript. D. Macías: data acquisition, review of the manuscript. D. Fletcher-Sanfeliu: data acquisition, review of the manuscript. D. Martínez: data acquisition, review of the manuscript. E. Martín: data acquisition, review of the manuscript. M. Martín: data acquisition, review of the manuscript. J. Margarit: data acquisition, review of the manuscript. R. Hernández-Estefanía: data acquisition, review of the manuscript. E. Monguió: data acquisition, review of the manuscript. J. Otero: data acquisition, review of the manuscript. J. Silva: data interpretation of data, drafting and review of the manuscript.
All authors approve the final version
All authors agree to be responsible for all aspects of the work and warrant that all questions regarding accuracy or completeness have been properly investigated and resolved.
D. Hernández-Vaquero and E. Rodríguez-Caulo contributed equally to this study.
CONFLICTS OF INTERESTNone.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2021.04.010