There are no in-depth studies of the long-term outcome of patients with syncope after exclusion of cardiac etiology. We therefore analyzed the long-term outcome of this population.
MethodsFor 147 months, we included all patients with syncope referred to our syncope unit after exclusion of a cardiac cause.
ResultsWe included 589 consecutive patients. There were 313 (53.1%) women, and the median age was 52 [34-66] years. Of these, 405 (68.8%) were diagnosed with vasovagal syncope (VVS), 65 (11%) with orthostatic hypotension syncope (OHS), and 119 (20.2%) with syncope of unknown etiology (SUE). During a median follow-up of 52 [28-89] months, 220 (37.4%) had recurrences (21.7% ≥ 2 recurrences), and 39 died (6.6%). Syncope recurred in 41% of patients with VVS, 35.4% with OHS, and 25.2% with SUE (P=.006). In the Cox multivariate analysis, recurrence was correlated with age (P=.002), female sex (P <.0001), and the number of previous episodes (< 5 vs ≥ 5; P <.0001). Death occurred in 15 (3.5%) patients with VVS, 11 (16.9%) with OHS, and 13 (10.9%) with SUE (P=.001). In the multivariate analysis, death was associated with age (P=.0001), diabetes (P=.007), and diagnosis of OHS (P=.026) and SUE (P=.020).
ConclusionsIn patients with noncardiac syncope, the recurrence rate after 52 months of follow-up was 37.4% and mortality was 6.6% per year. Recurrence was higher in patients with a neuromedial profile and mortality was higher in patients with a nonneuromedial profile.
Keywords
Syncope is a symptom that generates substantial health care resource use. The most common mechanisms are reflex syncope, which includes vasovagal syncope (VVS), and orthostatic hypotension syncope (OHS), which is more common in older patients.1,2 Recurrence of syncope in general is reported in one third of patients at 3 years, the same as in the population with VVS, but the recurrence of OHS is not well described.2–4 Treatment of the patient with syncope is based on the etiology. When the etiology is cardiac, the treatment is usually aimed at the specific cause (that is, bradyarrhythmia or tachyarrhythmia). However, the specific treatment for noncardiac etiology is usually determined by the frequency of the syncopal episodes and their impact on the patient's quality of life.4–6
The published probability of death in the population with VVS has generally been low, comparable to that of the general population4,5; some studies do not even report it,7 but it differs depending on the population studied.5,8,9
We hypothesized that the recurrence rate and mortality in patients with syncope of noncardiac cause would differ according to the etiology, whether orthostatic hypotension or syncope of unknown etiology (SUE). The aim of this study was to describe, in patients who experience syncope, recurrence of syncope and mortality, dividing patients into these 3 etiological categories according to the European Society of Cardiology criteria (), in a cohort of patients assessed in the syncope unit of a single center, after exclusion of a cardiac cause.
METHODSInclusion criteriaIn a prospective registry that included all consecutive patients referred to our syncope unit, we have previously described the diagnostic tests performed to exclude a cardiac cause.10 All the patients included in this study had a previous syncope. In the syncope unit of our hospital, we use a standardized protocol following the recommendations in the European guidelines on syncope.1,2,11 Patient enrolment started on April 1, 2006 and ended on January 31, 2018.
With the aim of achieving as close a follow-up as possible in these 1058 patients, for this retrospective analysis we included only those patients referred to our unit who were resident in our health care area. Cardiac etiology was always excluded by the patient's treating physician using the standard diagnostic tests that they considered necessary (that is, echocardiography, stress testing, perfusion imaging, electrophysiology study, coronary angiography, or implantable Holter). All tests were reviewed in the unit and have been reported previously.10 The patients were then referred to our unit for further assessment including a head-up tilt test (). All patients gave written informed consent. As this was a registry and not an interventional study, we did not request hospital ethics committee approval.
Follow-upTo ensure that follow-up would be at least 6 months in all patients, follow-up started on April 1, 2006 and ended on July 31, 2018. A prespecified protocol was used for clinic follow-up visits, telephone calls, and review of electronic medical records: all patients had at least 1 clinic visit and annual telephone follow-up. In all patients, the data recorded at each follow-up visit included: presence or absence of recurrence and date, number of recurrences, death and its cause, injuries, need for device-based treatment, hospital admissions, and emergency department visits. The electronic medical records in our public health system helped achieve and complete 100% adherence to follow-up, as we were able to check the visits to the emergency department if the patient told us about them in clinic or over the phone. For patients who died at home or of an unknown cause, we contacted their families to assess the probability of sudden cardiac death.
Statistical analysisQualitative variables are presented as absolute and relative frequencies, and quantitative variables are presented as mean ±standard deviation or median [interquartile range] depending on the distribution of the variable, evaluated using the Kolmogorov-Smirnov test. Qualitative variables were compared using the chi-square test or Fisher exact test, and quantitative variables were compared using the Student t test, Mann-Whitney test, or Kruskal-Wallis test, as appropriate. To assess the event-free survival time (recurrent syncope, death), Kaplan-Meier survival analysis using the log-rank test (Mantel-Cox) was used to compare the different groups classified according to the final diagnosis reached in the unit, which was that used for follow-up analysis. The time was calculated from the date the patient was seen in the syncope unit until the date of the first recurrence. Cox proportional hazards regression models were used to analyze the risk of recurrence of syncope and of death within each specific etiology (1, VVS; 2, OHS; 3, SUE). All clinical variables were included to assess their possible relationship with outcome. Receiver operating characteristic (ROC) curve analysis was used to predict syncope recurrence as an outcome. Analysis was performed using the SPSS V24.0 program. P values < .05 were considered statistically significant.
RESULTSFrom April 1, 2006 to July 31, 2018, 1058 patients were assessed, but the analysis included only 589 patients who were resident in our health care area. Of them, 313 (53.1%) were women, with a mean age of 52 [34-66] years. The patients had had 4 [2-10] syncopal episodes before the start of the study, with a time since first syncope of 36 [12-120] months. The final diagnosis was VVS in 69%, OHS in 11%, and SUE in 20.2% of cases. There was a difference in etiology by age (P=.0001) and sex (P = .008) (table 1).
Clinical characteristics of the 589 patients by sex, final etiological diagnosis, recurrence, and mortality.
| Men276 (46.9) | Women313 (53.1) | P | VVS405 | OHS65 | SUE119 | P | Patients withrecurrence of syncope220 (37.4) | Patients withoutrecurrence of syncope369 (62.6) | P | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age, y | 52 [35-66] | 52 [34-66] | .92 | 49 [31-63] | 64 [48-73] | 55 [38-68] | .0001 | 50 [35-66] | 53 [33-65] | .85 |
| Men | 173 (62.7) | 39 (14.1) | 64 (23.2) | .008 | ||||||
| Women | 232 (74.1) | 26 (8.3) | 55 (17.6) | |||||||
| Hypertension | 65 (23.6) | 82 (26.2) | .45 | 88 (21.7) | 23 (35.4) | 36 (30.3) | .02 | 90 (24.4) | 57 (25.9) | .68 |
| Diabetes | 37 (13.4) | 17 (5.4) | .001 | 30 (7.4) | 10 (15.4) | 14 (11.8) | .06 | 34 (9.2) | 20 (9.1) | .96 |
| Atrial fibrillation | 4 (1.4) | 8 (2.6) | .34 | 6 (1.5) | 5 (7.7) | 1 (0.8) | .003 | 7 (1.9) | 5 (2.3) | .48 |
| Number of previous syncopal episodes | 3 [1-6] | 5 [2-11] | .0001 | 4 [2-10] | 3 [1-5] | 3 [1-6] | .0001 | 5.5 [3-11.5] | 3 [1-6] | .0001 |
| Time since first syncope, months | 24 [9-96] | 36 [12-180] | .018 | 48 [12-180] | 18 [6-36] | 14 [6-48] | .0001 | 48 [12.5-180] | 24 [9-96] | .0001 |
| Recurrence of syncope | ||||||||||
| Patients with recurrence | 84 (30.4) | 136 (43.5) | .001 | 167 (41.2) | 23 (35.4) | 30 (25.2) | .006 | |||
| Number of syncopal episodes | 0 [0-2] | 0 [0-1] | .0001 | 0 [0-2] | 0 [0-1] | 0 [0-1] | .001 | |||
| Recurrence-free time, months | 78.8 (83.2-101.6) | 84.3 (72.8-95.7) | 92.4 (83.2-101.6) | .04 | ||||||
| Mortality | ||||||||||
| Number of deaths | 22 (8) | 17 (5.4) | .25 | 15 (3.7) | 11 (16.9) | 13 (10.9) | .001 | |||
| Number of events | 0 [0-2] | 0 [0-1] | .0001 | 0 [0-2] | 0 [0-1] | 0 [0-1] | .001 | |||
| Mortality-free survival, months | 121 (118.4-123.5) | 102.32 (91.9-112.5) | 108.7 (101-116.2) | .0001 | ||||||
OHS, orthostatic hypotension syncope; SUE, syncope of unknown etiology; VVS, vasovagal syncope.
Values are presented as No. (%), mean±standard deviation, or median [interquartile range]. P values <.05 were considered statistically significant.
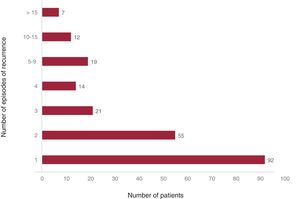
We were able to complete 100% follow-up of the population. After a median follow-up of 52 [28-89] months, 220 patients (37.4%) had at least 1 recurrence of syncope, with a time to first recurrence of 46 [21-82] months. The median number of recurrences was 2 [1-3]. The annual cumulative probability of recurrence was 8.7%. In 42% of the patients who had recurrence, the recurrence was an isolated episode, while the other 58% had 2 or more episodes of recurrence (figure 1). The cumulative probability of syncope recurrence was higher in women than in men (P = .001), and women also had a higher number of recurrences (P=.0001) (table 1).
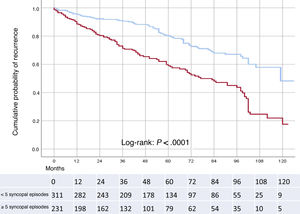
The recurrence-free survival for the 220 patients who had recurrence was 82.2 (95% confidence interval [95%CI], 78-86.4) months. We identified different cutoff values for prediction of recurrence. According to the ROC analysis, 5 previous episodes gave the best sensitivity (0.605) and specificity (0.661), with an area under the curve of 67.2%±0.2%. The cumulative probability of recurrence was lower in patients with fewer than 5 episodes than in those with 5 or more previous episodes: 26.3% vs 51.6% (P=.0001) (figure 2).
Cumulative probability of recurrence in patients with fewer than 5 previous syncopal episodes (blue line), syncope-free survival time, 94.3 (95%CI, 89-99.6) months, compared with those with 5 or more (red line), syncope-free survival time, 67.2 (95%CI, 61.2-73.2) months (log-rank test,P <.0001). 95%CI, 95% confidence interval.
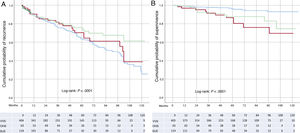
The number of patients with recurrence of syncope was higher in the VVS group than in the OHS or SUE groups (P=.006). There were also differences in the number of recurrences of syncope depending on the etiology (P=.001) and in recurrence-free survival time (log-rank test,P <.001) (table 1, figure 3A). Factors identified as independent variables associated with recurrence of syncope were age (hazard ratio [HR],0.65; 95%CI, 0.49-0.86; P=.002), female sex (HR,2.81; 95%CI, 1.9-3.9; P <.0001) and the number of previous episodes (< 5 vs ≥ 5, HR,2.98; 95%CI, 2.1-4.2; P <.0001).
A: cumulative probability of recurrence of syncope in patients with VVS, syncope-free survival time, 78.8 (95%CI, 73.9-83.4) months (blue), compared with those with OHS, syncope-free survival time, 84.3 (95%CI, 72.8-95.7) months (red) and SUE, syncope-free survival time, 92.4; (95%CI, 83.2-101.6) months (green) (log-rank test, P <.001), B: cumulative probability of mortality in patients with VVS, mortality-free survival time, 121 (95%CI, 118.4-123.5) months (blue) compared with those with OHS, mortality-free survival time, 102.32 (95%CI, 91.9-112.5) months (red) and SUE, 108.7 (95%CI,101.2-116.2) months (green) (log-rank test, P <.0001). 95%CI, 95% confidence interval; OHS, orthopedic hypotension syncope; SUE, syncope of unknown etiology; VVS, vasovagal syncope.
There were 39 deaths (6.6%), with an annual cumulative probability of death of 1.53%, with no differences between men and women (P=.25). Only 4 deaths were due to cardiovascular causes and none were sudden cardiac death. There was a significant difference in age between those who died and those who survived (P <.0001). Patients who died had a higher cumulative probability of hypertension (P=.021) and diabetes (P=.0001); however, they had fewer recurrences of syncope (P=.004) (table 2). Patients with recurrence of syncope had a lower cumulative probability of death (P=.004), and age and diabetes were associated with mortality (table 3).
Causes of death in the study population
| VVS, n | OHS, n | SUE, n | |
|---|---|---|---|
| Cause of death | |||
| Cardiovascular | 1 | 2 | 1 |
| Noncardiovascular | 14 | 9 | 12 |
| Cancer | 6 | 2 | 4 |
| Sepsis | 1 | 1 | 2 |
| Respiratory infection | 1 | 1 | 2 |
| Suicide | 2 | 0 | 0 |
| Idiopathic pulmonary fibrosis | 1 | 0 | 0 |
| Myelodysplasia | 1 | 1 | 0 |
| Distal necrosis of the foot | 0 | 1 | 0 |
| Acute gastroenteritis | 0 | 0 | 0 |
| Acute pancreatitis | 0 | 0 | 1 |
| Peptic ulcer | 0 | 0 | 1 |
| Unknown | 2 | 2 | 2 |
OHS, orthostatic hypotension syncope; SUE, syncope of unknown etiology; VVS, vasovagal syncope.
Clinical characteristics according to mortality during follow-up. Univariate and multivariate analysis between characteristics and mortality
| Survivors (n=550) | Nonsurvivors (n=39) | P | HR (95%CI) | P | HR (95%CI) | P | |
|---|---|---|---|---|---|---|---|
| Age, y | 50 [33-64] | 71 [59-79] | .0001 | 1.075 (1.048-1.103) | .0001 | 1.062 (1.034-1.090) | .0001 |
| Male sex | 254 (46.2) | 22 (56.4) | .25 | 0.728 (0.387-1.372) | .326 | ||
| Hypertension | 132 (24) | 15 (38.5) | .021 | 2.146 (1.123-4.101) | .021 | 0.546 (0.263-1.130) | .100 |
| Diabetes | 42 (7.6) | 12 (30.8) | .0001 | 6.536 (3.260-13.103) | .0001 | 2.683 (1.309-5.500) | .007 |
| Atrial fibrillation | 10 (1.8) | 2 (5.1) | .147 | 3.663 (0.881-15.231) | .074 | ||
| Number of previous syncopal episodes | 4 [2-8] | 5 [2-15] | .31 | 1.004 (0.989-1.020) | .566 | ||
| Time since first syncope, months | 36 [12-120] | 24 [6-60] | .16 | 1.000 (0.997-1.002) | .730 | ||
| Recurrence of syncope | 214 (38.8) | 6 (15.8) | .004 | ||||
| Final diagnosis of OHS | 54 (9.8) | 11 (28.2) | 4.440 (2.038-9.672) | .0001 | 2.466 (1.113-5.465) | .026 | |
| Final diagnosis of SUE | 106 (19.3) | 13 (19.3) | 3.071 (1.460-6.462) | .003 | 2.419 (1.147-5.105) | .020 |
95%CI, 95% confidence interval; HR, hazard ratio; OHS, orthostatic hypotension syncope; SUE, syncope of unknown etiology.
Values are presented as No. (%), mean±standard deviation, or median [interquartile range]. P values <.05 were considered statistically significant.
The median time until death was 51 [27-85] months, with no differences between men and women (P=.19). Survival time was 117 (95%CI, 114.2-119.7) months. When analyzed by etiology, there were differences in mortality (P=.0001) and event (death)-free survival (log-rank test [Mantel-Cox], P <.0001) (table 1, figure 3B). On multivariate analysis, the diagnoses of OHS and SUE were identified as independent markers associated with mortality (table 3).
DISCUSSIONThe main findings from our study are the following: a) patients with syncope of noncardiac etiology encompass 3 different populations: VVS, OHS, and SUE; b) recurrence of syncope is common and is correlated with clinical factors; c) the cumulative probability of death differs depending on the etiology; and d) these patients should be assessed in specialized units.
In line with our results, a higher prevalence of noncardiogenic syncope has been reported in women, particularly if the etiology is VVS.4,5,7,12 Sex also influences the time to recurrence of syncope and the occurrence of repeat events. However, implantable Holter monitoring would have provided more information to help determine the etiology, especially in patients with SUE.
Previously, age has been reported as being associated with etiology and recurrence of syncope7,13; however, our previous experience has demonstrated that age is not associated.4 The age of patients with VVS is similar to that previously described by our group and others.4,7 Of note, in our series we found a significant difference in age between patients with VVS (younger) and patients with OHS and SUE.
The role of conventional risk factors and their effect on recurrence of syncope is not well established. In our series, the prevalence of diabetes was higher in men than in women, although we also observed age differences between the 3 etiological groups. The prevalence of diabetes in men was similar to that described previously (12.39%)12; however, the Framingham study showed a much lower prevalence of diabetes in the total population with syncope (6.2%) and patients with VVS (4.4%) and SUE (4.4%).5 There may be various reasons for this discrepancy and they may be related to the fact that the Framingham study was published several decades ago and the prevalence of diabetes in the general population has increased since then.14
Recurrence of syncopeThe annual syncope recurrence rate was 8.7% over a follow-up of 4.3 years, and recurrences occurred in 37.4% of the patients; 76.6% of these recurrences occurred in patients with VVS and OHS, findings that are similar to those published by other authors,4,15,16 although it is important to note that our population had a high cumulative probability of syncope recurrence and, therefore, was very symptomatic. This is in contrast to the population cohort with syncope in the Framingham study, who had a much lower cumulative probability of recurrence, of 21.6% or 1.27% per year after a mean follow-up of 17 years. In addition, it was reported that 17.6% of patients with recurrence had only 1 episode of recurrence and only 4% had more than 1.5 The recurrence-free survival time in the 220 patients who had recurrence was certainly long, at 82.2 (95%CI, 78-86.4) months. In previous studies by our group this time was shorter, at 50.1 (95%CI, 46-54) months, but the data related to the whole population included in the study, not only those with recurrence.4
The number of syncope recurrences was higher than that previously reported by other investigators, albeit with shorter follow-up times.7 Our findings indicate that one third of the patients sent for further assessment for syncope may need targeted therapies to avoid recurrence, and we believe that future research in this field should be encouraged.
Past syncope burden has been identified in other studies as a marker of future recurrence.4,6,17 In our population, having 5 or more syncopal episodes prior to inclusion in the registry was independently associated with recurrence. Another interesting factor associated with recurrences during follow-up was sex, as confirmed by other authors.4,6,16,18 In our series, women had a higher cumulative probability of recurrence and a risk of recurrence 3 times higher than that of men.
MortalityWe found slightly higher mortality in men, driven mainly by noncardiac causes. The reasons for this finding remain undetermined. However, it is plausible that syncope, especially if it is recurrent and not of vasovagal etiology, may simply be a marker of frailty that identifies older patients with multiple comorbidities who are at risk of mortality from all causes. The low mortality and inverse association between recurrence of syncope and mortality would suggest that the relationship between syncope and mortality should be established with caution. Few studies have analyzed the cumulative probability of mortality in outpatients with noncardiogenic syncope who have not been admitted to hospital. Yasa et al.8 analyzed a prospective cohort based on a population of 30 528 middle-aged individuals who were discharged with a diagnosis of unexplained syncope or OHS, although they had a higher incidence of cardiovascular disease and mortality. It should be noted that this population, although they were the same age (62±7 vs 63±7 years), had been admitted to hospital for syncope. In a series of patients with orthostatic hypotension, Naschitz et al.19 reported a higher risk of death probably related to the severity of comorbidities, which was double that of the total study population. However, this association has not been reflected in other studies.5,20 In VVS, a lower mortality was found, which is in line with previous publications and supports the clinical observation included in the European guidelines that recurrent episodes are a marker of benign outcome.1,2,9
The role of age in mortality has previously been described in patients with syncope of different etiologies, but not specifically in patients with noncardiogenic syncope.21 Diabetes was independently associated with mortality in a study of patients admitted to hospital due to syncope; over a follow-up of 27 months, the cumulative probability of mortality was 12% and the factors independently associated with mortality were diabetes (HR,2.7; 95%CI, 1.4-5.2), smoking (HR,2.8; 95%CI, 1.4-5.5), and atrial fibrillation (HR,2.4; 95%CI, 1.9-5.4).19 Our finding is in agreement with a univariate meta-analysis that reported that the effect of noncardiac or unexplained syncope on mortality increases with age and prevalence of diabetes and hypertension.9
Finally, SUE was independently associated with mortality, as Ungar et al.20 already described in patients admitted to hospital for syncope (odds ratio [OR],4.6; 95%CI, 1.002-21.727; P <.059). In a population-based study, Sule et al.22 also reported the diagnosis of SUE as an independent predictor of mortality (HR,1.32; 95%CI, 1.09-1.60; P <.01). Likewise, in our study, OHS had a higher cumulative probability of mortality, an increase of almost 3 times that with VVS; this association was previously described by Masaki et al.,23 who reported a high mortality in the population with OHS and proposed the frailty of this population as driving the possible relationship with mortality. While it is true that the association between SUE and OHS with mortality may not be causal, it could be a marker (more than a factor) of risk of general (not cardiac) mortality. A study more in line with this objective should be designed to properly evaluate this.
Perhaps the most important conclusion from our descriptive study comprising 12 years of patient inclusion is that it has demonstrated the usefulness of syncope units—extremely common in other countries—for the assessment and management of this population, yet there are few in Spain. The very low cardiac mortality observed demonstrates that the initial diagnostic workup aimed at excluding cardiac syncope was appropriate, highlighting the importance of a good initial assessment and the enormous usefulness of these units.
LimitationsOur study has several limitations: one is the prospective inclusion of all consecutive patients referred to our syncope unit, which indicates a potential selection bias. The inclusion period from 2006 to 2018 introduces an obvious limitation, as during these 12 years there have been substantial changes in the diagnostic workup of patients with syncope. The data analysis was retrospective. This was a single-center study of a sample selected from patients sent to a syncope unit after exclusion of a potential cardiac cause. Another limitation or bias is having selected only the population pertaining to our health care area. It would have been of great interest to include a series of patients with similar characteristics without a history of syncope to compare the outcomes. The diagnosis of cardiac syncope had been excluded through clinical assessment and diagnostic tests performed by the patients’ physicians before they were referred to the syncope unit, so the group will certainly not be homogeneous in terms of the tests performed or their interpretation in the specialized syncope unit. The reproducibility of the head-up tilt test has been questioned, but it is in line with our previous publications and the European guidelines on syncope. An area under the curve of 0.67 with the cutoff of 5 episodes of syncope must be recognized as relatively low. We tried to judge the cause of unknown deaths, but we cannot rule out the possibility of underestimating sudden cardiac deaths. We believe that the use of an implantable Holter monitor in our population with SUE could have improved the identification of the cause of syncope; however, 92.5% had a normal ECG and 95% had no evidence of structural heart disease, so an implantable Holter monitor was probably not indicated in most of them and would have offered very little added benefit to the diagnosis.
In a survey carried out in 2015 on hospitals in the USA, Kachalia et al.24 describe that 83% of patients with syncope underwent an excessive number of diagnostic tests. The excessive use of medical resources for patients with low-risk syncope is increasingly recognized as a problem.25 The findings of our study are applicable to patients referred for further assessment of unexplained syncope to an experienced syncope unit, and may or may not reflect the situation of a population of outpatients seeking medical advice following syncope.
CONCLUSIONSNoncardiac syncope, particularly reflex syncope, has an annual cumulative probability of recurrence of approximately 9%. Recurrence is higher in those with neurally-mediated profiles (young women with many previous syncopal episodes). Mortality in this population is mainly due to noncardiovascular causes and is associated with a nonneurally-mediated profile (older, diabetic, and due to orthostatic hypotension or unknown cause). Syncope units are extremely useful for studying this population.
- –
There are few studies on the long-term outcomes in patients admitted to hospital for syncope, and very few have analyzed the outcomes in patients with syncope not requiring hospital admission. Noncardiac syncope generates frequent medical visits and high resource use. Specific treatment for this population remains a subject of debate.
- –
The cumulative probability of syncope recurrence is crucial to identify patients with a diagnosis of syncope who will need specific treatment.
- –
There have been few studies on the long-term mortality of the population with low-risk or noncardiac syncope and with discordant results.
- –
The population with noncardiac syncope is sometimes described as low risk in general; in our experience, the long-term risk can be determined by different etiologies.
- –
In a long-term prospective study with 100% follow-up in a tertiary hospital, patients with syncope of noncardiac etiology had a considerable cumulative probability of recurrence and high mortality, both associated with clinical variables.
- –
The high cumulative probability of recurrence and mortality found was associated with the etiology of the syncope, with significant differences between vasovagal syncope, syncope due to orthostatic hypotension and syncope of unknown etiology.
- –
Our findings require confirmation in clinical studies designed for this population. More syncope units should be established.
This study did not receive any specific funding from public, private, or nonprofit agencies.
AUTHORS’ CONTRIBUTIONSAll the authors actively participated in the study: G. Barón-Esquivias, A.J. Díaz-Martín, M. Quintanilla, C. García-Romero, I. Paneque, C. Rubio-Guerrero, R. Rodríguez-Corredor and J.I. Valle-Racero assessed all the patients in the syncope unit and, together with the other authors, analyzed and interpreted the data and wrote the manuscript. C.V. Almeida-González, A. Ordóñez, C.A. Morillo, C. Barón-Solís and G. Barón-Esquivias performed the statistical analysis. All authors have approved the results and the final version of the manuscript.
CONFLICTS OF INTERESTThere are no industry links. There are no conflicts of interest between the authors and this study.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.recesp.2021.10.003